


The article underscores the critical significance of control and treatment groups in clinical research, asserting their essential roles in guaranteeing the validity and reliability of study outcomes. It articulates that meticulously structured studies employing these cohorts—incorporating techniques such as randomization and blinding—are vital for isolating treatment effects and minimizing bias. This rigorous approach ultimately culminates in more credible research findings, which are pivotal for enhancing patient care.
In the intricate landscape of clinical research, the effectiveness of treatments often hinges on the meticulous design of control and treatment groups. These groups serve as the backbone of studies, enabling researchers to draw valid conclusions about the efficacy and safety of new medical interventions. By exploring the nuances of how these groups function and the methodologies behind them, readers can uncover critical insights that not only enhance the integrity of clinical trials but also significantly impact patient outcomes.
What challenges arise when these groups are improperly defined?
How can researchers ensure that their findings are both reliable and ethically sound?
At bioaccess®, we harness the power of segments and interventions to enhance research processes. By meticulously designing our studies with these critical components, we ensure the generation of accurate and reliable results that expedite approvals and market access for Medtech, Biopharma, and Radiopharma innovations. Reference sets, which include placebo and active comparisons, serve as benchmarks for control and treatment, enabling us to isolate the impacts of experimental treatments and evaluate their effectiveness relative to standard care. This methodological rigor is essential; only 6.1% of studies adequately reported statistical power analyses, highlighting the need for robust design in clinical trials.
Our strategic presence in Latin America, the Balkans, and Australia empowers us to implement these methodologies effectively, ensuring ethical compliance and rapid patient enrollment. Recent advancements in trial structures, such as the use of multiple comparison sets and innovative blinding techniques, further enhance the reliability of our findings. For instance, employing randomization mitigates bias, while the application of external comparison sets facilitates broader evaluations, enriching our understanding of intervention efficacy.
Leaders in medical research underscore the significance of these methodologies in streamlining processes. By focusing on the integrity of both monitored and experimental sets, bioaccess® not only accelerates research but also contributes to the advancement of medical innovations that can significantly improve patient outcomes.

