


The article titled "10 Essential Clinical Trial Diversity Metrics for Better Outcomes" tackles a critical question: how can we effectively measure and enhance diversity in clinical trials to achieve superior health outcomes? This inquiry is not just relevant; it is essential for the future of clinical research. By employing specific diversity metrics—such as age, race, and gender—we can ensure representative participation. This, in turn, enhances the generalizability and effectiveness of clinical research findings, ultimately leading to improved healthcare solutions for diverse populations.
In the Medtech landscape, the role of diversity metrics cannot be overstated. They serve as a foundation for addressing key challenges in clinical trials, ensuring that all segments of the population are represented. This representation is vital for the development of treatments that are effective across different demographics. As we consider our own challenges in clinical research, it becomes clear that the integration of these metrics is not merely beneficial but necessary.
In conclusion, the importance of collaboration in this endeavor cannot be overlooked. By working together to implement these diversity metrics, we can pave the way for more inclusive and effective clinical trials. The next steps involve not only recognizing the significance of these metrics but also taking decisive action to incorporate them into our research practices.
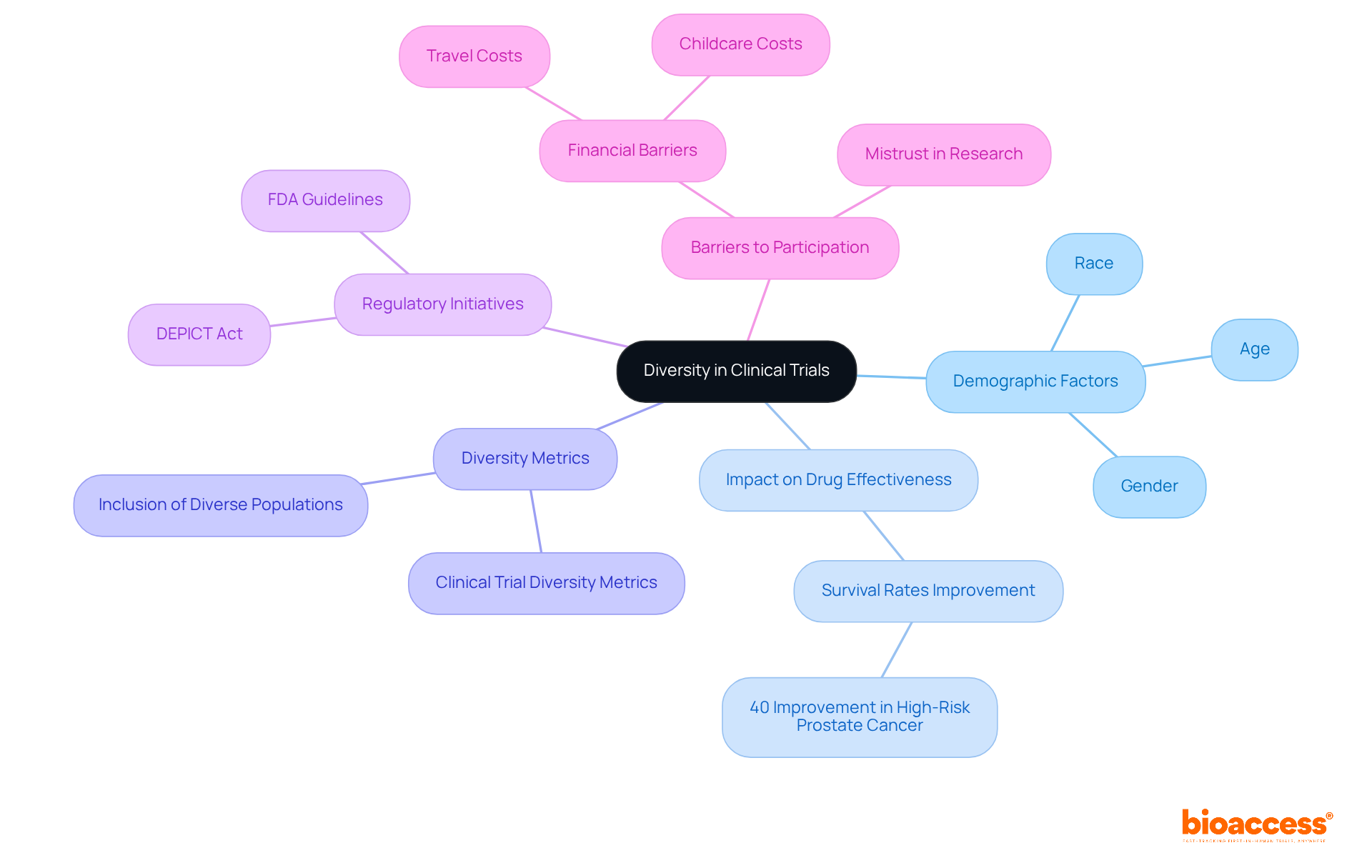
In the realm of clinical research, the significance of diversity cannot be overstated. Studies increasingly reveal that demographic factors such as age, race, and gender profoundly influence treatment outcomes. This reality underscores the paramount need for comprehensive clinical trial diversity metrics.
This article delves into ten essential metrics that not only highlight the importance of diverse participant representation but also explore how these metrics can lead to improved health outcomes and greater generalizability of research findings.
