


The article presents seven pivotal examples of biomedical devices that are revolutionizing patient care. These include:
Such innovations are not merely enhancements; they significantly elevate health monitoring, improve chronic disease management, and empower patients. By providing real-time data and facilitating timely medical interventions, these devices are transforming healthcare delivery and markedly enhancing patient outcomes.
Biomedical devices stand at the forefront of a healthcare revolution, fundamentally reshaping the delivery and monitoring of patient care. As technology advances, innovations—from wearable health trackers to sophisticated remote monitoring systems—present unprecedented opportunities to enhance patient outcomes and engagement. However, this rapid evolution raises a pressing question: how can healthcare providers ensure the effective integration of these devices into existing systems to truly transform patient care?
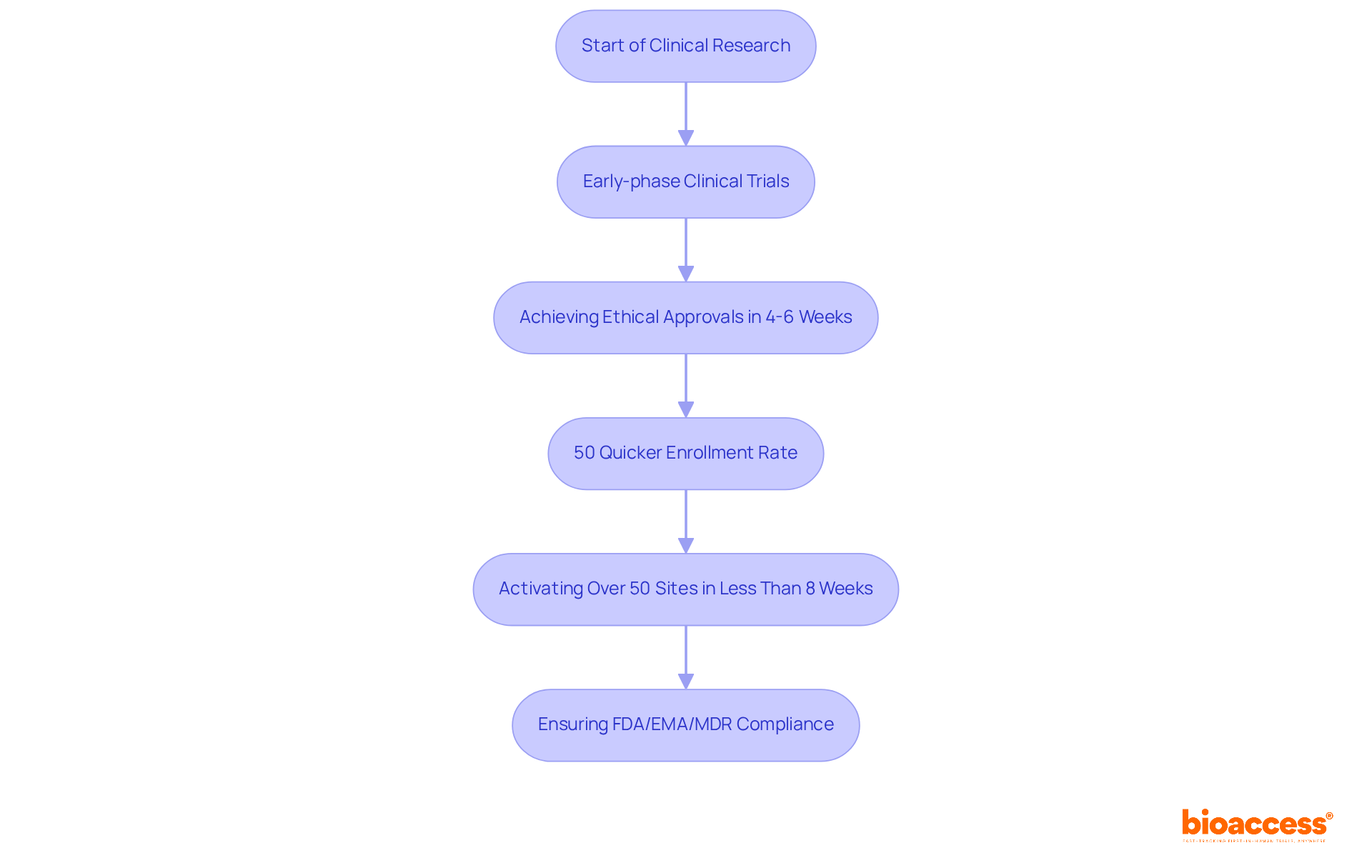
bioaccess® excels in accelerating clinical research for Medtech innovations by harnessing its deep understanding of regulatory landscapes. Specializing in early-phase clinical trials, the organization facilitates the swift transition of medical devices from concept to market, achieving ethical approvals in an impressive 4-6 weeks. This efficiency results in a 50% quicker enrollment rate for individuals