


The journey of a medical device from concept to market is undeniably complex and multifaceted, often filled with both challenges and opportunities. Understanding the ten distinct phases of the medical device life cycle not only illuminates the path innovators must navigate but also underscores the critical importance of strategic planning and compliance in delivering effective healthcare solutions.
As companies strive to meet the ever-growing demand for innovative medical technologies, a pressing question emerges: how can they accelerate this life cycle while ensuring safety, efficacy, and regulatory adherence?
This exploration delves into each phase, revealing insights that could reshape the future of medical device development.
bioaccess® excels in delivering rapid clinical research services tailored for the Medtech sector. By leveraging the compliance speed of Latin America, the diverse patient demographics of the Balkans, and the efficient ethical approval processes in Australia, bioaccess® secures ethical approvals in an impressive 4-6 weeks. This remarkable efficiency leads to enrollment rates that are up to 50% faster than traditional markets, significantly accelerating the medical device life cycle from initial concept to market entry.
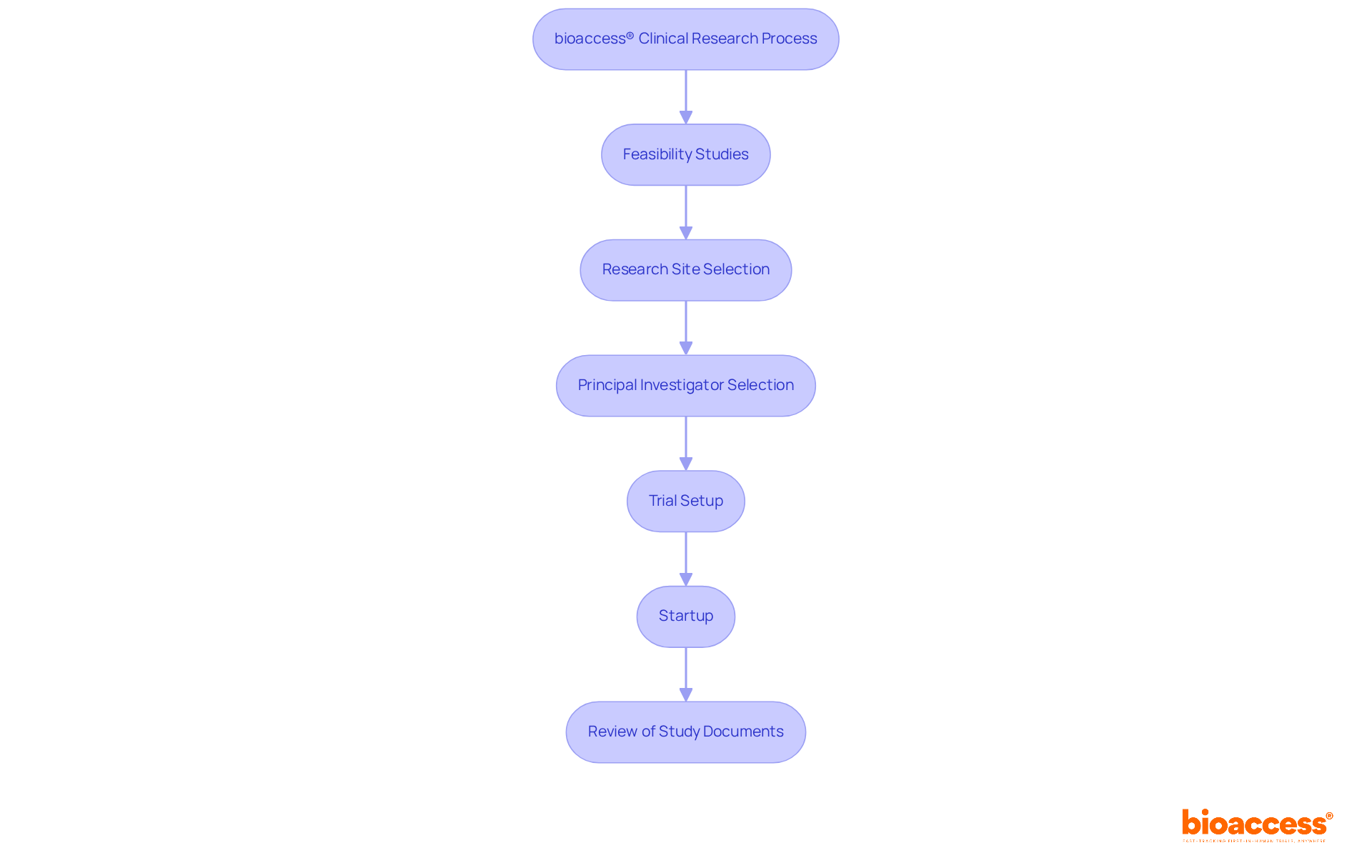
Recent advancements in clinical research underscore the importance of such flexibility. Companies are increasingly navigating complex compliance environments while addressing the growing demand for innovative healthcare solutions. bioaccess® offers a comprehensive process that encompasses:
The partnership with Welwaze Medical Inc. for the Celbrea® healthcare product launch in Colombia exemplifies how bioaccess® supports Medtech and biopharma startups in Latin America, enhancing their market access and regulatory compliance. As industry specialists emphasize, integrating advanced technologies and forming strategic alliances is crucial for improving the speed and efficiency of clinical trials. This ultimately benefits healthcare and accelerates the delivery of innovative solutions to those in need.