Yet, a pressing challenge remains: how can stakeholders effectively overcome barriers to ensure that clinical trials are inclusive and reflective of the populations they aim to serve?
bioaccess® leverages the regulatory efficiency of Latin America, the diverse participant groups of the Balkans, and streamlined processes in Australia to enhance research diversity. This strategic combination facilitates ethical approvals within just 4-6 weeks and accelerates enrollment by 50% compared to traditional markets. By prioritizing diverse groups, bioaccess® not only improves representation in studies but also enhances health outcomes and the generalizability of findings, as reflected in clinical trial diversity metrics. The inclusion of varied demographics is essential, as research indicates that clinical trial diversity metrics can significantly influence treatment efficacy and safety across different populations.
Successful medical studies, such as Early-Feasibility Studies and First-In-Human Studies in the Balkans, exemplify this approach, demonstrating that engaging with varied participant groups yields more robust data and improved healthcare solutions. With bioaccess®'s comprehensive research study management services—including feasibility studies, site selection, compliance reviews, and project management—clients can effectively navigate the complexities of studies while achieving savings of $25K per individual. As Dr. Kelly Herremans aptly states, "If the research study doesn’t encompass representation of diverse patients, we can’t - and shouldn’t - anticipate that the results will be applicable to all patient demographics, which underscores the need for clinical trial diversity metrics."
In the evolving Medtech landscape, collaboration is key. By working together, stakeholders can address the challenges of clinical research and ensure that findings are relevant and beneficial to all populations.

Understanding the variety in research studies is essential for comprehensively grasping how demographic factors—like age, race, and gender—impact drug effectiveness and safety. Research shows that variability in drug response can lead to significant disparities in treatment outcomes. For instance, a recent study revealed that survival rates for high-risk prostate cancer improved by 40% with a specific drug combination. This underscores the importance of including diverse populations in research to enhance clinical trial diversity metrics. By ensuring representation from various demographic groups, studies can tailor treatments to better meet the needs of all patients, ultimately enhancing patient care and promoting health equity.
Moreover, initiatives such as the DEPICT Act mandate diversity action plans in research designs, which are essential for improving clinical trial diversity metrics and reflect a growing recognition of the need for inclusive research practices. This approach not only addresses historical disparities but also builds trust within underrepresented communities, paving the way for more effective and equitable healthcare solutions. Additionally, the FDA advises that sponsors justify the inclusion or exclusion of specific populations in investigational new drug applications, highlighting the critical need for clinical trial diversity metrics to ensure diverse representation.
It's also vital to acknowledge the financial barriers that significantly impact participation in research studies, particularly for individuals with low socioeconomic status. Addressing these challenges is crucial for achieving genuine diversity in clinical research.
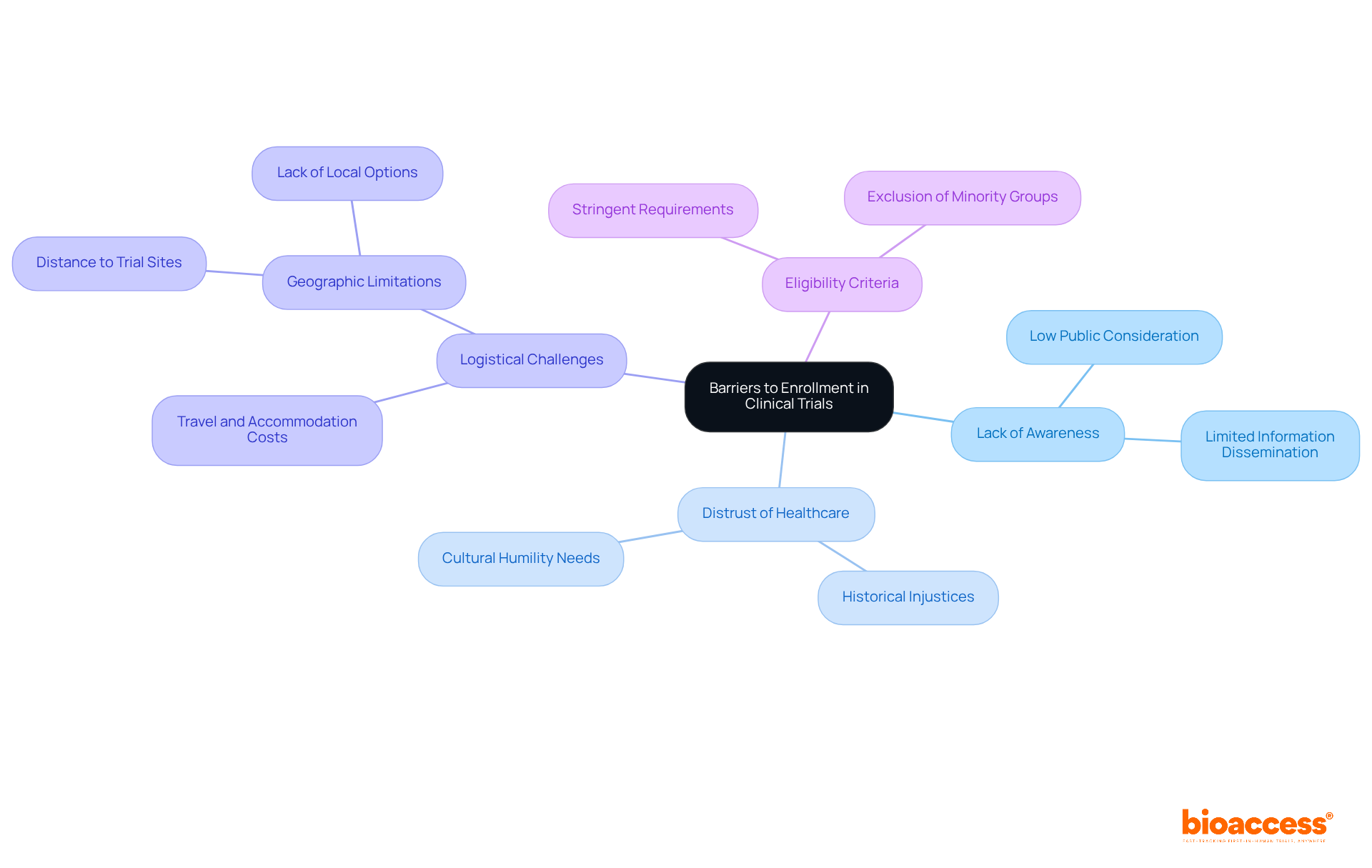
Obstacles to participation in research studies are multifaceted, encompassing:
Socioeconomic factors and cultural differences further complicate participation, particularly for underrepresented groups. Research indicates that historical injustices have fostered distrust, with 55% of individuals citing personal expenses as a significant factor influencing their decision-making. Financial hurdles present a major barrier, particularly for minority groups seeking to engage in research studies.