compared to traditional markets, a crucial advantage for Medtech companies eager to deliver their innovations to recipients swiftly. Notably, bioaccess has activated over 50 sites in less than 8 weeks, ensuring FDA/EMA/MDR compliance across LATAM, Eastern Europe, and Australia, supported by FDA/EMA/MDR-ready datasets and centralized monitoring.
The significance of early-stage trials cannot be overstated; they are essential in validating ideas and ensuring that innovative technologies effectively meet user needs. The ability to navigate intricate regulatory landscapes is vital for promoting innovation and improving healthcare—a strength that bioaccess® distinctly provides. Collaborations with firms such as Welwaze Medical Inc. for the Celbrea® medical product launch in Colombia further exemplify bioaccess's role in streamlining market access and regulatory processes. This reinforces its commitment to fast, cost-effective, and high-quality research for Medtech and biopharma startups.
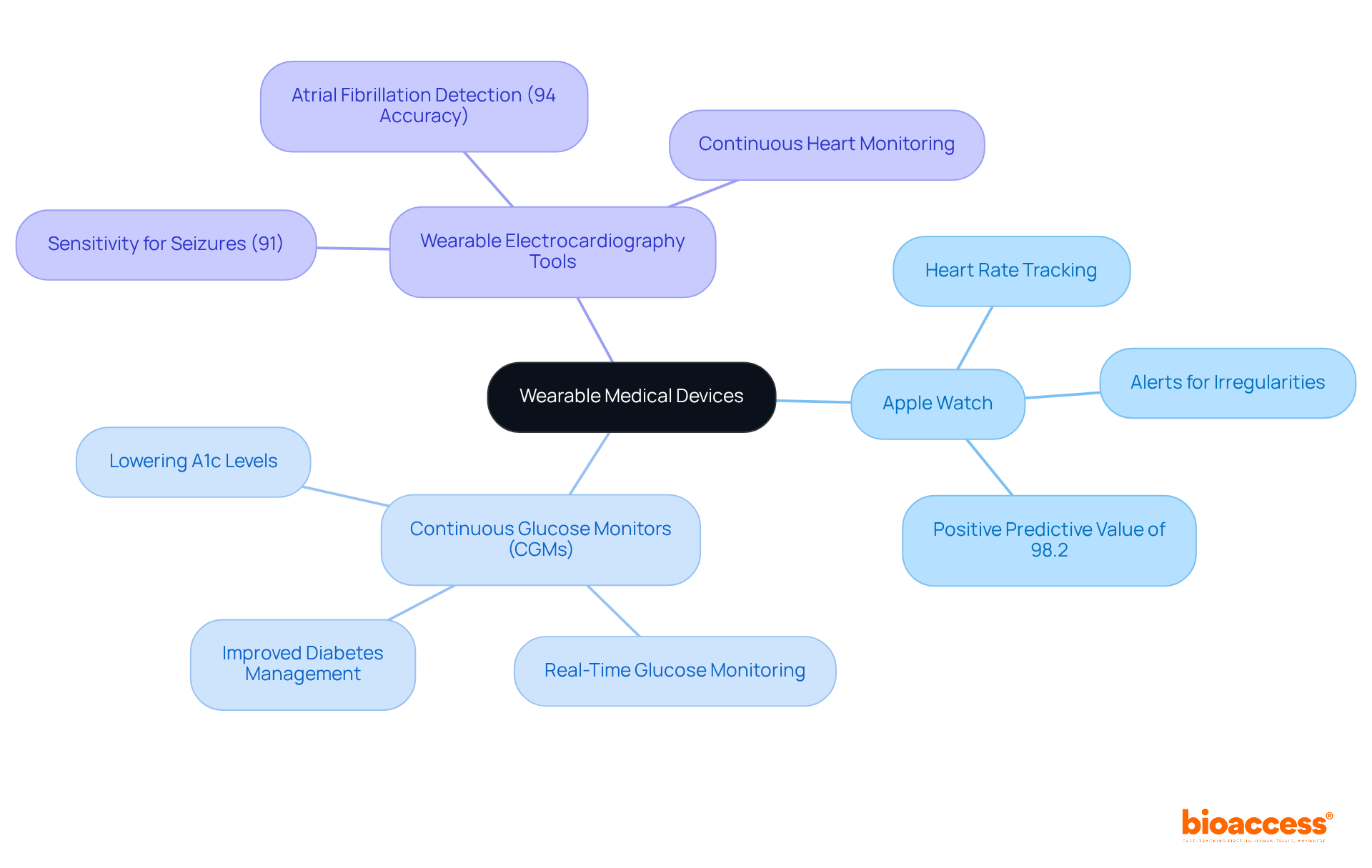
Wearable medical gadgets, such as smartwatches and fitness trackers, are revolutionizing patient observation and are considered examples of biomedical devices by providing immediate wellness information that significantly enhances proactive wellness management. These examples of biomedical devices are designed to monitor vital signs, activity levels, and sleep patterns, empowering users to take control of their well-being.
For instance, the Apple Watch not only tracks heart rate but also alerts users to irregularities, boasting a remarkable positive predictive value of 98.2% for identifying abnormal heart rhythms, which can potentially prevent serious medical issues. Continuous glucose monitors (CGMs) have been demonstrated to lower hemoglobin A1c levels in individuals with type 1 diabetes, showcasing their effectiveness in improving health outcomes.
Furthermore, wearable electrocardiography tools exhibit a sensitivity of 91% for detecting tonic-clonic seizures, underscoring their critical role in health monitoring. The integration of AI into these devices further amplifies their capabilities, enabling predictive analytics that inform both individuals and healthcare providers, with AI-assisted wearables achieving 94% accuracy in detecting atrial fibrillation. This technological advancement fosters personalized health insights, cultivating a more engaged and informed patient population.
However, potential barriers to adoption, such as perceived complexity and accessibility issues, must be addressed to fully realize the benefits of wearable devices. As wearable technology continues to evolve, its significance in chronic disease management and preventive care is anticipated to grow, establishing it as an essential element of modern healthcare.
