


The article delineates three pivotal strategies for effective recruitment in clinical trials:
Each strategy is substantiated by relevant examples and data, illustrating that a concentrated focus on demographics, the application of digital tools for outreach, and the cultivation of relationships with healthcare providers can significantly enhance participant acquisition and improve study outcomes. This approach not only addresses the complexities of clinical research but also underscores the necessity for collaboration among all parties involved.
The success of clinical trials hinges on effective recruitment strategies that bridge the gap between potential participants and groundbreaking research. By identifying target populations, leveraging technology, and fostering relationships with stakeholders, researchers can significantly enhance their recruitment efforts. However, with numerous variables at play, how can clinical trial teams ensure they are not only reaching the right people but also engaging them meaningfully? This article delves into three key strategies poised to transform clinical trial recruitment, offering insights that could reshape the future of medical research.
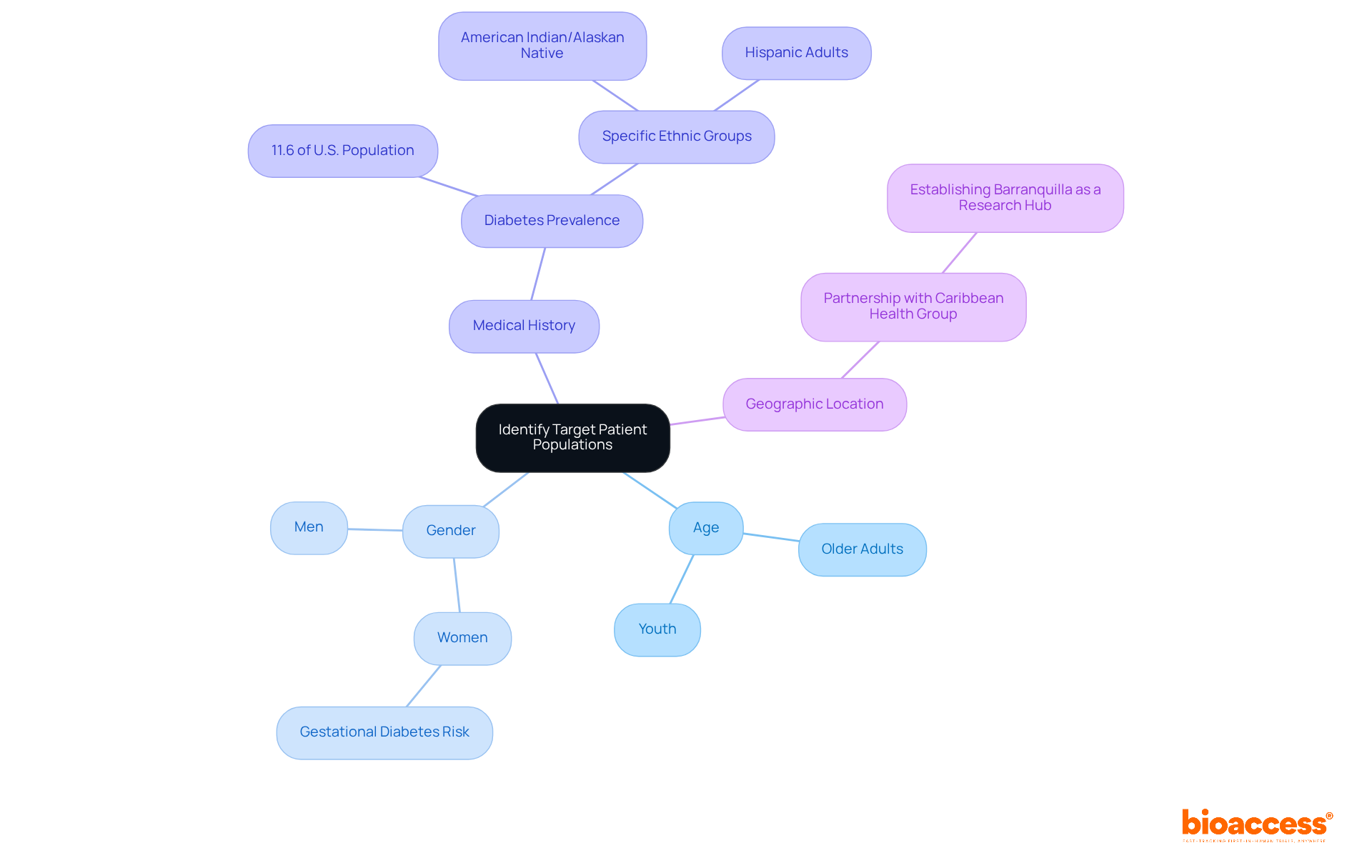
Identifying target groups is essential in clinical research, commencing with a comprehensive analysis of disease characteristics. Leveraging existing data from previous studies, registries, and healthcare databases is crucial for defining the ideal participant profile. Key factors to consider include:
Collaborating with healthcare providers and patient advocacy groups yields valuable insights into patient demographics. For instance, the partnership between bioaccess™ and Caribbean Health Group, revealed on March 29, 2019, during a meeting in Miami, FL, aims to establish Barranquilla as a premier location for clinical research in Latin America, supported by Colombia's Minister of Health. This strategic collaboration enhances the hiring process by promoting local involvement and awareness.