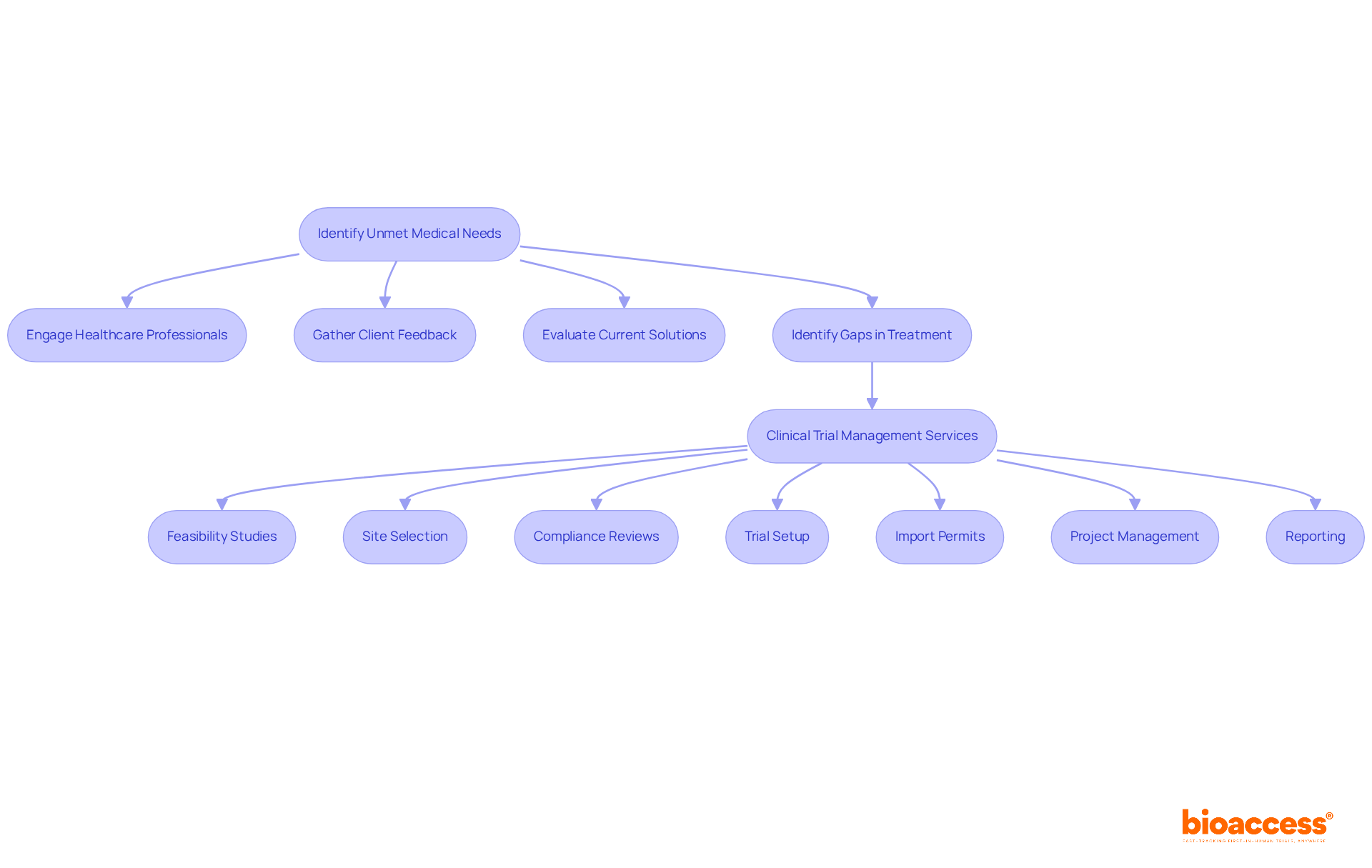
The concept phase is vital in the medical device life cycle, emphasizing thorough research to identify unmet health needs within the healthcare environment. Engaging healthcare professionals - who make up a significant portion of the workforce in identifying these needs - is essential. Their insights, paired with client feedback, empower innovators to evaluate current solutions and uncover specific gaps in treatment or diagnosis. For example, recent trends in medical equipment innovation in 2025 spotlight tools developed directly from patient experiences, underscoring the importance of this feedback loop. By tailoring tools to address these recognized needs, innovators significantly enhance their chances of acceptance and success in subsequent phases.
To support this process, bioaccess offers comprehensive clinical trial management services, including:
These services not only streamline the clinical trial process but also contribute to the overall success of healthcare innovations. As one healthcare expert noted, "Comprehending the real-world difficulties encountered by individuals is essential for creating effective medical solutions." This collaborative approach, supported by bioaccess's expertise, fosters innovation and ensures that new devices align with the actual demands of the healthcare system throughout the medical device life cycle, ultimately transforming lives in Latin America through advanced Medtech.