Moreover, geographic limitations often restrict access to these studies. More than half of U.S. cancer patients lack local alternatives, and nearly 50% of individuals with prevalent metastatic cancers must travel over an hour to reach a study site. Addressing these obstacles is crucial. For instance, implementing decentralized studies can mitigate geographic challenges by leveraging telemedicine, local laboratories, and home health services to bring the study directly to the patient.
Additionally, fostering cultural humility and acknowledging past injustices are vital steps in rebuilding trust within communities. By recognizing and understanding these barriers, stakeholders can devise effective strategies to enhance clinical trial diversity metrics, thus ensuring equitable access for all groups and improving the reliability of research outcomes.
To enhance participation in clinical trials, organizations can adopt several effective strategies:
Engage with Community Leaders: Building trust within communities is crucial. As noted by the FDA, "Engaging local leaders and health advocates can help build trust and improve recruitment rates in underserved communities." Collaborating with local leaders and health advocates can significantly improve recruitment rates among underrepresented groups. The recent partnership between bioaccess™ and Caribbean Health Group illustrates this method, as they collaborate to establish Barranquilla as a premier location for medical studies in Latin America, with backing from Colombia's Minister of Health.
Simplify Legal Procedures: Streamlining legal processes and minimizing in-person visit requirements can alleviate logistical burdens, making participation more accessible.
Utilize Technology for Remote Participation: Leveraging digital health tools allows for remote engagement, which can help overcome geographic and temporal barriers. This method has been demonstrated to improve participant experience and boost diversity in research studies. However, it is essential to address digital literacy concerns, ensuring that educational materials are accessible to individuals with varying levels of digital skills.
Provide Education About the Legal Process: Offering clear, culturally relevant educational materials can demystify the legal process and encourage participation. Ensuring that information is accessible to individuals with varying levels of digital literacy is essential.
