


The article presents effective strategies for treating reversible perfusion defects, underscoring the critical importance of:
These elements are pivotal in enhancing treatment outcomes, as they ensure tailored approaches, accurate diagnostics, and comprehensive care plans. Such meticulous attention to detail ultimately leads to improved patient satisfaction and health results, reinforcing the necessity of these strategies in clinical practice.
The landscape of reversible perfusion defect treatment is rapidly evolving, driven by innovative strategies and advanced technologies that promise to enhance patient outcomes. As healthcare providers refine their approaches, understanding the most effective methods becomes crucial for optimizing care. What are the key strategies that can transform the management of these conditions and ensure that patients receive the best possible treatment? This article delves into ten pivotal strategies that not only address the complexities of reversible perfusion defects but also pave the way for improved clinical practices and patient engagement.
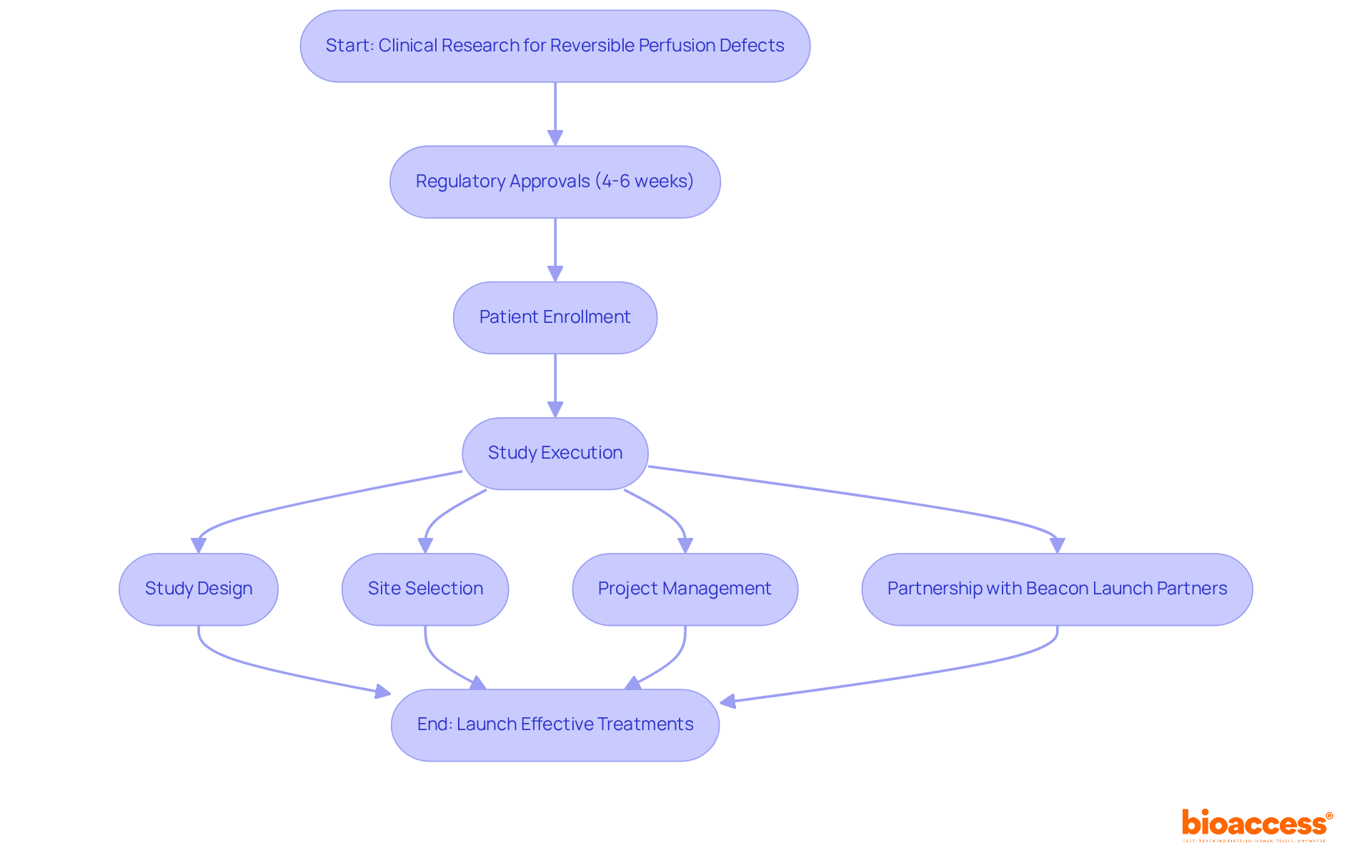
bioaccess® excels in accelerating clinical studies for reversible perfusion defect treatment by leveraging its strategic geographical advantages. The regulatory landscape in Latin America, the Balkans, and Australia allows bioaccess® to secure ethical approvals within an impressive timeframe of 4-6 weeks. This efficiency not only accelerates patient enrollment but also streamlines study execution, significantly reducing the average time to market for innovative therapies.