When conducting a study for a new diabetes medication, focusing on populations with a high prevalence of diabetes is vital, particularly older adults and specific ethnic groups. In the United States, approximately 38.4 million people had diabetes in 2021, representing 11.6% of the population, with significant prevalence among American Indian and Alaska Native adults. This focused hiring approach not only simplifies the enrollment process but also increases the likelihood of achieving significant outcomes from the study, ultimately enhancing the overall effectiveness of clinical research.
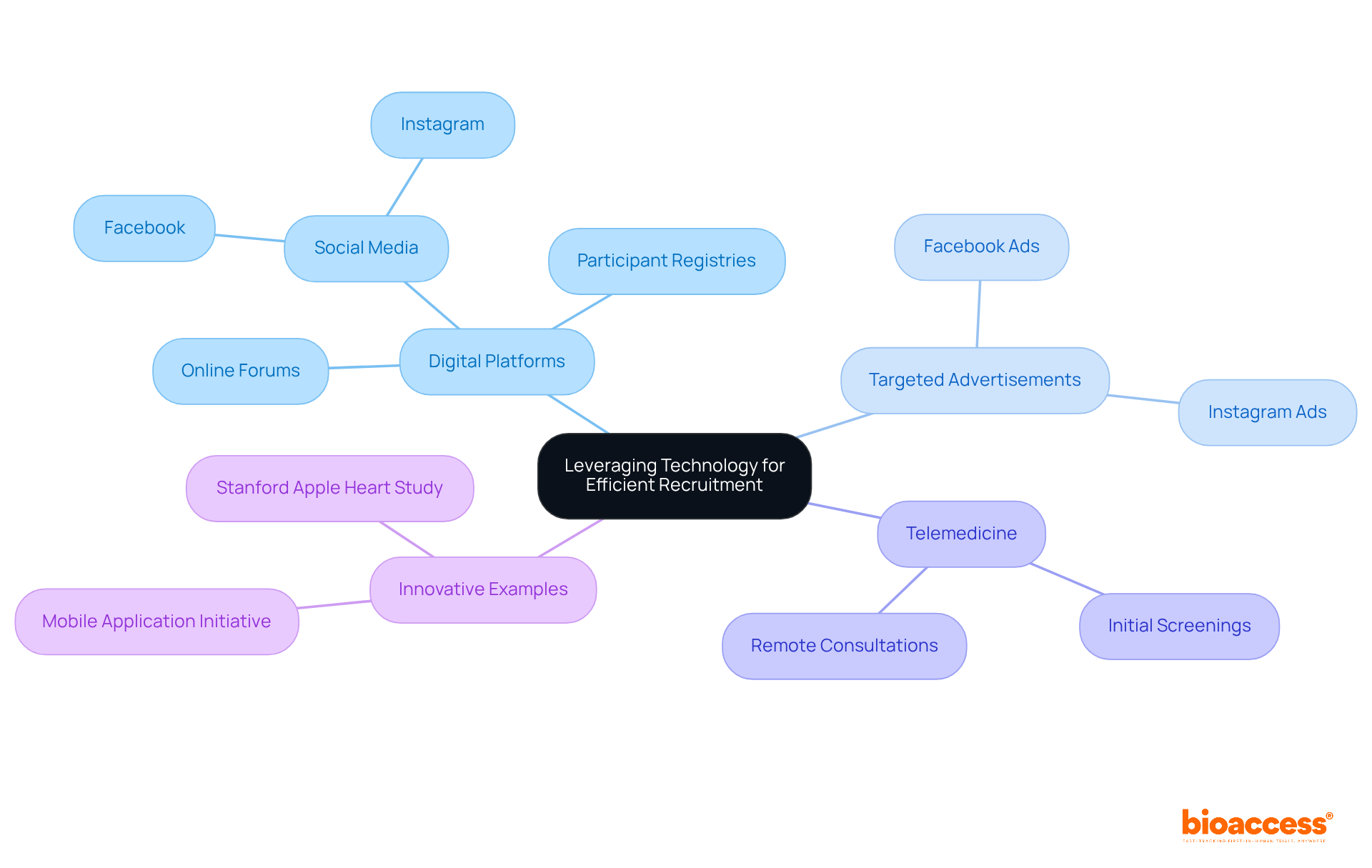
Employing technology is crucial for efficient clinical trials recruitment, particularly through digital platforms such as social media, participant registries, and online forums. Targeted advertisements on platforms like Facebook and Instagram enable researchers to efficiently reach specific demographics. Research indicates that 73% of patients prefer obtaining information about clinical studies from their healthcare providers, underscoring the importance of integrating social media engagement with traditional communication techniques. Furthermore, utilizing telemedicine for initial screenings significantly expands access and convenience for individuals, particularly for those residing far from trial locations—70% of potential participants live more than two hours away from an academic medical center.