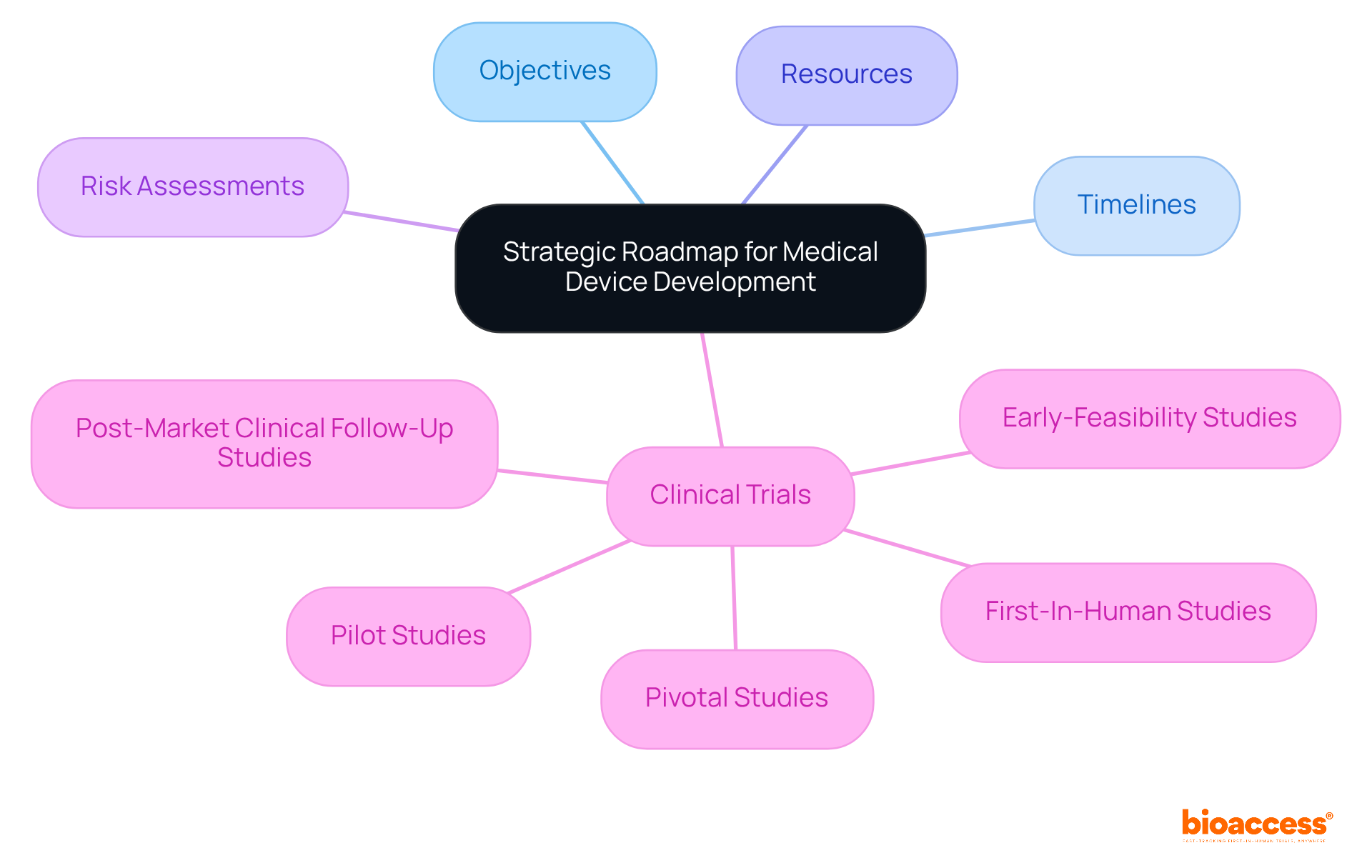
During the planning phase of the medical device life cycle, a strategic roadmap is created that outlines the project’s objectives, timelines, and required resources. This roadmap is crucial for guiding the entire development process, ensuring that all team members are aligned and milestones are met. It also encompasses risk assessments and contingency plans to tackle potential challenges that may arise during development.
With bioaccess®'s expertise in managing clinical trials - including Early-Feasibility Studies, First-In-Human Studies, Pilot Studies, Pivotal Studies, and Post-Market Clinical Follow-Up Studies - this roadmap can be tailored to navigate the complexities of compliance approvals and patient enrollment. Their expedited method allows for official approval in just 6-8 weeks, significantly faster than conventional timelines. This efficiency enables treatment-naive cardiology or neurology groups to be enrolled 50% faster than Western sites.
Such strategic planning ensures that all aspects of the clinical trial are managed effectively, paving the way for successful outcomes. By collaborating with bioaccess®, you can address the key challenges in clinical research and enhance your trial's success.
During the design stage of the medical device life cycle, teams create detailed specifications and develop prototypes for healthcare apparatuses. This iterative design process, which is part of the medical device life cycle, involves testing initial prototypes for functionality, usability, and safety. The feedback from these tests is crucial for refining the design throughout the medical device life cycle, ensuring that the final product meets compliance standards and user requirements.
In Colombia, adherence to INVIMA regulations is not just important; it’s essential. The Colombia National Food and Drug Surveillance Institute oversees the marketing and manufacturing of health products, ensuring their safety, efficacy, and quality. Within INVIMA, the Directorate for Health Equipment and other Technologies plays a pivotal role in regulating healthcare instruments, proposing technical standards, and ensuring compliance with pre- and post-market requirements. Understanding INVIMA's role as a Level 4 health authority, as classified by PAHO/WHO, is vital for teams navigating the compliance landscape effectively.
Effective prototyping can significantly reduce time to market in the medical device life cycle by identifying issues early in the development process. Organizations that employ iterative design methodologies report a remarkable 43% decrease in time to market compared to traditional approaches. This statistic underscores the importance of a robust design process in the Medtech landscape, especially within the medical device life cycle, where collaboration and adherence to regulatory standards are paramount.