With an extensive range of services—study design, feasibility studies, site selection, compliance reviews, trial setup, import permits, project management, and reporting—bioaccess® plays a crucial role in advancing effective treatments for reversible circulation issues. The company’s partnership with Beacon Launch Partners enhances its expertise in managing early-feasibility and first-in-human studies, ensuring that Medtech and biopharma startups can navigate the complexities of clinical trials with confidence. Medtech leaders emphasize that regulatory speed is vital for maintaining a competitive advantage, as companies with top-quartile innovation scores experience 40% higher revenue growth than their peers.
Ongoing clinical research updates suggest promising results, including successful trials in Latin America. With its commitment to transforming the field for reversible perfusion defect treatment therapies, bioaccess® remains at the forefront of clinical research, ready to address the challenges faced by the industry.
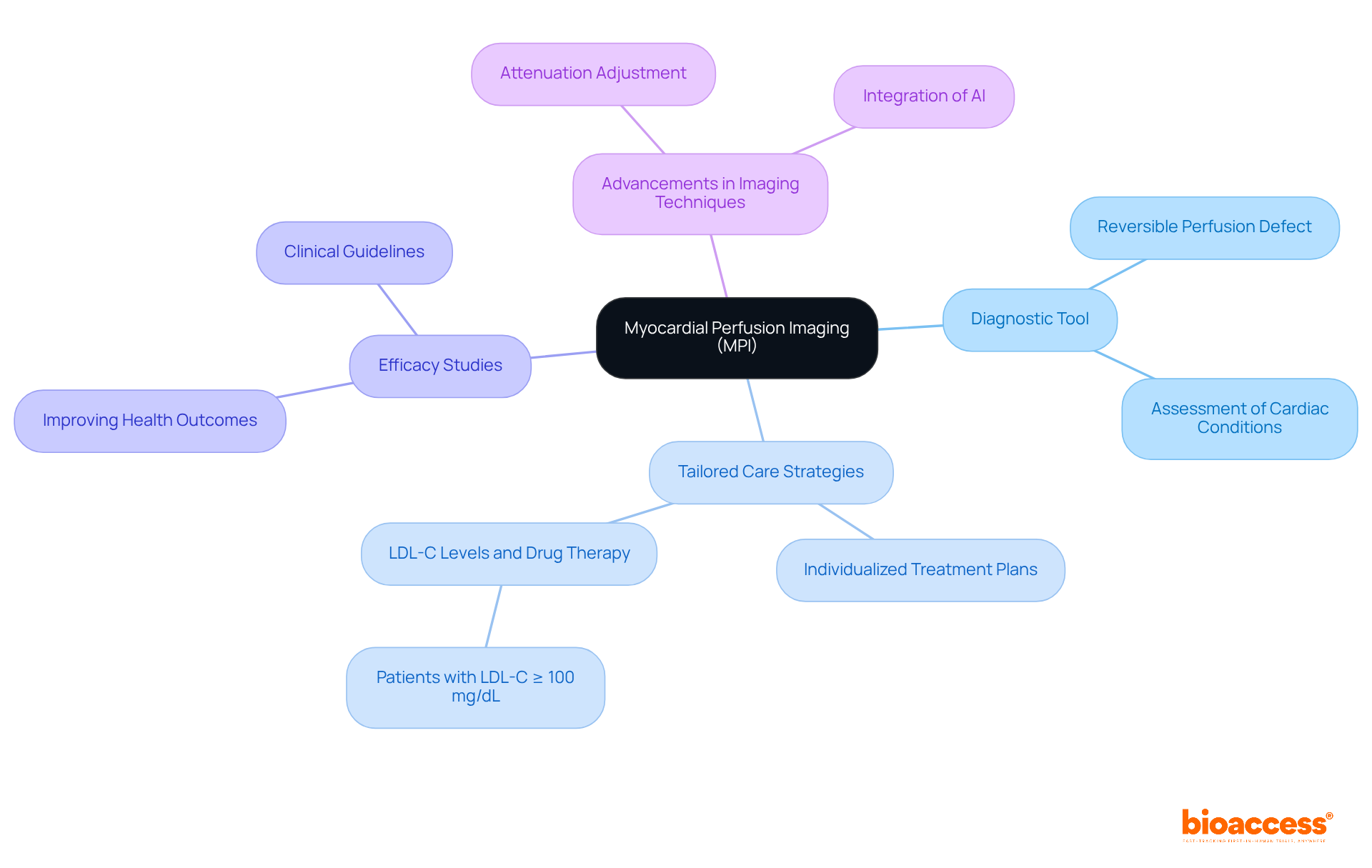
Myocardial blood flow imaging (MPI) serves as a critical diagnostic tool, offering comprehensive insights into circulation to the heart muscle. By pinpointing areas of reversible perfusion defect treatment, clinicians can tailor care strategies that meet specific individual needs. MPI plays a pivotal role in evaluating the severity of cardiac conditions and informs the selection of appropriate therapeutic interventions, ensuring that patients receive the most effective care aligned with their unique profiles.