Offer Financial Incentives: Providing financial support for participation can address economic barriers, making it easier for individuals from diverse backgrounds to take part in research studies. The collaboration between GlobalCare Clinical Trials and bioaccess™ aims to improve ambulatory services for research in Colombia, achieving over a 50% reduction in recruitment time and 95% retention rates, showcasing the effectiveness of such strategies.
By implementing these strategies, organizations can effectively overcome barriers to participation and improve clinical trial diversity metrics, ultimately leading to more generalizable and impactful research outcomes. Furthermore, referencing the FDA's 27-point action plan aimed at enhancing participation of women, minorities, and older adults in research studies can offer a current framework that supports these strategies.

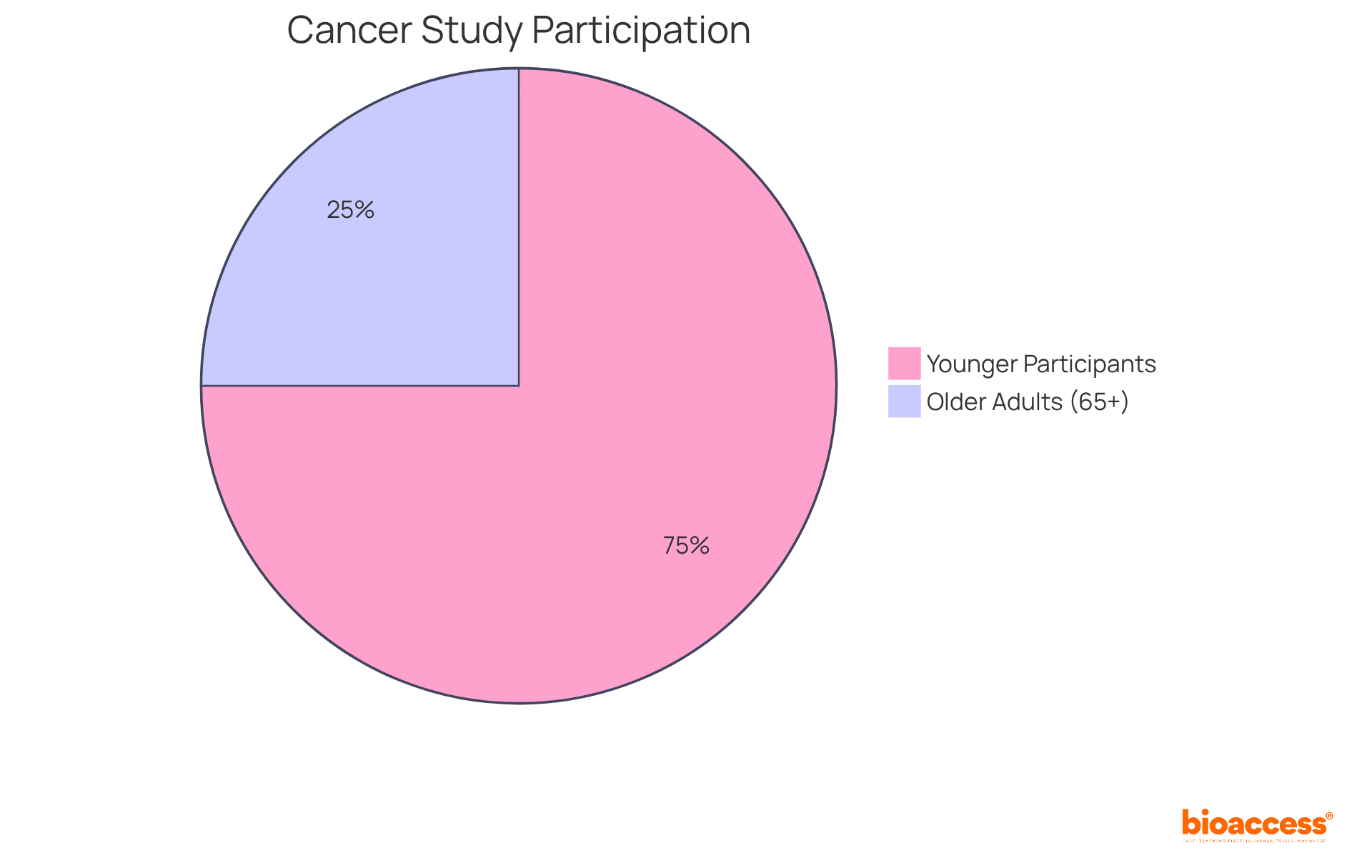
Incorporating age diversity in research studies is essential for understanding how treatments perform across different life stages. Older adults often display unique physiological responses to medications, which can significantly affect treatment outcomes. For instance, research indicates that older patients, who represent a substantial portion of chronic disease cases, may respond differently to treatments compared to younger populations. By systematically tracking age as a vital metric, researchers can ensure that clinical trial diversity metrics accurately represent the demographics of those affected by the conditions under investigation. This method not only improves the safety and effectiveness of treatments but also promotes health equity by addressing the specific needs of all age groups.
Current data reveals a concerning trend: the participation of older adults in research studies is alarmingly low, with only 25% of cancer-focused study participants aged 65 and older, despite this demographic accounting for over half of all cancer diagnoses. This stark statistic raises an important question: how can we enhance the inclusivity of clinical research?
Prioritizing age diversity in recruitment strategies is crucial for generating research findings that are relevant and beneficial to the entire population. By taking action now, we can ensure that all age groups are represented, ultimately leading to more effective and equitable healthcare solutions.