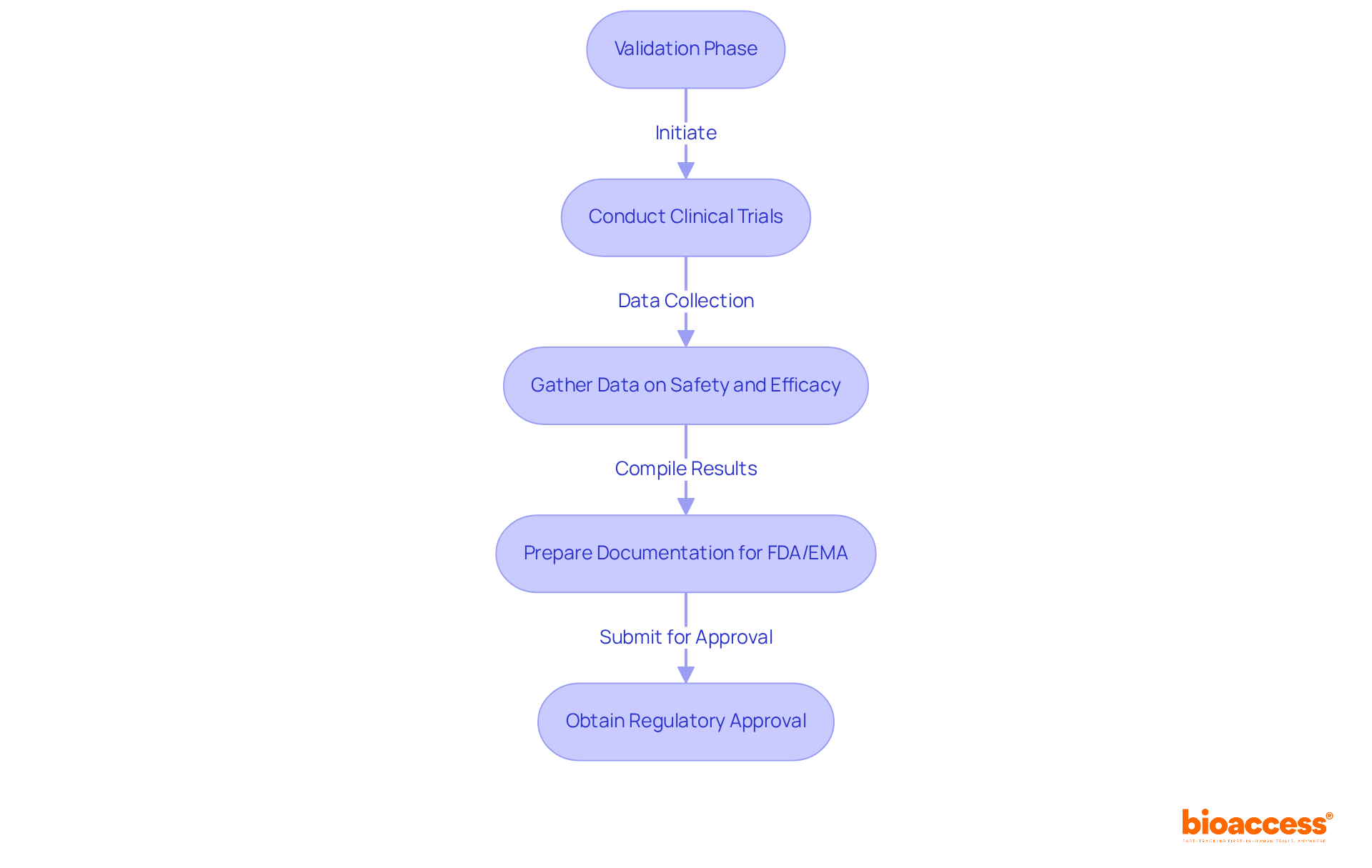
The validation phase, which is crucial in the medical device life cycle, demands rigorous testing to ensure that the device meets all compliance standards and functions effectively. This phase involves conducting clinical trials aimed at gathering substantial data on both safety and efficacy. For instance, as of May 2023, over 58,000 clinical studies were underway in early phases, highlighting the extensive research efforts dedicated to supporting submissions.
Preparing comprehensive documentation for oversight organizations, such as the FDA or EMA, is vital for successful validation. This process not only facilitates the necessary approvals but also ensures that the product can be marketed safely and efficiently. The average duration for clinical trials seeking regulatory approval can exceed 10 years, which underscores the importance of meticulous planning and execution during this phase to prevent delays and ensure compliance.