Recent studies underscore the efficacy of MPI in improving health outcomes, with evidence indicating that patients with LDL-C levels of 100 mg/dL or higher should be prescribed drug therapy upon hospital discharge. Furthermore, the specialist agreement paper on CT myocardial flow imaging, published on March 16, 2020, highlights the essential role of MPI in contemporary cardiac care planning. As the field continues to evolve, the integration of advanced imaging techniques—particularly the crucial aspect of attenuation adjustment in nuclear myocardial blood flow imaging studies—further enhances the identification of reversible perfusion defect treatment. This evolution reinforces MPI's status as a fundamental component of effective cardiac care.
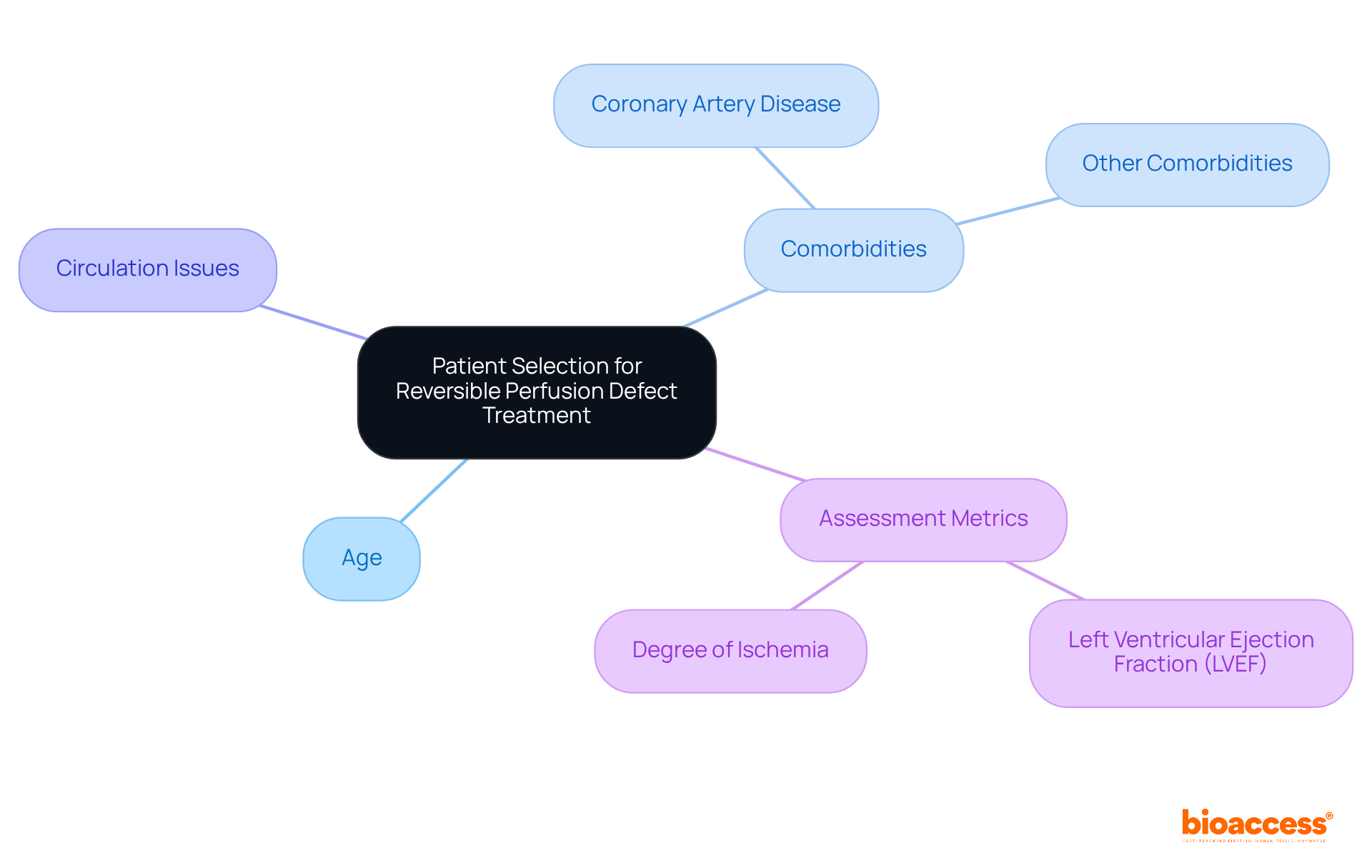
Efficient selection of individuals is essential for enhancing results in reversible perfusion defect treatment for circulation issues. Clinicians must assess factors such as age, comorbidities, and the extent of circulation issues to identify the most appropriate candidates for specific therapies. For instance, studies indicate that older individuals with significant comorbidities, such as coronary artery disease, often experience poorer outcomes, highlighting the need for tailored approaches. Significantly, 60% of individuals exhibited minor to moderate issues with blood flow, underscoring the commonality of these conditions within the group.
In clinical trials, effective selection criteria for individuals have encompassed the evaluation of left ventricular ejection fraction (LVEF) and the degree of ischemia, which are essential in forecasting responses to therapy. The existence of extensive perfusion defects has been recognized as an independent predictor of mortality at 12 months, with a hazard ratio of 2.90, emphasizing the significance of choosing individuals with considerable defects for reversible perfusion defect treatment. Moreover, individuals with significant reversible perfusion defect treatment had roughly three times greater risk of death at one year compared to those with smaller deficits, reinforcing the urgency of effective selection in improving outcomes.
Current best practices recommend a thorough assessment of demographics, as these factors greatly impact treatment effectiveness. By concentrating on individuals who are most likely to gain from interventions, healthcare providers can enhance clinical outcomes, minimize adverse effects, and ultimately boost satisfaction. Healthcare providers should regularly review patient demographics and comorbidities to ensure optimal patient selection.
Stress testing protocols are essential for assessing the efficacy of remedies related to reversible perfusion defect treatment. These protocols simulate physical exertion, enabling clinicians to monitor the heart's response under stress conditions. By examining pre- and post-intervention results, healthcare providers can effectively evaluate enhancements in myocardial perfusion, which is crucial for determining reversible perfusion defect treatment and making personalized modifications to care plans. This data-driven approach not only improves care for individuals but also aligns with current guidelines that promote stress testing as a standard procedure in cardiac management.
The integration of stress testing into clinical workflows has been shown to significantly improve treatment outcomes. Studies demonstrate that patients who undergo these evaluations experience better prognostic results and more personalized care strategies. This underscores the critical role of stress testing in advancing cardiac care and highlights the necessity for healthcare providers to incorporate these protocols into their practice.