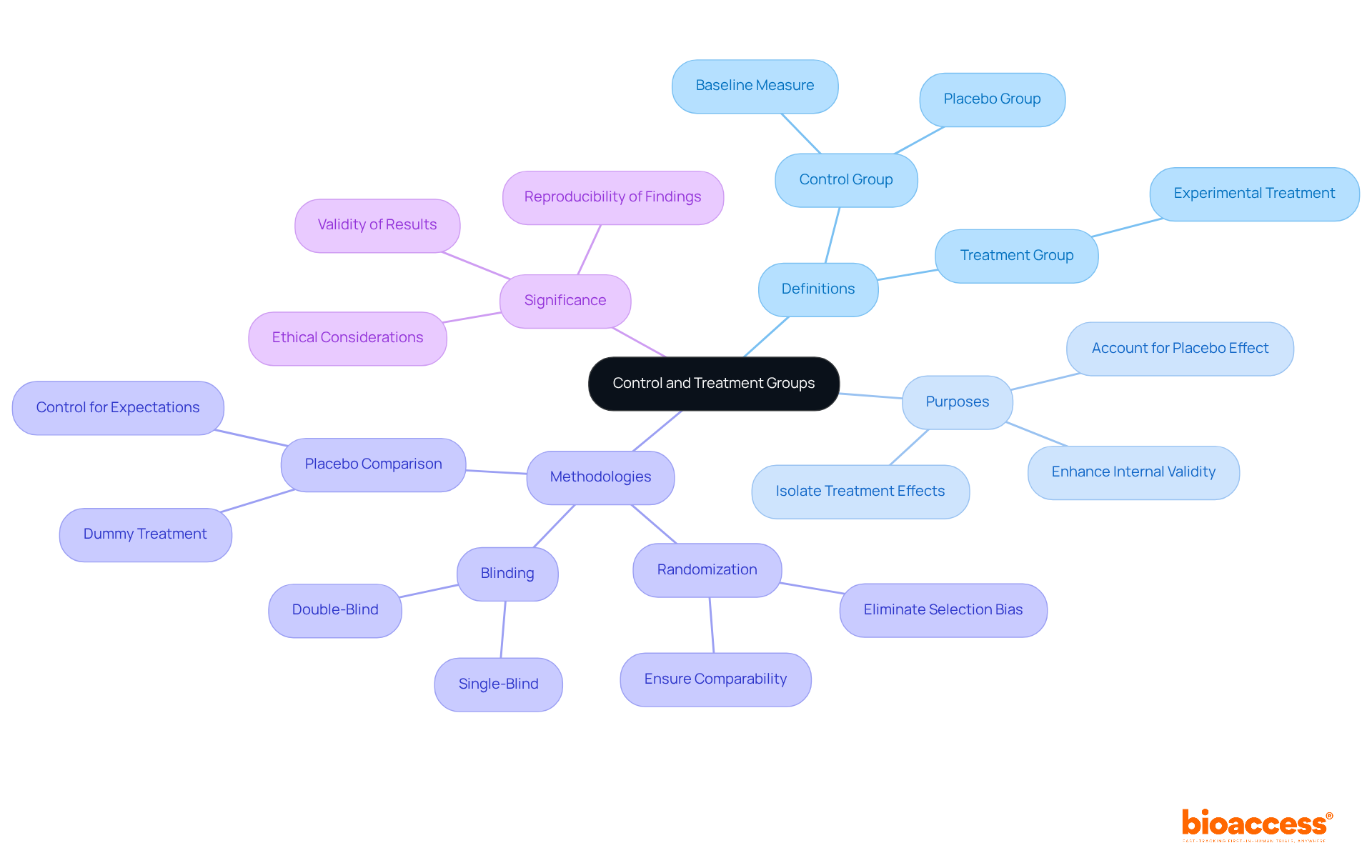
In clinical studies, reference sets play a crucial role by establishing a baseline for comparison with intervention sets. A reference set comprises participants who do not receive the experimental treatment; instead, they may receive a placebo or a conventional treatment. This arrangement is vital for accurately assessing the efficacy and safety of new interventions. For instance, in the landmark Salk polio vaccine trials conducted in 1954, over 600,000 school students participated, with one group receiving a placebo while another group received no injection at all. The results revealed that the vaccine was nearly 90% effective, underscoring the importance of having a clearly defined reference set.
Reference sets can take various forms, including:
Each type serves distinct purposes based on the research question and ethical considerations. For example, placebo comparison sets are often regarded as the gold standard for evaluating the effectiveness of interventions, as they help isolate the effects of the experimental intervention from psychological factors associated with receiving any treatment. Active treatment sets consist of participants receiving a standard therapy recognized as effective, while no treatment sets involve participants who receive no intervention whatsoever.
Recent statistics indicate that the use of placebo in comparison sets remains prevalent in clinical trials, as it allows researchers to evaluate the true effect of the experimental intervention. Moreover, participants in the Diabetes Prevention Program's lifestyle modification cohort experienced a 58% reduced risk of developing type 2 diabetes compared to the placebo cohort, highlighting the significance of comparison cohorts in contemporary research. Expert insights emphasize that maintaining similarity between the control and treatment sets is essential to avoid invalid results. As Sindhuja A. notes, 'Control and treatment teams are essential in medical trials and research experiments to validate the outcomes.' Techniques such as randomization and blinding are employed to minimize bias and ensure that both sets are comparable in known and unknown factors.
Understanding the interactions of care teams is vital for medical research. These teams consist of participants who undergo the experimental intervention, and their outcomes are compared with those of the reference set. This comparison is crucial for determining the effectiveness and safety of the new intervention in terms of control and treatment, ultimately influencing medical decisions and regulatory approvals. Ethical considerations regarding the use of comparison sets are also paramount, as researchers must safeguard the rights and welfare of participants while striving for scientifically reliable outcomes.