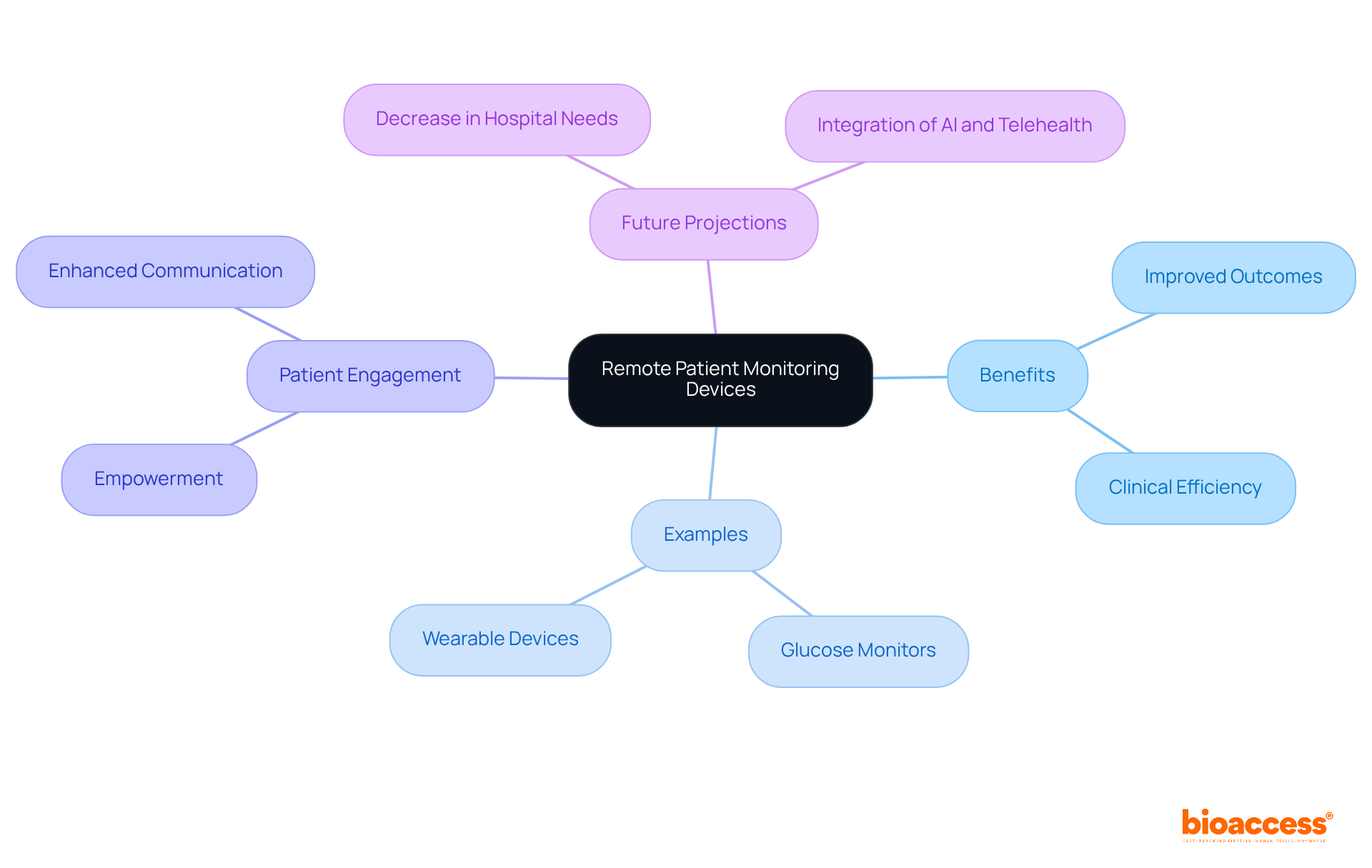
Remote health monitoring (RPM) tools are revolutionizing healthcare delivery by enabling providers to monitor individuals' health metrics remotely. These tools are particularly effective for managing chronic conditions such as diabetes and hypertension, providing continuous data that facilitates timely interventions.
For example, examples of biomedical devices include glucose monitoring devices that relay readings directly to healthcare providers, allowing for immediate adjustments to treatment plans and significantly improving outcomes for patients.
As Dr. Glen Stream notes, "We believe consumer wellness innovations — applications, wearables, self-assessment tools — hold the potential to enhance the patient-physician relationship and improve wellness results."
The convenience of RPM not only boosts clinical efficiency but also promotes greater patient engagement, empowering individuals to take charge of their health from the comfort of their homes.
With advancements in telehealth, it is projected that by 2030, the need for hospitals may significantly decrease, underscoring the importance of integrating RPM systems for delivering personalized, proactive care.