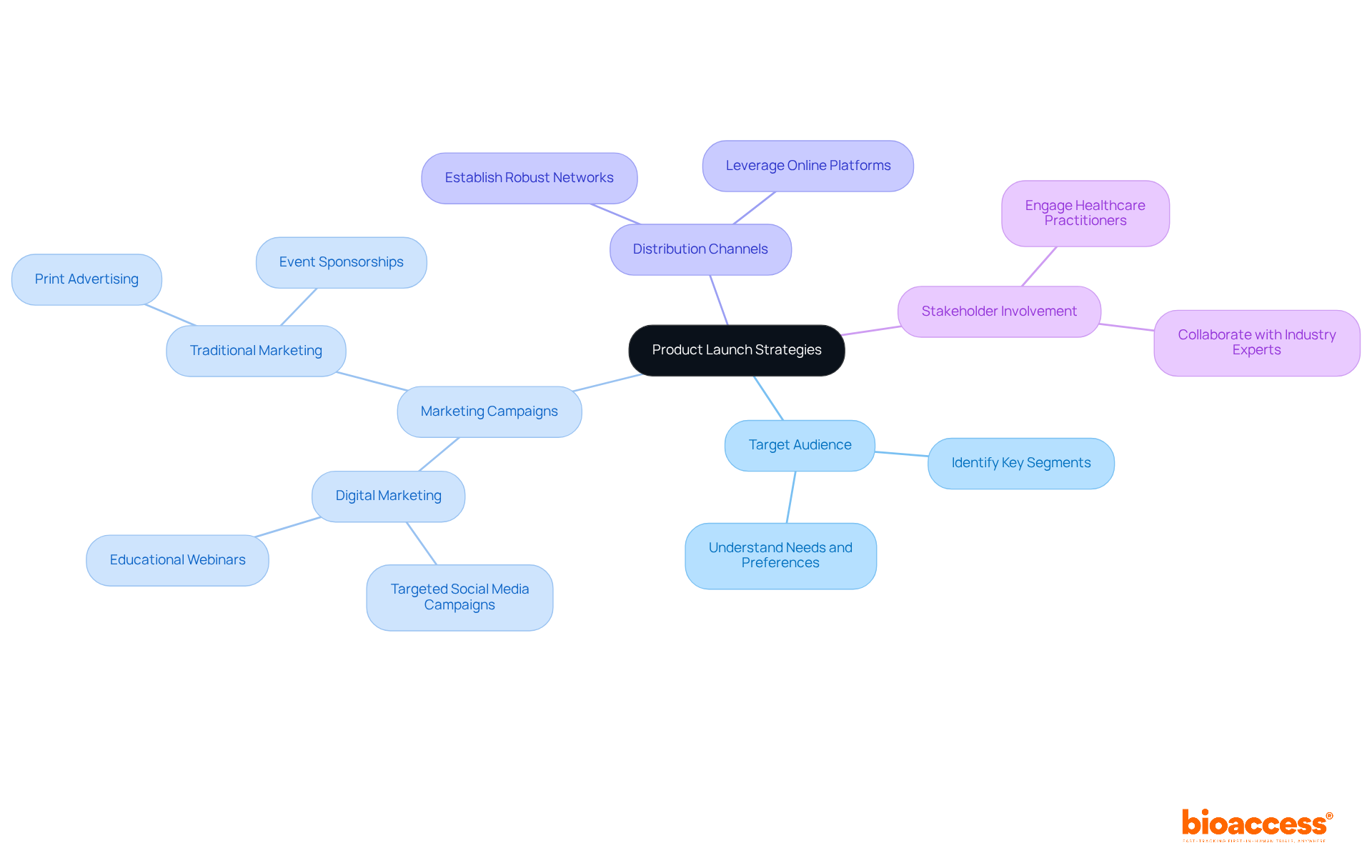
During the product launch phase, developing comprehensive strategies is essential for effectively introducing healthcare instruments to the market. This process begins with identifying target audiences and crafting compelling marketing campaigns, while also establishing robust distribution channels. Involving healthcare practitioners and stakeholders is vital for creating awareness and building trust in the new product.
A well-executed launch can significantly impact initial sales. Studies indicate that successful marketing campaigns can lead to an average initial sales growth of 20-30% post-launch, as noted in industry analyses. For instance, leveraging digital marketing strategies - such as targeted social media campaigns and educational webinars - can enhance visibility and foster relationships with potential users. This aligns with the rising trend of incorporating digital health technologies, which are becoming increasingly significant in the healthcare equipment landscape.
Ultimately, a strategic approach to product introduction not only establishes a foothold in the competitive healthcare equipment market but also sets the stage for long-term success. Collaboration among stakeholders will be crucial in navigating the challenges of clinical research and ensuring that the product meets the needs of its users.
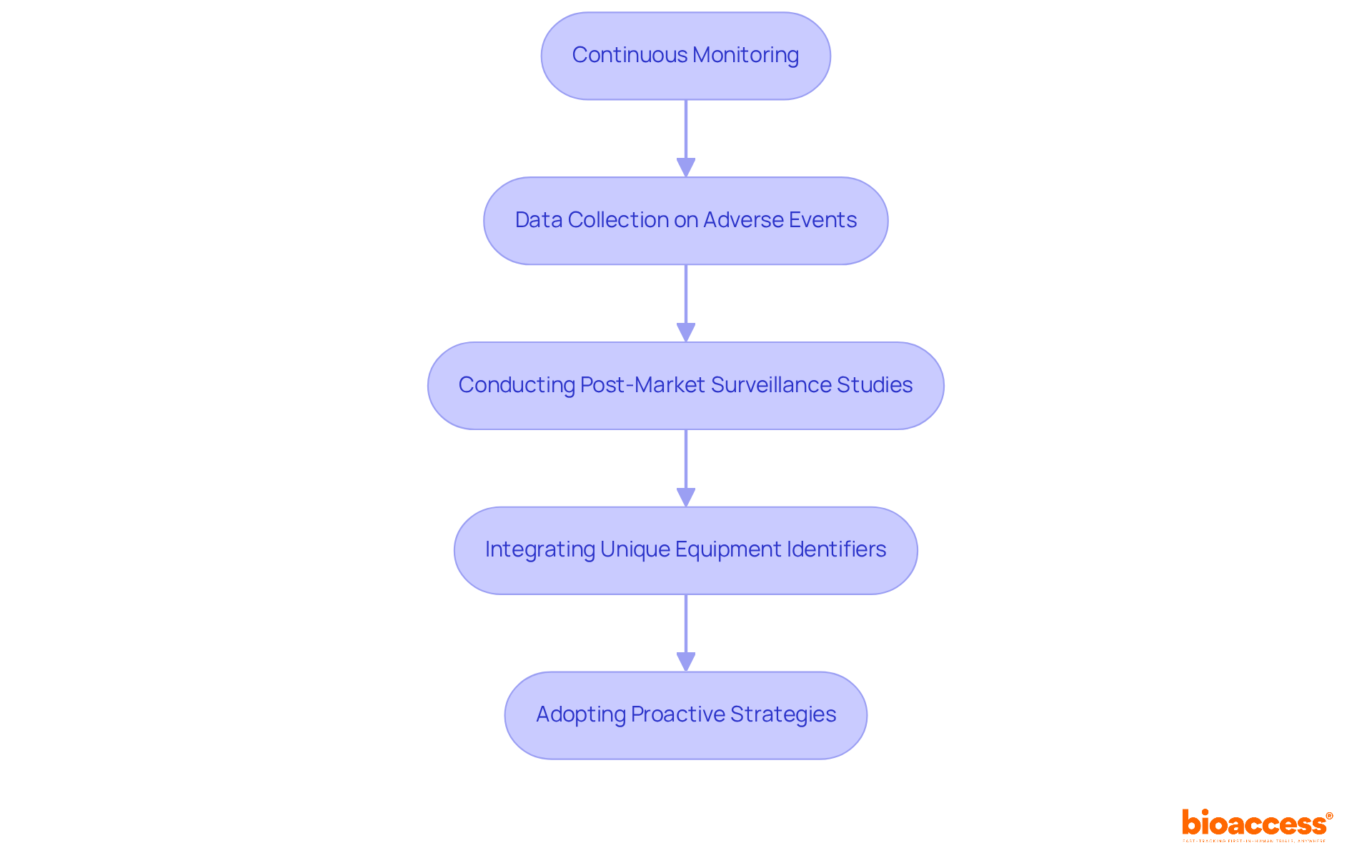
The post-market phase is crucial for ensuring the ongoing safety and effectiveness of medical products within the medical device life cycle. It involves continuous monitoring of equipment performance and adherence to standards. This includes the systematic collection of data on adverse events, which is vital for identifying potential safety issues throughout the medical device life cycle. Recent studies reveal that a significant portion of adverse events are reported late, with nearly a third of initial manufacturer reports not submitted within the regulatory deadline. Such delays can obstruct timely responses to safety concerns, underscoring the necessity for robust post-market surveillance systems.
Conducting post-market surveillance studies is essential for evaluating real-world equipment performance throughout the medical device life cycle. These studies not only track negative occurrences but also gather user feedback, which is critical for guiding future enhancements and updates to the product. For example, integrating unique equipment identifiers into databases could improve tracking and provide a more comprehensive view of outcomes.
As we approach 2025, the landscape of post-market surveillance is transforming, marked by increasing regulatory scrutiny and the implementation of more stringent data collection requirements. This shift necessitates that manufacturers adopt proactive strategies for overseeing equipment performance, ensuring that safety information reaches healthcare providers and individuals promptly. By leveraging advanced data analytics and machine learning, companies can bolster their surveillance capabilities, ultimately enhancing patient safety and equipment reliability.