Advanced imaging methods, particularly PET and SPECT, play a critical role in the management of reversible perfusion defect treatment. These modalities deliver high-resolution images that allow for precise localization of abnormalities related to reversible perfusion defect treatment, significantly enhancing diagnostic accuracy. Recent studies reveal that PET imaging achieves a sensitivity of 71.1%, surpassing SPECT's 51.7% (p<0.001), highlighting its superior diagnostic capabilities.
As nuclear medicine physician Remco Knol noted, "A key advantage of PET/CT is that you can quantify, which makes an important difference in cardiological evaluation." By integrating these advanced imaging technologies into clinical practice, healthcare providers can make more informed care decisions, ultimately leading to improved outcomes for patients.
Furthermore, these methods facilitate continuous monitoring of therapeutic effectiveness in reversible perfusion defect treatment, allowing for timely adjustments in care management. The evolution of PET and SPECT imaging continues to present promising solutions for the accurate assessment of cardiac conditions. Additionally, the effective radiation doses associated with PET imaging are significantly lower than those of SPECT, enhancing safety and comfort for patients.
Given that coronary artery disease impacts an estimated 15.4 million Americans, the importance of accurate diagnostic imaging in this domain cannot be overstated.

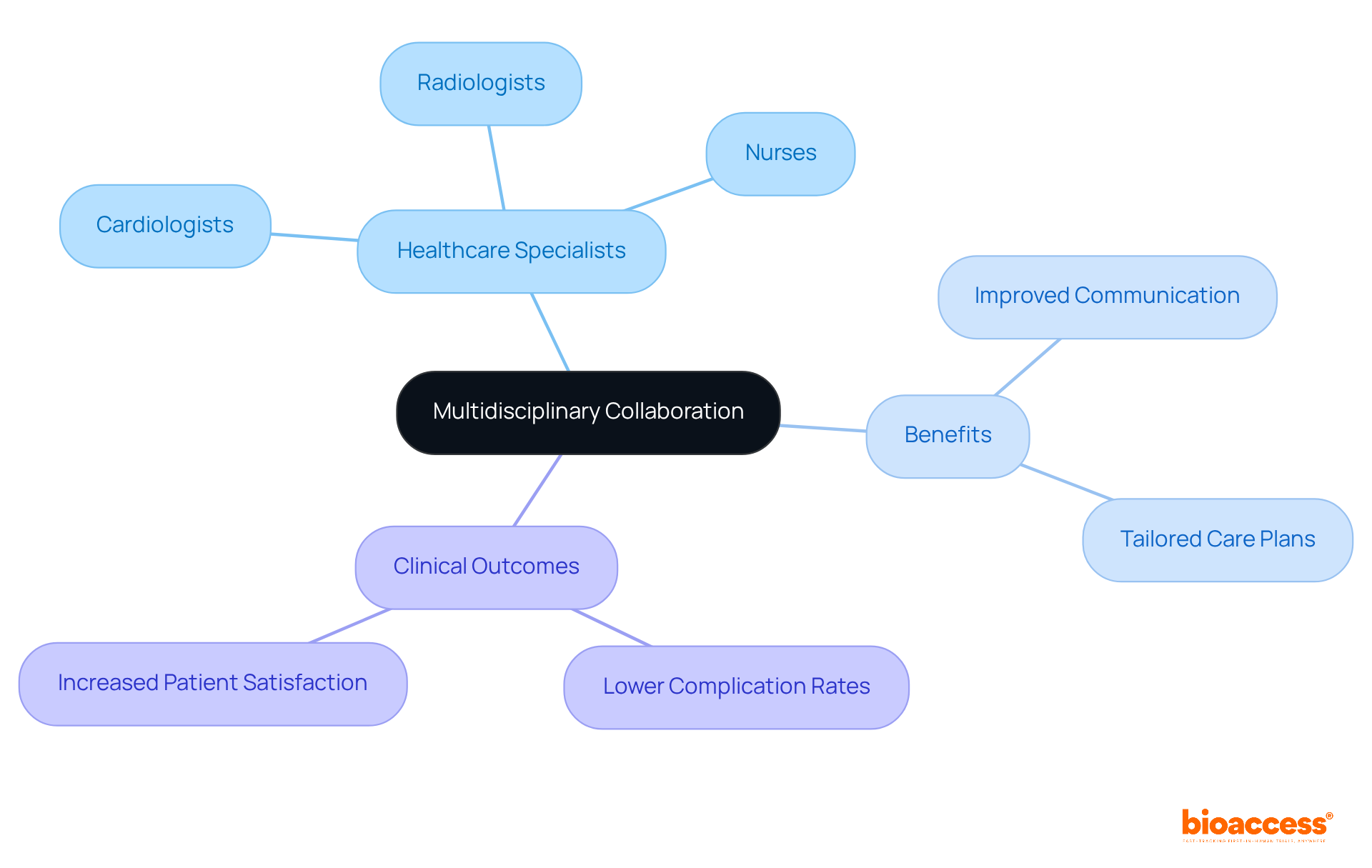
Multidisciplinary collaboration is paramount for enhancing strategies focused on reversible perfusion defect treatment. By engaging a diverse group of cardiologists, radiologists, nurses, and other healthcare specialists, we ensure a holistic approach to patient care. This collaborative structure fosters efficient communication and knowledge exchange, culminating in the development of comprehensive care plans tailored to the unique needs of each individual.