To successfully implement RPM systems, healthcare providers should invest in training and resources that support the adoption of these innovative solutions.
Blood pressure cuffs serve as essential instruments for monitoring cardiovascular health, with recent advancements in digital technology significantly enhancing their functionality. Modern digital cuffs not only provide accurate readings but also incorporate capabilities for data sharing with healthcare providers. Innovations such as smart cuffs that connect with mobile applications empower individuals to track their blood pressure over time and seamlessly share this information with their doctors. This continuous monitoring is crucial for managing conditions like hypertension, where timely adjustments to treatment can lead to improved outcomes for patients.
As Tammy M. Brady, M.D., Ph.D., states, "Through collaborative efforts and continued research, nurses can lead the way in realizing the full potential of cuffless blood pressure monitoring, ultimately advancing cardiovascular healthcare delivery."
Furthermore, integrating these tools into daily routines fosters greater engagement among individuals, encouraging proactive health management and adherence to treatment strategies. However, it is vital to acknowledge that while these technologies offer significant benefits, challenges regarding accuracy and validation persist, particularly for cuffless devices. Given that hypertension remains the leading preventable cause of cardiovascular disease, the necessity of precise monitoring cannot be overstated.

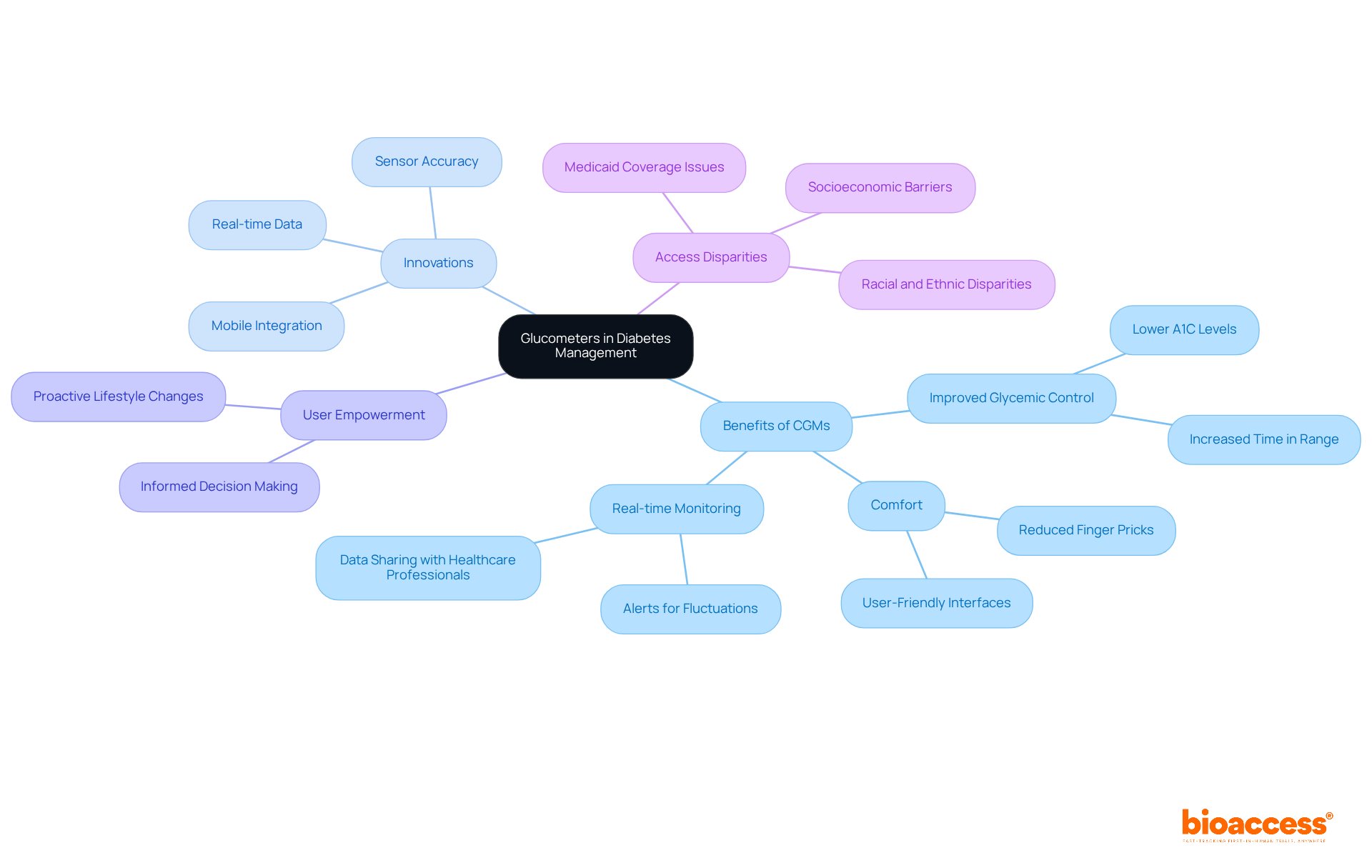
Glucometers are essential in diabetes management, facilitating real-time monitoring of blood glucose levels. The advent of continuous glucose monitors (CGMs) has revolutionized this domain, providing individuals with continuous data without the discomfort associated with frequent finger pricks. These sophisticated devices not only enhance user comfort but also significantly improve glycemic control by alerting users to fluctuations in their blood sugar levels. Research has demonstrated that individuals using CGMs experience improved time in range and lower A1C levels, leading to better overall health outcomes. For instance, one individual successfully reduced their A1C from 9.3% to 6.2% after adopting a CGM, illustrating the tangible benefits of this technological advancement.