Control and treatment cohorts are essential for maintaining the internal validity of clinical trials, as they allow researchers to differentiate the effects of the intervention from other influencing factors. By comparing outcomes between the control and treatment cohorts, researchers can ascertain whether the observed effects stem from the treatment itself or from external influences. This comparison is essential for establishing causality and bolstering the credibility of the study's findings.
Statistics reveal that 48% of studies requiring a comparison set fail to include a clearly defined one, underscoring the importance of proper comparison set implementation. Research that effectively employs comparison sets significantly enhances internal validity, leading to more reliable conclusions.
Experts emphasize that a well-structured comparison set is crucial for isolating the impacts of the independent variable. As trial officials assert, without a reference set, it becomes challenging to determine if changes in treatment participants are genuinely due to the control and treatment or merely a result of natural progression.
For example, in a study assessing a new treatment for ADHD, the inclusion of a placebo comparison enabled researchers to differentiate between the medication's effects and the placebo effect, thereby ensuring robust internal validity. Such instances illustrate the critical role of reference sets in clinical research, reinforcing their function as a cornerstone for valid and dependable findings.

Treatment groups comprise participants receiving the intervention under investigation, with their outcomes compared to those of a control and treatment group. This comparison is essential for evaluating the effectiveness of the control and treatment intervention, as it helps determine whether any observed improvements are statistically significant. Such evaluations are crucial for guiding clinical decisions and securing regulatory approvals.
Clinical researchers emphasize that the integrity of intervention comparisons can significantly affect study results. Successful comparisons between control and treatment groups enhance the reliability of findings, as evidenced by recent studies in 2025 that underscore the importance of rigorous methodologies in evaluating intervention effects. By maintaining strict inclusion and exclusion criteria and ensuring random assignment, researchers can effectively isolate the impact of the intervention, thereby providing robust evidence for its efficacy.
Furthermore, bioaccess plays a pivotal role in enabling these trials by delivering comprehensive trial management services, including:
This support not only elevates the quality of medical research but also stimulates local economies through job creation and healthcare enhancements. Ultimately, the function of intervention teams in clinical trials is critical, as they not only guide clinical practice but also shape the future of medical advancement.

The essential methodological difference between control and treatment sets lies in their assignment of interventions. Control and treatment sets do not receive the experimental intervention, whereas experimental sets do. This critical distinction significantly influences data collection, analysis, and interpretation. To ensure valid conclusions regarding the efficacy of the control and treatment, researchers must maintain comparability between both sets in all aspects except for the intervention itself.
Utilizing random assignment methods—such as simple randomization, stratified randomization, or covariate-adaptive randomization, which modifies assignment probabilities based on observed covariates—can enhance the integrity of comparability among participants. Additionally, employing allocation concealment methods, like sealed envelope techniques, helps prevent predictability in group assignments, further safeguarding the study's validity.
Citations from research methodologists underscore the significance of this distinction. One remarked, "In a controlled experiment, all variables apart from the independent variable are kept constant," emphasizing the importance of strict design in resource allocation. Furthermore, the selection of intervention allocation can directly influence research outcomes; well-organized randomization not only reduces bias but also improves the dependability of results.
Current best practices advocate for the use of centralized randomization systems and rigorous training for personnel involved in the process, ensuring that randomization is executed effectively and ethically. Conducting a statistical power analysis is essential for determining the necessary sample size, which is crucial for ensuring the validity of the study's findings. By adhering to these principles, including the consideration of placebo cohorts to prevent changes in outcomes due to participant awareness, researchers can significantly enhance the robustness of their trials.

In the arrangement of management and intervention groups, emphasizing ethical considerations is essential. Researchers must ensure that informed consent is obtained, which involves providing participants with comprehensive information about the study's objectives, risks, and benefits. As emphasized, 'Informed consent is the backbone of ethical medical research.' This process not only upholds the principle of autonomy but also fosters trust between researchers and participants.
Reducing risks is crucial, especially when employing placebo controls; such controls must be justified in the context of control and treatment, particularly in the presence of effective therapies. Ethical oversight by Institutional Review Boards (IRBs) is crucial for safeguarding participant welfare and maintaining the integrity of the research process. Research institutions must establish IRBs to ensure the safety of human subjects.