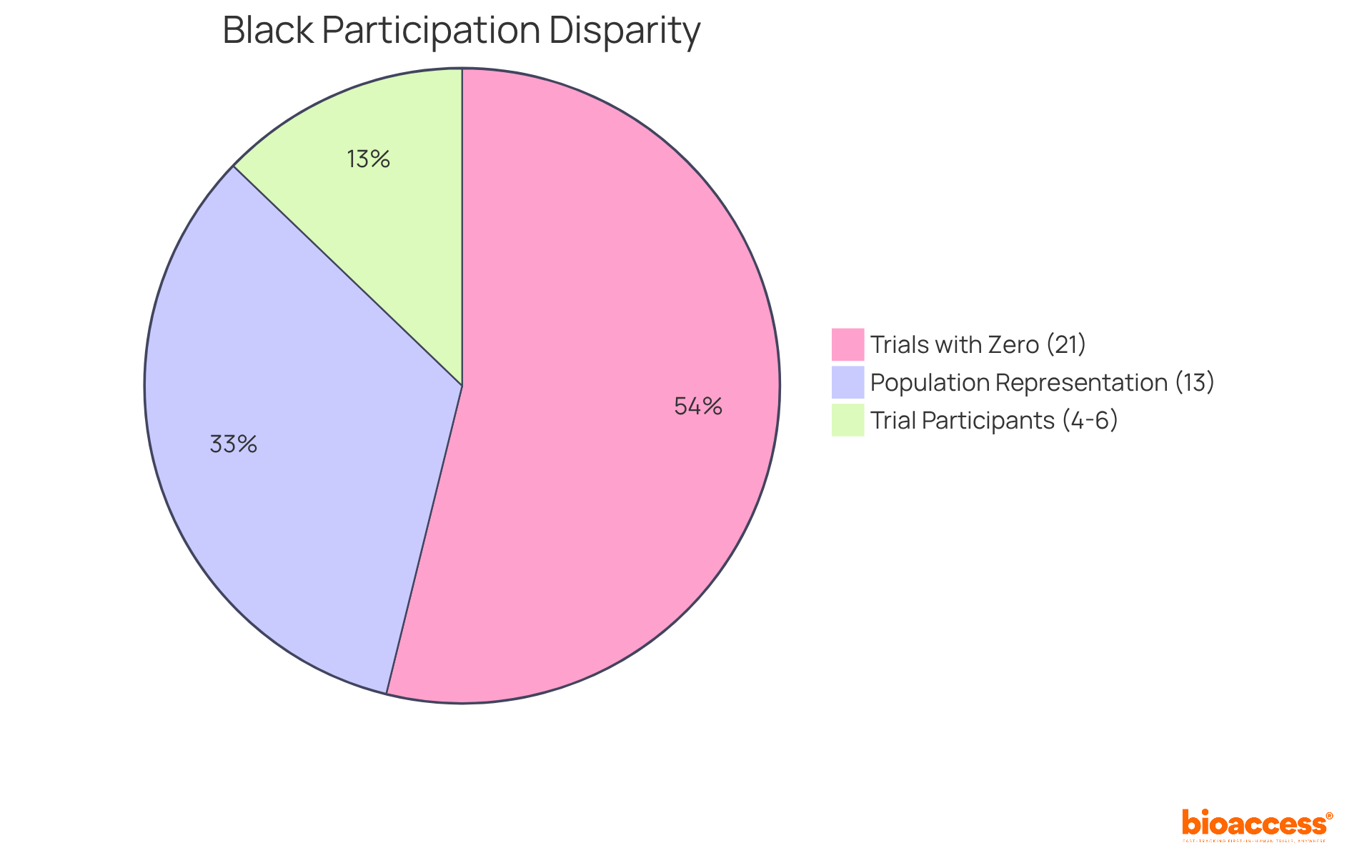
Race and ethnicity serve as crucial indicators for assessing diversity in research studies, encompassing unique genetic, environmental, and lifestyle factors that significantly influence treatment outcomes. Recent studies reveal notable differences in treatment effectiveness among various racial groups, underscoring the urgent need for tailored strategies in medical research. For instance, research shows that Black participants constituted only 4-6% of cancer clinical study enrollees, despite representing approximately 13% of the population. Alarmingly, 21% of trials reported zero Black enrollees, highlighting the critical issue of underrepresentation and its implications for understanding treatment performance across diverse genetic backgrounds.
By systematically collecting and analyzing race and ethnicity data as part of clinical trial diversity metrics, researchers can identify these disparities and strive to ensure that all populations benefit equitably from medical advancements. The impact of genetic diversity on treatment efficacy is paramount; it is essential for developing therapies that work effectively across different demographic groups. Notably, one in five new molecular entities authorized by the FDA from 2008 to 2013 exhibited variations in exposure or response among racial or ethnic groups, reinforcing the necessity for customized research strategies. As the sector moves toward more inclusive methods, integrating genetic factors into research designs will be vital for achieving better health outcomes and fostering trust among underrepresented communities.
Moreover, the FDA's Race and Ethnicity Guidance aims to enhance race and ethnicity documentation in studies, providing a regulatory framework that supports these initiatives. To bolster diversity in research studies, stakeholders must prioritize the systematic collection of demographic information and consider employing study navigators to assist underrepresented groups, thereby improving clinical trial diversity metrics.
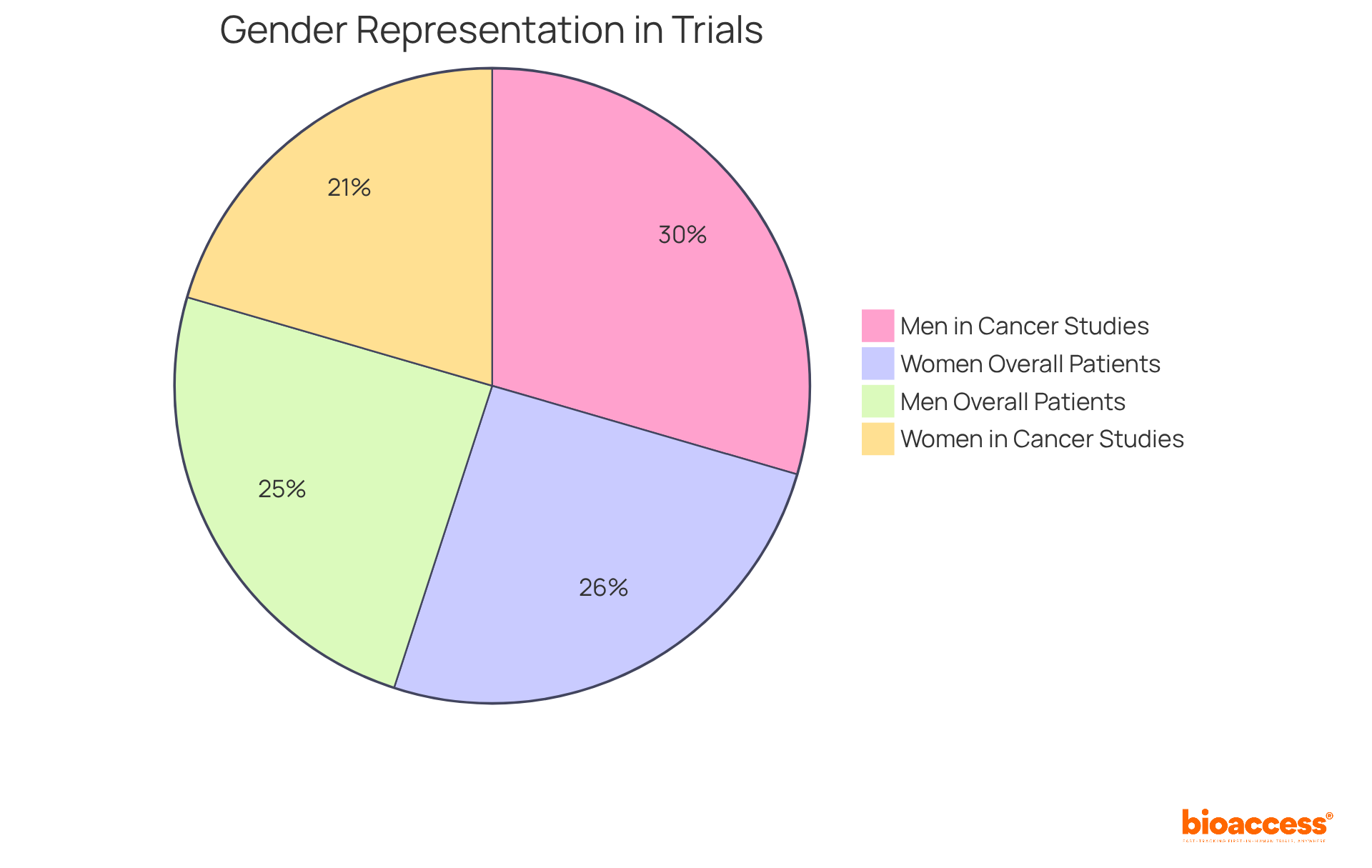