Recent studies reveal that such teamwork markedly improves clinical outcomes, evidenced by lower complication rates and heightened patient satisfaction. Programs that integrate various specialties have demonstrated effectiveness in refining care protocols, underscoring the power of collaborative efforts in tackling reversible perfusion defect treatment. By leveraging the strengths of each team member, healthcare professionals can elevate care strategies, ultimately enriching the overall patient experience.
Clinical trials play a pivotal role in advancing innovative reversible perfusion defect treatment. These studies rigorously assess the safety and effectiveness of new therapies, significantly contributing to the medical knowledge base. Recent trials have explored therapies such as gene therapy and novel pharmacological agents, which have shown promise in the context of reversible perfusion defect treatment and restoring myocardial perfusion. By participating in clinical trials, individuals gain access to groundbreaking therapies that may not yet be available through conventional care, enhancing their prospects for improved outcomes.
Furthermore, the collaboration between bioaccess™ and Caribbean Health Group, announced on March 29, 2019, during a meeting at PROCOLOMBIA's office in Miami, aims to establish Barranquilla as a premier destination for clinical trials in Latin America, with the support of Colombia's Minister of Health. This initiative not only enriches the clinical trial landscape but also expedites the recruitment process, achieving over a 50% reduction in recruitment time and an impressive 95% retention rate. bioaccess® provides essential services that facilitate regulatory approval, site activation, and participant recruitment, which are crucial for clinical research directors.
Current trends indicate a growing engagement in clinical trials for cardiac therapies, driven by increased awareness and the potential for personalized care options. This surge in participation accelerates the development of new therapies and fosters a collaborative environment where individual experiences inform future research directions. As clinical trials continue to shape innovations in cardiac care, their impact on improving outcomes for individuals undergoing reversible perfusion defect treatment remains profound.