Present guidelines highlight the importance of clear informed consent practices adapted to the intricacies of trials, especially those involving cutting-edge technologies such as AI. As highlighted in recent discussions, the ethical implications of expanding access to interventions without ensuring equitable control and treatment options must be carefully considered to avoid exacerbating existing health disparities. A study noted the need for equitable access to AI screening, especially for underserved populations.
The incorporation of AI into medical workflows further complicates these ethical considerations, necessitating a nuanced understanding of how to balance innovation with participant safety and ethical obligations. To navigate this ethical issue in medical research effectively, it is imperative to ensure that informed consent is truly informed.

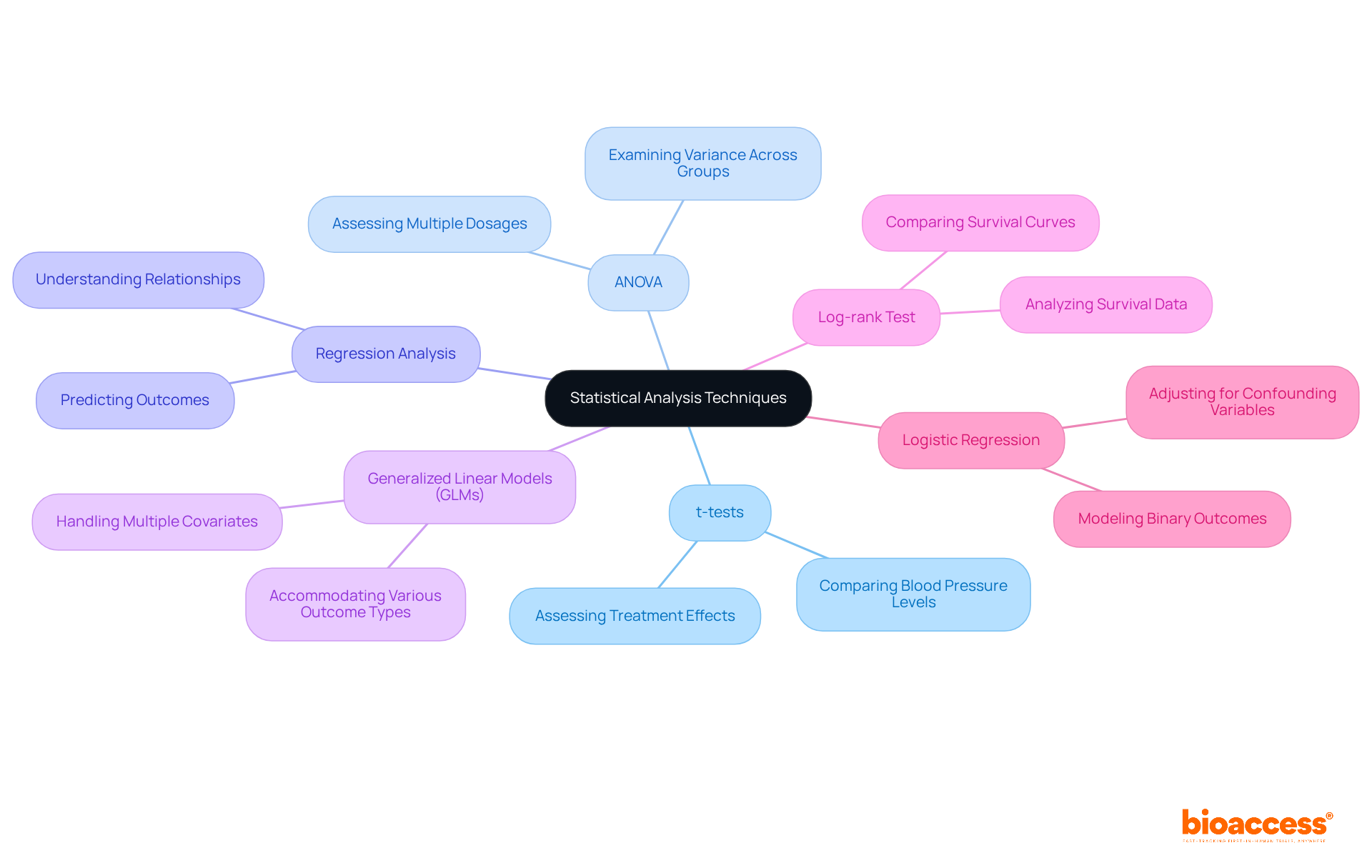
Statistical analysis techniques for control and treatment categories are essential in clinical research. Methods such as t-tests, ANOVA, and regression analysis play crucial roles, enabling researchers to evaluate whether differences in outcomes between populations are statistically significant. For instance, t-tests are frequently utilized to compare averages between two sets, while ANOVA broadens this comparison to three or more sets, allowing for a thorough examination of variance across various treatment conditions. In clinical research, a t-test could involve comparing the blood pressure levels of patients receiving a new medication versus those on a placebo. Similarly, ANOVA could assess the effectiveness of various dosages of a drug across multiple patient categories.