Regulatory compliance stands as a cornerstone for medical equipment manufacturers, demanding strict adherence to a complex web of legal requirements set forth by regulatory bodies like the FDA and EMA. Understanding equipment classification, navigating pre-market approval processes, and fulfilling post-market obligations are crucial. For instance, the FDA's Breakthrough Devices Program (BDP) has streamlined the approval process for innovative products, allowing for quicker reviews while ensuring safety and effectiveness.
Organizations must establish robust quality management systems and maintain comprehensive documentation to demonstrate compliance throughout the medical device life cycle. Recent regulatory shifts, including updates to the FDA's guidance on health equity and the EMA's initiatives for accelerated assessments, highlight the necessity of staying informed about evolving regulations. This vigilance is not just essential for compliance; it is also vital for achieving market success in an increasingly competitive landscape.
As the Medtech sector continues to evolve, the importance of collaboration and proactive engagement with regulatory changes cannot be overstated. Are you prepared to navigate these challenges and leverage the opportunities they present? The path to success lies in understanding and adapting to the regulatory environment.

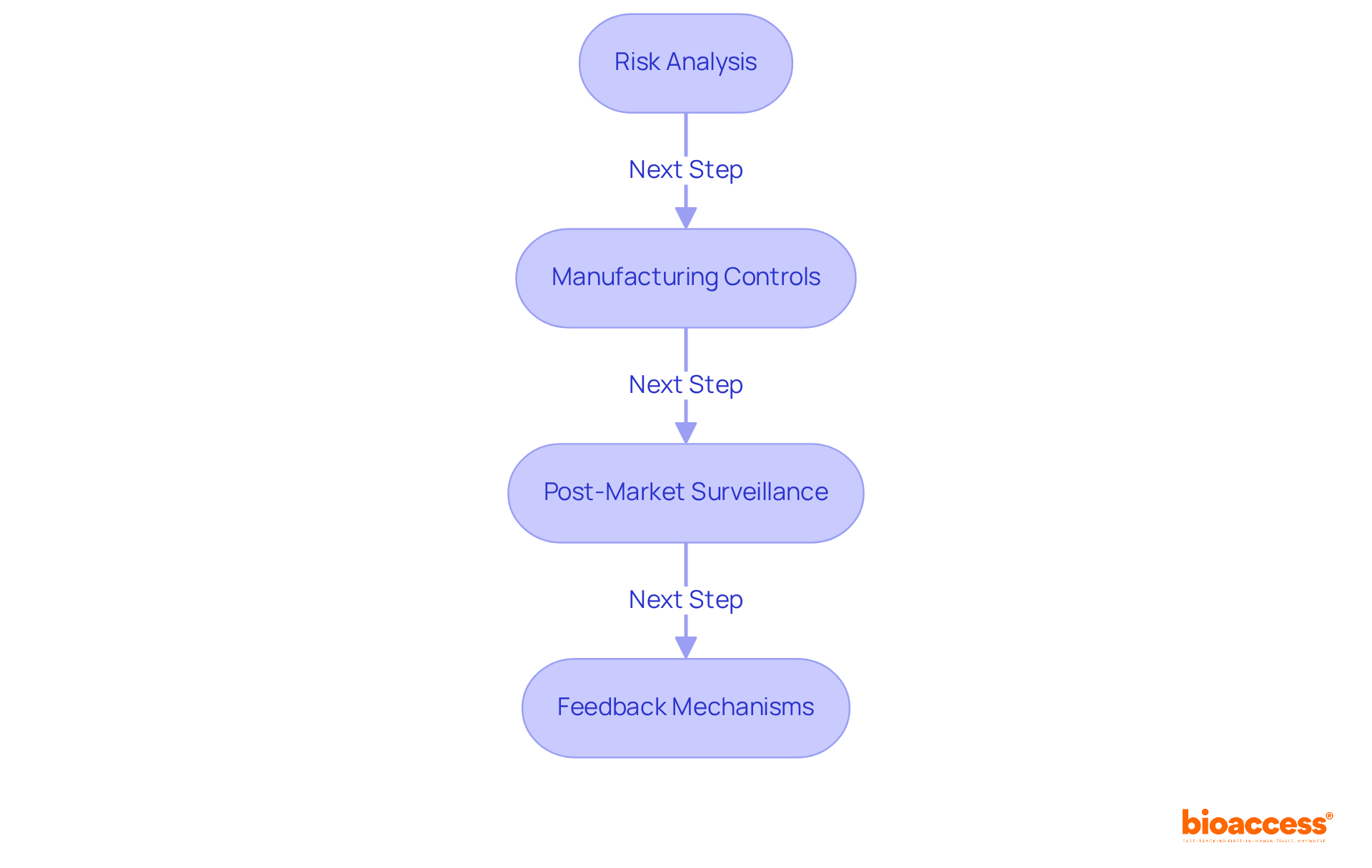
Effective risk management is essential for ensuring safety and equipment reliability throughout the medical device life cycle. This process starts with thorough risk analyses during the design phase, where potential hazards are identified and assessed. Implementing robust controls during manufacturing is vital to mitigate these risks, while continuous monitoring of device performance post-launch helps identify any emerging safety concerns.
In 2025, significant attention has been directed towards safety initiatives within the Medtech sector, emphasizing the need for proactive measures. For instance, the FDA has underscored the importance of prompt reporting of adverse events, noting that over 1.2 million reports were not submitted within the necessary 30-day deadline, raising serious safety concerns. Furthermore, a study revealed that nearly a third of adverse event reports were submitted late, highlighting the critical need for improved reporting practices. The Cumberlege report has also pointed out the lack of informed decision-making regarding medical devices and surgical procedures, stressing the importance of comprehensive risk management.
Quotes from industry leaders reinforce this focus on safety for individuals:
Evaluating risks throughout the medical device life cycle is not just a regulatory requirement; it’s also a means to foster user trust. The FDA estimates that maintaining an active medical apparatus postmarket surveillance system would cost about $8 million per year, underscoring the financial implications of inadequate reporting and surveillance systems. By prioritizing individual safety and adhering to compliance standards, companies can significantly enhance health outcomes and cultivate a culture of safety within the healthcare ecosystem. This commitment to risk management ultimately leads to improved equipment performance and greater user satisfaction.
Moreover, it’s crucial to recognize that 73% of participants reported never receiving feedback on submitted reports, revealing a significant gap in the reporting process that can impact safety. Additionally, 82% of participants felt that all reporting methods were ineffective, which highlights the challenges faced in current reporting systems. The stakes are high, as studies have linked 1.7 million injuries and 80,000 fatalities to healthcare instruments, emphasizing the necessity for effective risk management strategies.
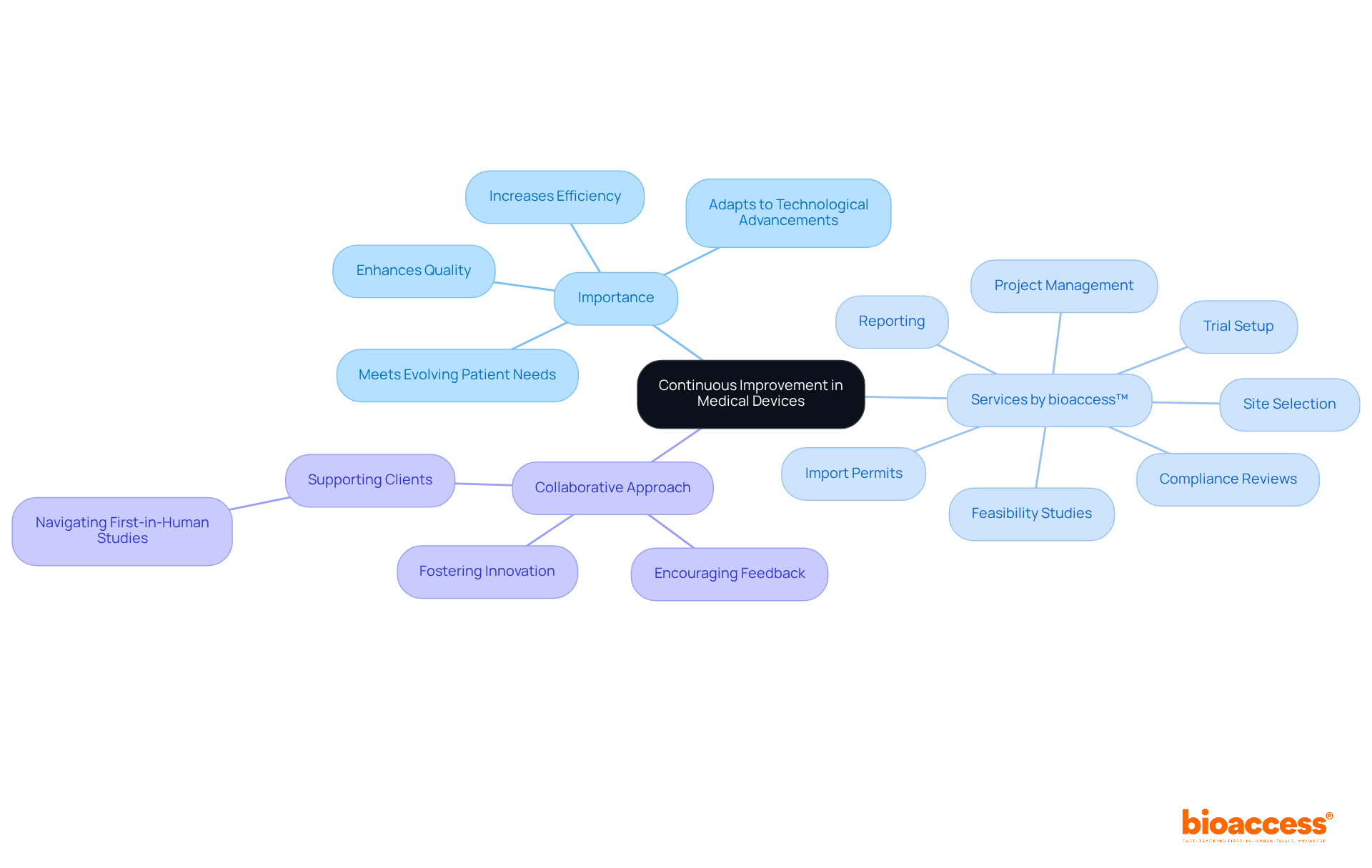
Continuous improvement is essential in the medical device industry, where regularly evaluating and refining processes, products, and services can significantly enhance quality and efficiency. This commitment is crucial for staying ahead of technological advancements, regulatory changes, and evolving patient needs. Companies like bioaccess™ exemplify this dedication through their comprehensive clinical trial management services, which encompass:
By fostering a culture of innovation and actively encouraging feedback from users and stakeholders, bioaccess™ not only drives enhancements but also supports clients like Avantec Vascular in navigating the complexities of first-in-human studies in Latin America. This collaborative approach is vital for addressing the unique challenges faced in clinical research today. How can your organization leverage such partnerships to improve outcomes?
Committing to continuous improvement allows organizations to maintain competitiveness and ensure long-term success in the market. By embracing this philosophy, companies can adapt to the ever-changing landscape of the Medtech industry, ultimately benefiting both their operations and the patients they serve.
The medical device life cycle is a critical journey that encompasses essential phases for the successful development and market introduction of innovative healthcare solutions. By understanding these phases-from identifying unmet medical needs to post-market surveillance-organizations can effectively navigate the complexities of Medtech. This ensures that new devices not only meet regulatory standards but also address real-world patient needs.
Throughout this article, we’ve provided key insights into each phase, underscoring the importance of thorough research, strategic planning, effective design, rigorous validation, and ongoing compliance. The roles of clinical trials, risk management, and continuous improvement are vital components that contribute to the overall success of medical devices. Moreover, partnerships with specialized organizations like bioaccess® can significantly enhance the efficiency and speed of the medical device life cycle, facilitating quicker market entry and ultimately improving patient outcomes.