A notable example is the Stanford Apple Heart Study, which successfully registered over 400,000 individuals using wearable technology, showcasing the potential for large-scale remote monitoring and data collection. Additionally, a recent initiative that utilized a mobile application for user engagement achieved a 30% increase in enrollment speed compared to traditional methods. By embracing these technological innovations, clinical trials recruitment can improve participant acquisition efficiency while fostering deeper engagement with individuals, ultimately leading to more successful outcomes.
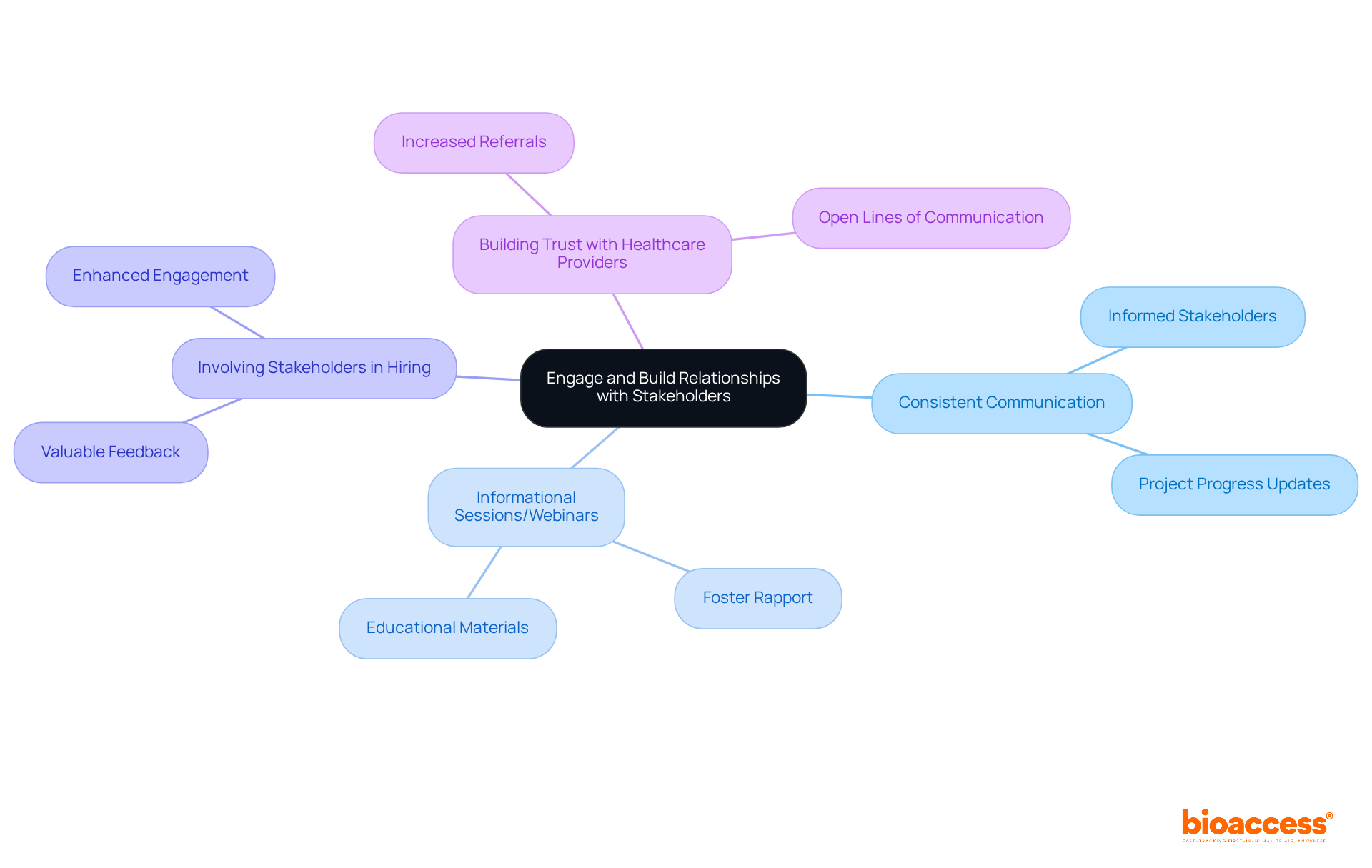
Engaging with stakeholders, particularly healthcare providers, is crucial for the successful clinical trials recruitment for clinical studies. Establishing consistent communication pathways ensures these stakeholders are informed about the project's progress and goals. Hosting informational sessions or webinars can significantly foster rapport and trust. A recent clinical study for a novel cancer treatment exemplifies this; it effectively engaged local oncologists by providing educational materials and timely updates, leading to a notable increase in referrals of eligible patients.
Furthermore, involving stakeholders in the hiring process not only yields valuable feedback but also enhances participant engagement. By nurturing these relationships, clinical trials recruitment can develop a supportive network that streamlines efforts and improves overall study outcomes. Effective communication with healthcare providers holds particular significance, as studies indicate that 80% of physicians prefer to refer individuals to familiar colleagues and research centers. This highlights the necessity of building trust and maintaining open lines of communication to facilitate patient enrollment.
Identifying and implementing effective strategies for clinical trials recruitment is essential for advancing medical research and improving patient outcomes. This article highlights three pivotal approaches:
Each strategy plays a crucial role in enhancing recruitment efforts, ensuring that clinical trials can meet their objectives and contribute valuable insights to the medical community.