Recent advancements in statistical methods have refined the analysis of treatment and control groups. The integration of generalized linear models (GLMs) accommodates various outcome types, enhancing the robustness of findings. Proper statistical planning is crucial; it ensures that studies are adequately powered to detect meaningful effects and that potential confounding variables are accounted for. As highlighted by biostatisticians, careful planning in statistical design is vital for obtaining valid and reliable outcomes in research trials. This approach strengthens the internal validity of research and facilitates the translation of findings into clinical practice.
Moreover, the application of reference sets is essential in experimental design, as they assist in separating the impacts of the intervention from other factors. Random allocation of participants into comparison and intervention categories reduces variations that could obscure results, further emphasizing the significance of thorough statistical techniques in the control and treatment. Furthermore, methods such as the log-rank test are crucial for analyzing survival data, while logistic regression models can be employed for binary outcomes, providing a comprehensive toolkit for researchers.
Faulty experimental segments pose significant threats to the validity of clinical research, often leading to misleading conclusions. A primary concern is selection bias, which arises when reference sets differ markedly from intervention sets, potentially skewing results. For instance, a literature review revealed that 48% of studies lacking a comparison cohort failed to include one, thereby limiting the ability to draw reliable comparisons.
Furthermore, confounding variables that are not effectively subjected to control and treatment can obscure the true effects of the intervention, complicating the interpretation of study outcomes. As emphasized by experts in the field, having a clearly defined reference set is essential for establishing causality and ensuring that observed changes in the dependent variable are attributable to the treatment rather than external influences.
Therefore, meticulous design and oversight of experimental sets are crucial for maintaining the validity and reliability of clinical research outcomes.

To mitigate risks in experimental design, researchers must prioritize randomization, ensuring that participants are assigned to categories without bias. This process is essential for preserving the integrity of trial results, as it aids in balancing known and unknown confounding variables across intervention categories. A typical allocation ratio, for instance, is 1:1, where identical numbers of participants are assigned to both the experimental group and the control and treatment group.
Furthermore, blinding enhances this process by reducing the influence of participant and investigator expectations on outcomes, thereby maintaining the objectivity of the study. In a recent trial involving a new hypertension medication, participants were randomly assigned to either a placebo group or a group receiving the control and treatment. This design allowed for a clear assessment of the new drug's efficacy.
As noted by L. Thomas, the use of control and treatment sets assists in maintaining the internal validity of your research. Current best practices advocate for regular monitoring and interim analyses throughout the trial. This ongoing evaluation can identify potential issues early, enabling timely adjustments to the study design and ensuring that the trial remains robust and reliable.
By employing these strategies, researchers can significantly reduce the risk of biases that could undermine the validity of their findings, ultimately leading to more trustworthy and practical outcomes in medical research.