Sex and gender play a pivotal role in evaluating research diversity, as biological differences can significantly influence drug metabolism, effectiveness, and side effects. Research shows that women metabolize certain drugs differently than men, leading to variations in therapeutic outcomes. For example, studies indicate that women often experience higher drug levels at the same dosages due to differences in pharmacokinetics, raising critical concerns about safety and efficacy. Notably, women represent 41% of participants in cancer studies, despite making up 51% of patients, highlighting the urgent need for balanced representation.
By ensuring diverse gender representation in clinical studies, researchers can enhance clinical trial diversity metrics and develop treatments that are not only effective but also safe for all individuals. This approach is essential for improving health outcomes and addressing the unique medical needs of various groups. Furthermore, historical guidelines have often excluded women from early-stage studies, resulting in a lack of gender-specific data and potential unforeseen adverse effects in women. Addressing these challenges is vital for fostering inclusivity and ensuring that clinical trial diversity metrics accurately reflect the demographics of the populations affected by the diseases being studied.
Modeling and simulation methods play a pivotal role in evaluating the impact of clinical trial diversity metrics on the outcomes of clinical studies. By constructing virtual cohorts that accurately reflect real-world demographics, researchers can anticipate how various groups might respond to therapies. This innovative approach not only enhances decision-making in study design but also ensures that research is adequately powered to detect differences among diverse populations, taking into account clinical trial diversity metrics.
Recent trends indicate that integrating virtual populations can significantly elevate the significance of medical studies, leading to improved effectiveness and safety profiles for a broader range of patients. Moreover, research has shown that utilizing these methods can streamline the recruitment process, ultimately resulting in faster and more efficient evaluations. As the industry increasingly prioritizes diversity, the use of clinical trial diversity metrics in modeling and simulation will be crucial for achieving equitable health outcomes.

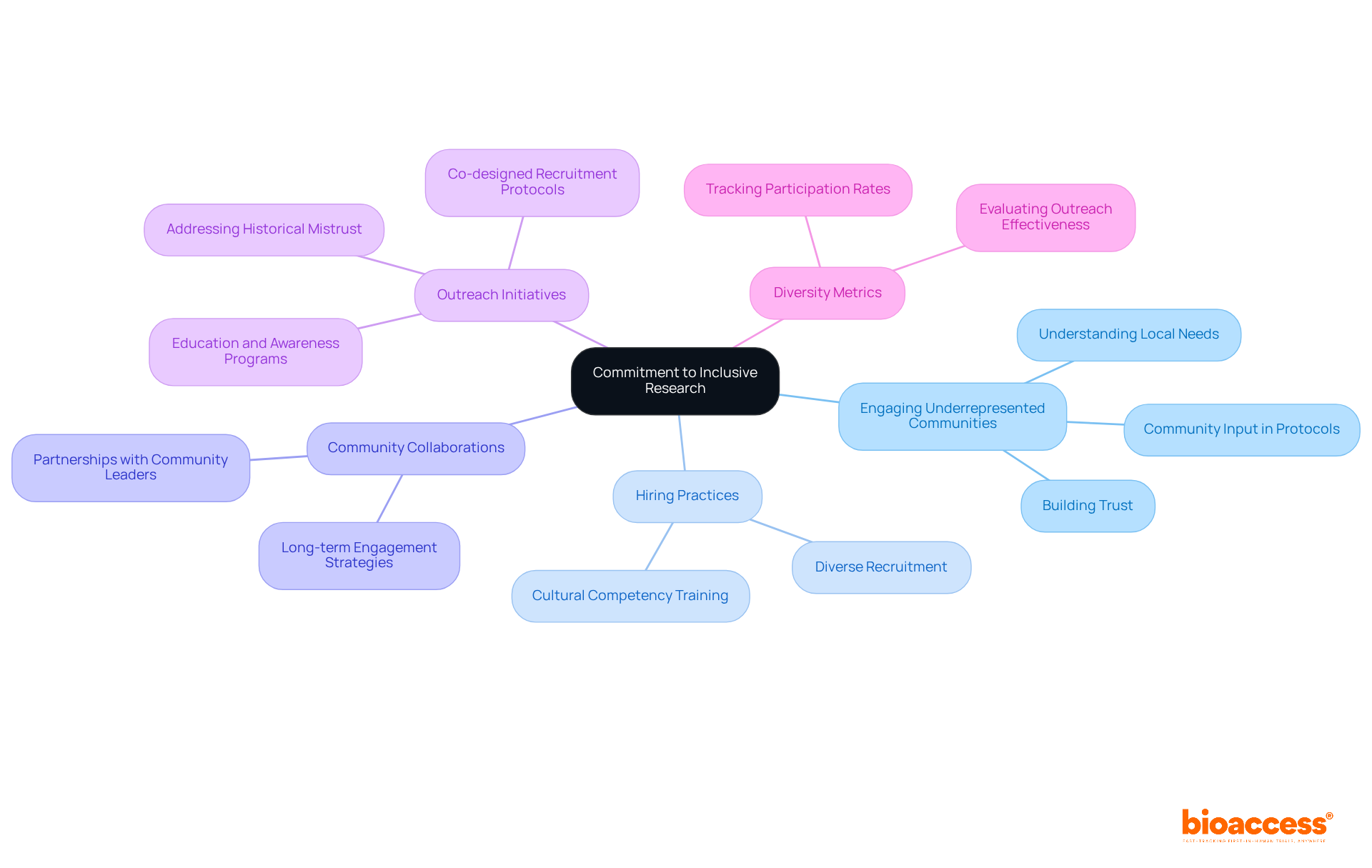