The first strategy emphasizes the importance of understanding patient demographics and characteristics, allowing researchers to focus their efforts on populations that are most relevant to their studies. The second strategy showcases how technology, such as social media and telemedicine, can streamline the recruitment process, making it easier to reach potential participants. Lastly, engaging with stakeholders, particularly healthcare providers, fosters trust and facilitates communication, ultimately leading to increased referrals and participant engagement.
In conclusion, the successful recruitment of participants for clinical trials hinges on a multifaceted approach that combines targeted outreach, technological innovation, and strong stakeholder relationships. By adopting these best practices, researchers can not only improve enrollment rates but also enhance the quality and effectiveness of their studies. Embracing these strategies is vital for the future of clinical research, as it ensures that trials reflect diverse patient experiences and ultimately lead to breakthroughs in healthcare.
Why is identifying target patient populations important in clinical research?
Identifying target patient populations is essential in clinical research as it allows for a comprehensive analysis of disease characteristics and helps define the ideal participant profile for studies.
What factors should be considered when identifying target patient populations?
Key factors to consider include age, gender, medical history, and geographic location.
How can collaboration with healthcare providers and patient advocacy groups benefit clinical research?
Collaborating with healthcare providers and patient advocacy groups provides valuable insights into patient demographics, which can enhance the recruitment and awareness of potential study participants.
Can you give an example of a collaboration aimed at improving clinical research?
An example is the partnership between bioaccess™ and Caribbean Health Group, which aims to establish Barranquilla as a premier location for clinical research in Latin America, supported by Colombia's Minister of Health.
Why is it important to focus on specific populations when studying new medications, such as diabetes treatments?
Focusing on populations with a high prevalence of diabetes, such as older adults and specific ethnic groups, simplifies the enrollment process and increases the likelihood of achieving significant outcomes, thereby enhancing the effectiveness of clinical research.
What was the prevalence of diabetes in the United States in 2021?
In 2021, approximately 38.4 million people in the United States had diabetes, representing 11.6% of the population, with significant prevalence among American Indian and Alaska Native adults.