Control and treatment cohorts serve as the cornerstone of clinical research, ensuring the validity and reliability of study outcomes. Understanding their definitions, purposes, and the ethical and statistical considerations is crucial for researchers. Control and treatment sets provide a baseline assessment, allowing researchers to determine if the changes observed in the treatment cohort are directly due to the treatment or influenced by other factors. For instance, in a study involving 100 participants, a 5% sample would consist of only 5 individuals, underscoring the necessity of a sufficiently sized comparison set for reliable conclusions.
Advancements in medical understanding often stem from well-structured studies that effectively utilize these cohorts. The application of placebo comparison sets is recognized as one of the most rigorous methods for evaluating intervention effectiveness, as they help in the control and treatment of the placebo effect, wherein participants' beliefs about the intervention can shape their responses. Recent findings indicate that studies employing robust methodologies, such as randomization and blinding, significantly enhance patient outcomes through effective control and treatment by minimizing bias and ensuring equivalence between intervention and reference sets.
Clinical research leaders stress the significance of meticulous study designs. As one noted, 'Randomization and blinding are two techniques frequently employed to reduce the likelihood of bias and guarantee that the test and comparison sets receive identical handling throughout the length of the clinical trial.' This observation emphasizes the necessity of incorporating comparison sets to isolate the effects of the independent variable, thereby bolstering the credibility of research outcomes. Ultimately, the careful design of control and treatment groups not only strengthens the internal validity of studies but also promotes the overarching objective of improving patient care and advancing medical science.
Control and treatment groups are fundamental components of clinical research that ensure the integrity and reliability of study findings. By establishing clear distinctions between these cohorts, researchers can accurately assess the efficacy of new interventions and draw meaningful conclusions that influence medical practice and regulatory decisions.
The article highlights several key insights regarding the importance of control and treatment groups, including their roles in:
Emphasizing methodologies such as randomization and blinding, it becomes evident that these practices significantly reduce bias and enhance the credibility of research outcomes. Moreover, the article underscores the critical need for well-defined reference sets to isolate the effects of interventions, ultimately leading to more dependable and impactful results.
In reflecting on these insights, it is clear that the meticulous design and implementation of control and treatment groups are paramount in advancing clinical research. As the landscape of medical innovation continues to evolve, embracing best practices in study design will not only improve patient outcomes but also contribute to the overarching goal of enhancing healthcare quality. Researchers and institutions are encouraged to prioritize these methodologies, ensuring that future studies are built on a foundation of integrity and scientific rigor.
What is the role of bioaccess® in clinical research?
Bioaccess® enhances research processes by utilizing segments and interventions to generate accurate and reliable results, expediting approvals and market access for Medtech, Biopharma, and Radiopharma innovations.
What are reference sets in clinical research?
Reference sets are groups of participants that do not receive the experimental treatment, serving as benchmarks for control and treatment groups. They may receive a placebo or a conventional treatment, allowing for accurate assessment of the efficacy and safety of new interventions.
What types of reference sets are commonly used?
Common types of reference sets include placebo reference, active reference, and no intervention reference, each serving distinct purposes based on research questions and ethical considerations.
Why are placebo comparison sets considered the gold standard?
Placebo comparison sets are regarded as the gold standard because they help isolate the effects of the experimental intervention from psychological factors associated with receiving any treatment, allowing for a clearer evaluation of effectiveness.
How do control and treatment groups contribute to the validity of clinical trials?
Control and treatment groups maintain the internal validity of clinical trials by allowing researchers to differentiate the effects of the intervention from other influencing factors, establishing causality, and bolstering the credibility of the study's findings.
What challenges exist in implementing comparison sets in studies?
Statistics show that 48% of studies requiring a comparison set fail to include a clearly defined one, which highlights the importance of proper implementation to enhance internal validity and reliability of conclusions.
What techniques are used to minimize bias in clinical trials?
Techniques such as randomization and blinding are employed to minimize bias and ensure that control and treatment sets are comparable in known and unknown factors.
Why is ethical consideration important in the use of comparison sets?
Ethical considerations are paramount as researchers must safeguard the rights and welfare of participants while striving for scientifically reliable outcomes in clinical research.