As the Medtech industry continues to evolve, a steadfast commitment to innovation and quality must remain at the forefront of development strategies. Embracing a culture of continuous improvement and proactive engagement with regulatory changes will not only foster trust among users but also pave the way for future advancements in healthcare technology. Organizations are encouraged to leverage these insights and strategies to enhance their operations, ensuring they deliver safer, more effective medical devices to those in need.
What services does bioaccess® provide for clinical research in the Medtech sector?
bioaccess® offers rapid clinical research services including feasibility studies, research site selection, principal investigator selection, trial setup, startup, and thorough review of study documents to ensure compliance with country-specific requirements.
How quickly can bioaccess® secure ethical approvals for clinical trials?
bioaccess® can secure ethical approvals in an impressive 4-6 weeks, which is significantly faster than traditional markets.
How do bioaccess®'s services impact the medical device life cycle?
By providing rapid ethical approvals and enrollment rates that are up to 50% faster than traditional markets, bioaccess® significantly accelerates the medical device life cycle from initial concept to market entry.
What is the importance of the concept phase in the medical device life cycle?
The concept phase is crucial for identifying unmet health needs within the healthcare environment through thorough research and engagement with healthcare professionals, which helps innovators tailor solutions to address specific gaps in treatment or diagnosis.
How does bioaccess® support the concept phase?
bioaccess® supports the concept phase by offering clinical trial management services that include feasibility studies, site selection, compliance reviews, trial setup, and project management throughout the study.
What is involved in the planning phase of the medical device life cycle?
The planning phase involves creating a strategic roadmap that outlines project objectives, timelines, required resources, risk assessments, and contingency plans to guide the development process.
How does bioaccess® enhance the planning phase for clinical trials?
bioaccess® tailors the strategic roadmap for managing clinical trials, allowing for expedited official approval in just 6-8 weeks, which helps enroll treatment-naive cardiology or neurology groups 50% faster than Western sites.
Why is collaboration with bioaccess® beneficial for clinical research?
Collaborating with bioaccess® helps address key challenges in clinical research, enhances trial success, and ensures that new medical devices align with the actual demands of the healthcare system.