A commitment to inclusive research is crucial for enhancing clinical trial diversity metrics in medical studies. Organizations must actively engage with underrepresented communities, demonstrating a genuine interest in their health needs and concerns. This commitment is evident in hiring practices, research frameworks, and ongoing collaborations with communities, all of which foster trust and encourage participation in research studies that utilize clinical trial diversity metrics. For instance, research indicates that only 8% of participants in new medication studies in the U.S. were Black, and just 11% were Hispanic, highlighting the urgent need for improved outreach initiatives.
Successful organizations, such as Sanofi, have launched community engagement initiatives that focus on understanding local needs and building relationships with community leaders. By investing in education and awareness, these organizations not only tackle historical mistrust but also enhance the inclusivity of their research. Furthermore, strategies like co-designed recruitment protocols that incorporate community input have proven effective in boosting clinical trial diversity metrics. As Raolat Abdulai, Global Clinical Lead at Sanofi, points out, "There are obstacles, including a historical lack of trust in research or medical organizations, and... access to these studies."
Ultimately, a strong commitment to inclusivity benefits not only underrepresented groups but also enriches the research environment, ensuring that findings are relevant across diverse communities.
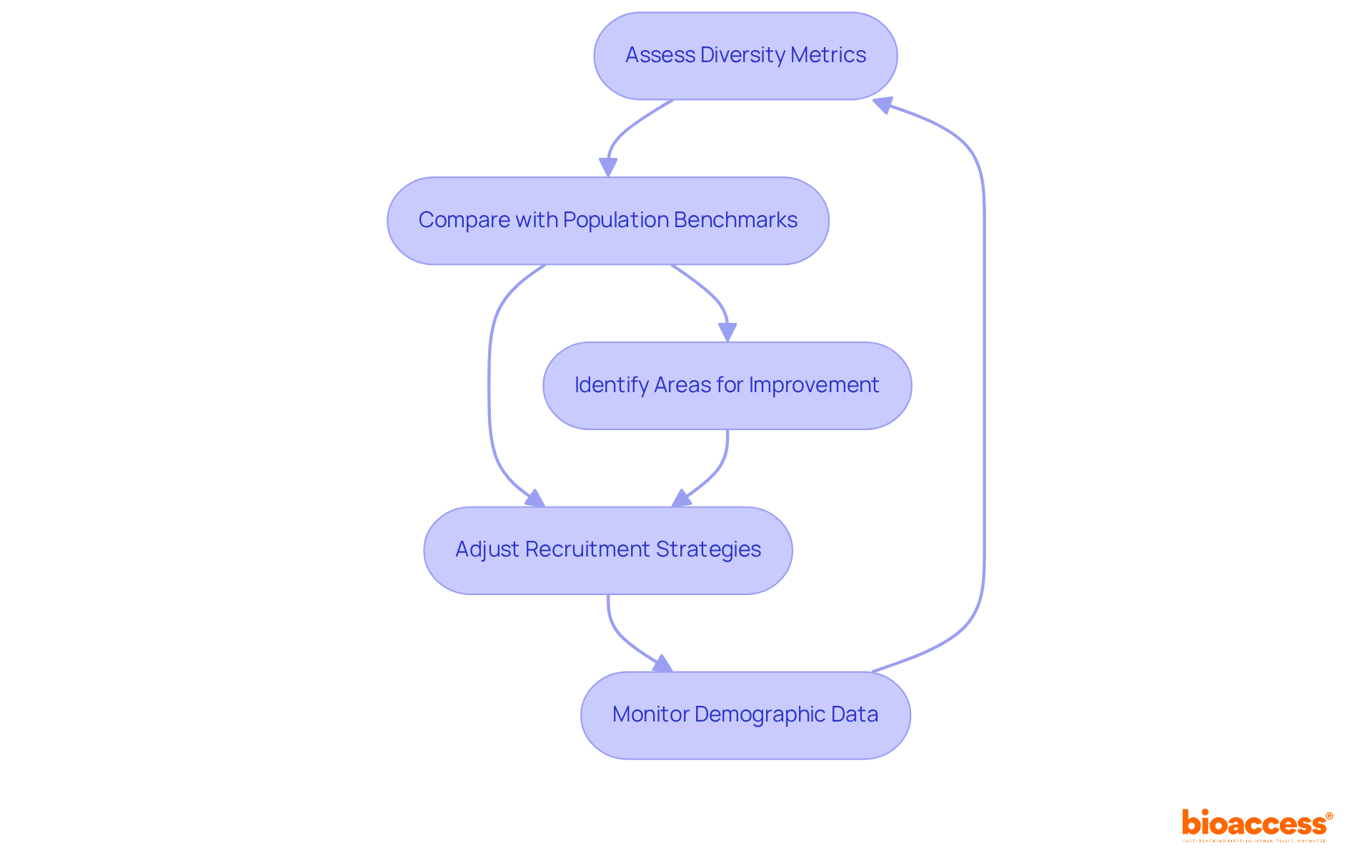
Regular assessment of clinical trial diversity metrics is crucial for tracking progress and identifying areas that need improvement. By systematically evaluating participant demographics against established population benchmarks, organizations can ensure their studies accurately reflect the communities they aim to serve. This iterative feedback process allows for timely adjustments to recruitment strategies and study designs, significantly enhancing the inclusivity and overall effectiveness of research. For instance, monitoring demographic data revealed that in 2023, 35% of clinical study participants were minorities, indicating a positive trend toward greater representation. However, ongoing efforts remain vital, as historical data shows that Black/African American involvement has fluctuated between 10% and 25% across various studies.