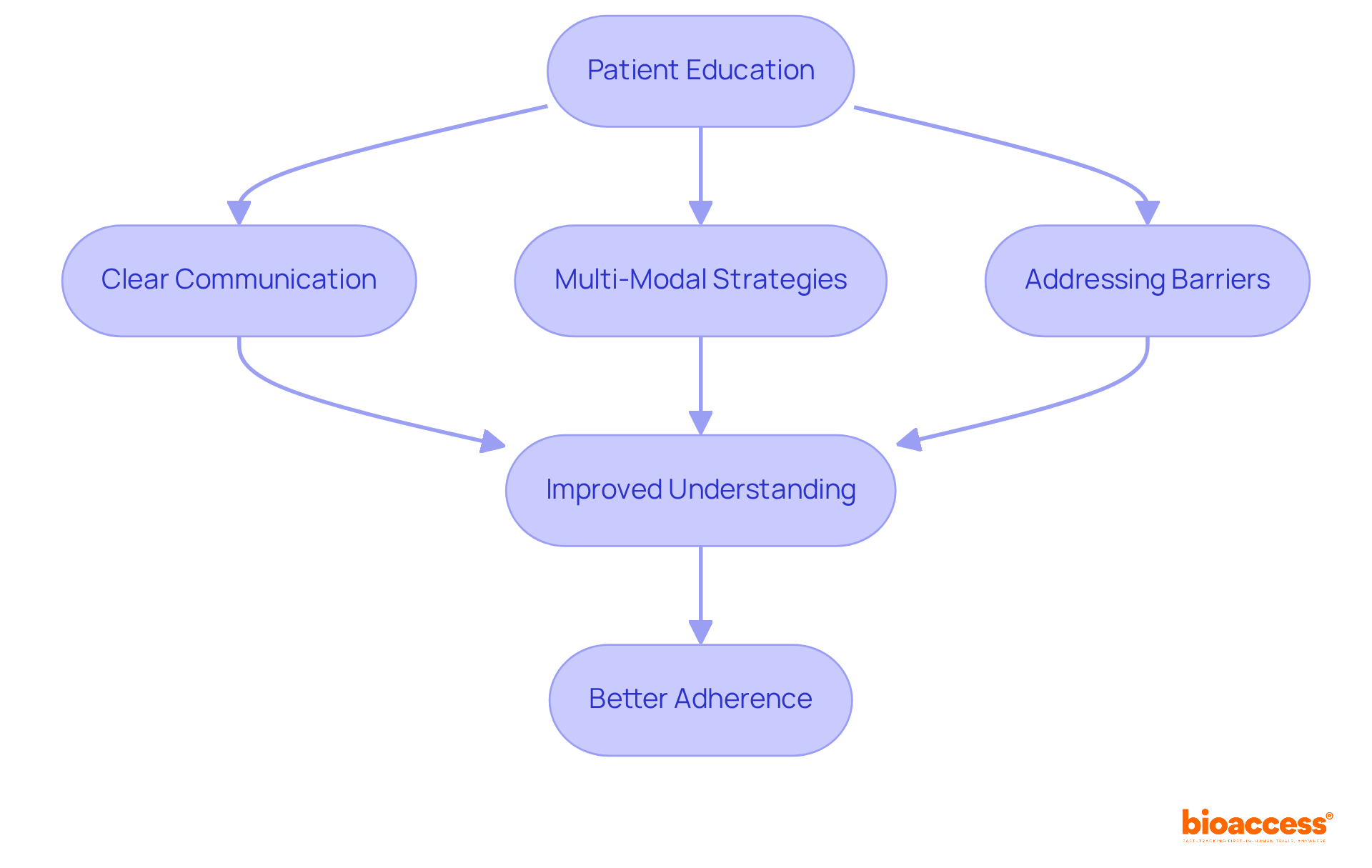
Patient education is crucial for the effective management of reversible perfusion defect treatment. By providing clear and understandable details about their condition and care alternatives, healthcare providers empower individuals to actively engage in their health management. Recent strategies underscore the importance of adhering to treatment plans, comprehending potential side effects, and implementing lifestyle modifications that foster overall health.
For instance, adherence rates for cardiovascular medications vary between 21% and 71%, emphasizing the necessity for impactful educational initiatives. Programs utilizing multi-modal strategies—such as personalized care plans, visual aids, and follow-up communications—have shown promise in enhancing understanding and engagement. Successful examples include interactive workshops and digital resources that significantly improve individuals' knowledge and compliance in managing their heart conditions.
Additionally, addressing adherence barriers, such as forgetfulness and low health literacy, is vital for improving outcomes. Care management initiatives like Chronic Care Management (CCM) and Advanced Primary Care Management (APCM) bolster these educational efforts, ensuring individuals receive the guidance necessary for reversible perfusion defect treatment and adherence to their care plans.
Follow-up care is essential for evaluating the effectiveness of interventions in the treatment of reversible perfusion defects. Frequent evaluations enable healthcare professionals to gauge individual progress and make necessary modifications to care plans. This ongoing monitoring can encompass:
By maintaining an active dialogue with individuals and adapting care as required, healthcare professionals can ensure optimal outcomes and enhance patient satisfaction.