The FDA Reauthorization Act of 2017 underscores the importance of including a broader range of patients, highlighting the regulatory commitment to improving representation. By implementing effective practices for demographic tracking—such as setting clear diversity goals and consistently reporting progress—organizations can improve clinical trial diversity metrics and foster a more equitable clinical trial environment that benefits all stakeholders. Moreover, addressing the implications of homogeneous study populations is critical, as such limitations can worsen health disparities and result in treatments that are less effective or carry unforeseen side effects for underrepresented groups.
Enhancing diversity in clinical trials is not just a regulatory requirement; it’s a fundamental necessity for achieving equitable and effective healthcare outcomes. Incorporating diverse participant groups leads to more representative data, which ultimately translates to better treatment efficacy and safety across varied populations. By prioritizing diversity metrics, stakeholders can ensure that clinical research remains relevant and beneficial for all demographics.
Key insights from the discussion highlight the critical role of demographics—such as age, race, ethnicity, and gender—in shaping clinical trial outcomes. Engaging community leaders, simplifying participation processes, and utilizing technology for remote engagement are essential strategies for overcoming barriers to enrollment. Moreover, a commitment to ongoing evaluation and improvement of diversity metrics is vital for tracking progress and ensuring that clinical trials reflect the communities they aim to serve.
The importance of fostering inclusivity in clinical research cannot be overstated. By actively addressing historical disparities and implementing effective outreach initiatives, the healthcare industry can build trust within underrepresented communities. This commitment not only enriches the research environment but also enhances the relevance and applicability of findings, ultimately paving the way for improved health equity. Stakeholders are encouraged to adopt these strategies and prioritize diversity, ensuring that future clinical trials are inclusive and representative of the diverse populations they intend to benefit.
What is bioaccess® and how does it enhance clinical trial diversity?
bioaccess® leverages the regulatory efficiency of Latin America, diverse participant groups from the Balkans, and streamlined processes in Australia to improve research diversity. It facilitates ethical approvals within 4-6 weeks and accelerates enrollment by 50% compared to traditional markets.
Why is diversity in clinical trials important?
Diversity in clinical trials is essential because it improves representation, enhances health outcomes, and increases the generalizability of findings. Research indicates that clinical trial diversity metrics can significantly influence treatment efficacy and safety across different populations.
What types of studies have successfully utilized bioaccess®'s approach?
Successful studies include Early-Feasibility Studies and First-In-Human Studies in the Balkans, which demonstrate that engaging with varied participant groups leads to more robust data and improved healthcare solutions.
What services does bioaccess® provide to support research study management?
bioaccess® offers comprehensive services such as feasibility studies, site selection, compliance reviews, and project management to help clients navigate the complexities of studies while achieving significant cost savings.
What are some demographic factors that impact drug effectiveness and safety?
Factors such as age, race, and gender can significantly influence drug response and treatment outcomes, highlighting the need for diverse populations in research to enhance clinical trial diversity metrics.
What initiatives exist to promote diversity in research studies?
Initiatives like the DEPICT Act mandate diversity action plans in research designs, which are essential for improving clinical trial diversity metrics and addressing historical disparities in healthcare.
What barriers exist that hinder diverse participation in clinical trials?
Barriers include a lack of awareness, distrust in the healthcare system, logistical challenges, stringent eligibility criteria, socioeconomic factors, and geographic limitations.
How do financial barriers affect participation in clinical trials?
Financial hurdles significantly impact participation, especially for individuals with low socioeconomic status, with many citing personal expenses as a major factor in their decision-making.
What strategies can be implemented to overcome geographic limitations in clinical trials?
Implementing decentralized studies that leverage telemedicine, local laboratories, and home health services can help mitigate geographic challenges by bringing the study directly to patients.
Why is cultural humility important in clinical trial diversity?
Fostering cultural humility and acknowledging past injustices are vital for rebuilding trust within communities, which is essential for improving participation and ensuring equitable access to research studies.