Ongoing innovation is essential for enhancing approaches to reversible perfusion defect treatment. As emerging research and technological advancements reshape the landscape of cardiac care, healthcare providers must embrace adaptability and integrate novel approaches into their practices. This commitment to innovation not only improves care effectiveness but also ensures that individuals receive the most current, evidence-based assistance. By cultivating a culture of continuous improvement, healthcare teams can profoundly influence patient outcomes and elevate the overall quality of care.
Recent studies indicate that new imaging techniques and AI-driven analyses are revolutionizing the diagnosis and treatment of reversible perfusion defect treatment. This underscores the importance of staying informed about current trends in cardiac treatment innovations. Healthcare professionals are encouraged to leverage these advancements to enhance their clinical practices and improve patient care outcomes.

The treatment of reversible perfusion defects represents a multifaceted endeavor that necessitates a strategic approach to optimize patient outcomes. By integrating advanced methodologies such as bioaccess®'s efficient clinical trial processes, myocardial perfusion imaging, and multidisciplinary collaboration, healthcare providers can significantly enhance the management of these conditions. The emphasis on patient selection, stress testing, and continuous innovation underscores the importance of tailored care that responds to individual needs and emerging research.
Key insights from the article highlight the critical role of advanced imaging techniques and rigorous clinical trials in shaping effective treatment strategies. The integration of patient education not only empowers individuals to adhere to their treatment plans but also fosters a proactive approach to managing their health. Furthermore, the collaborative efforts among various healthcare professionals ensure a comprehensive understanding of each patient's unique circumstances, leading to improved clinical outcomes.
As the landscape of cardiac care continues to evolve, it is imperative for healthcare practitioners to remain informed about the latest advancements and best practices. By embracing innovation and focusing on patient-centered strategies, the potential for improved outcomes in the treatment of reversible perfusion defects is vast. Engaging in ongoing education and research initiatives will not only enhance individual patient care but also contribute to the broader field of cardiology, ultimately transforming the management of reversible perfusion defects.
What is bioaccess® and how does it contribute to clinical research for reversible perfusion defect treatments?
bioaccess® accelerates clinical studies for reversible perfusion defect treatment by utilizing strategic geographical advantages and securing ethical approvals within 4-6 weeks. This efficiency enhances patient enrollment and streamlines study execution, reducing the time to market for new therapies.
What services does bioaccess® offer for clinical research?
bioaccess® provides a range of services including study design, feasibility studies, site selection, compliance reviews, trial setup, import permits, project management, and reporting to advance effective treatments for reversible circulation issues.
How does bioaccess® collaborate with other organizations?
bioaccess® partners with Beacon Launch Partners to enhance its expertise in managing early-feasibility and first-in-human studies, helping Medtech and biopharma startups navigate the complexities of clinical trials.
Why is regulatory speed important in clinical research?
Regulatory speed is crucial for maintaining a competitive advantage, as companies with top-quartile innovation scores experience 40% higher revenue growth than their peers.
What role does Myocardial Perfusion Imaging (MPI) play in treatment planning?
MPI is a critical diagnostic tool that provides insights into blood flow to the heart muscle, helping clinicians tailor care strategies and evaluate the severity of cardiac conditions for appropriate therapeutic interventions.
What recent findings support the efficacy of MPI?
Recent studies show that patients with LDL-C levels of 100 mg/dL or higher should receive drug therapy upon hospital discharge, highlighting MPI's role in improving health outcomes.
What factors are important for patient selection in reversible perfusion defect treatment?
Important factors include age, comorbidities, and the extent of circulation issues. Effective selection criteria consider left ventricular ejection fraction (LVEF) and ischemia degree to forecast therapy responses.
What is the significance of extensive perfusion defects in patient outcomes?
Extensive perfusion defects are independent predictors of mortality, with individuals having significant defects at a three times greater risk of death within one year compared to those with smaller deficits.
How can healthcare providers enhance clinical outcomes in reversible perfusion defect treatment?
By thoroughly assessing patient demographics and comorbidities, healthcare providers can optimize patient selection, improve treatment effectiveness, minimize adverse effects, and increase patient satisfaction.