The integration of mobile devices with CGMs allows users to effortlessly monitor their readings and share them with healthcare professionals, fostering a collaborative approach to diabetes management. Recent innovations in CGM systems, such as real-time data viewing and alerts, have enhanced user-friendliness and effectiveness. Consequently, healthcare professionals are increasingly recognizing CGMs as the new benchmark in diabetes care, underscoring their critical role in preventing serious complications related to hypo- and hyperglycemia.
Endocrinologists have noted that adopting CGMs empowers individuals to take control of their diabetes management, as they gain deeper insights into their glucose trends. This empowerment not only boosts adherence to treatment plans but also encourages proactive lifestyle changes. With ongoing advancements in CGM technology, including improved sensor accuracy and user interfaces, the future of diabetes management looks promising, paving the way for enhanced patient outcomes. However, it is crucial to recognize that access to CGMs is not equitable, particularly among marginalized groups such as poorer, older, Black and Brown Americans, and those on Medicaid. This disparity highlights the urgent need for improved coverage policies to ensure equitable access to this vital technology.
Pulse oximeters are important examples of biomedical devices that serve as essential tools for measuring blood oxygen saturation levels, playing a pivotal role in the management of respiratory conditions. These non-invasive tools provide immediate feedback on a person's oxygen levels, facilitating timely medical interventions.
Recent advancements in pulse oximetry technology, particularly the integration of artificial intelligence, have markedly improved their accuracy and accessibility, promoting widespread use in both clinical and home settings. For example, portable pulse oximeters are important examples of biomedical devices that empower individuals to monitor their conditions at home, ensuring they can swiftly seek medical assistance when necessary.
Innovations such as wireless connectivity and integration with mobile applications have further enhanced user engagement and data sharing with healthcare providers, ultimately improving the management of chronic respiratory conditions. Additionally, the FDA's proposed guidelines aimed at enhancing pulse oximeter accuracy for individuals with darker skin tones underscore ongoing efforts to address healthcare disparities.
The recent launch of the Pylo OX1-LTE unit by Prevounce Health in August 2024 exemplifies advancements in remote monitoring, highlighting the potential for improved care.

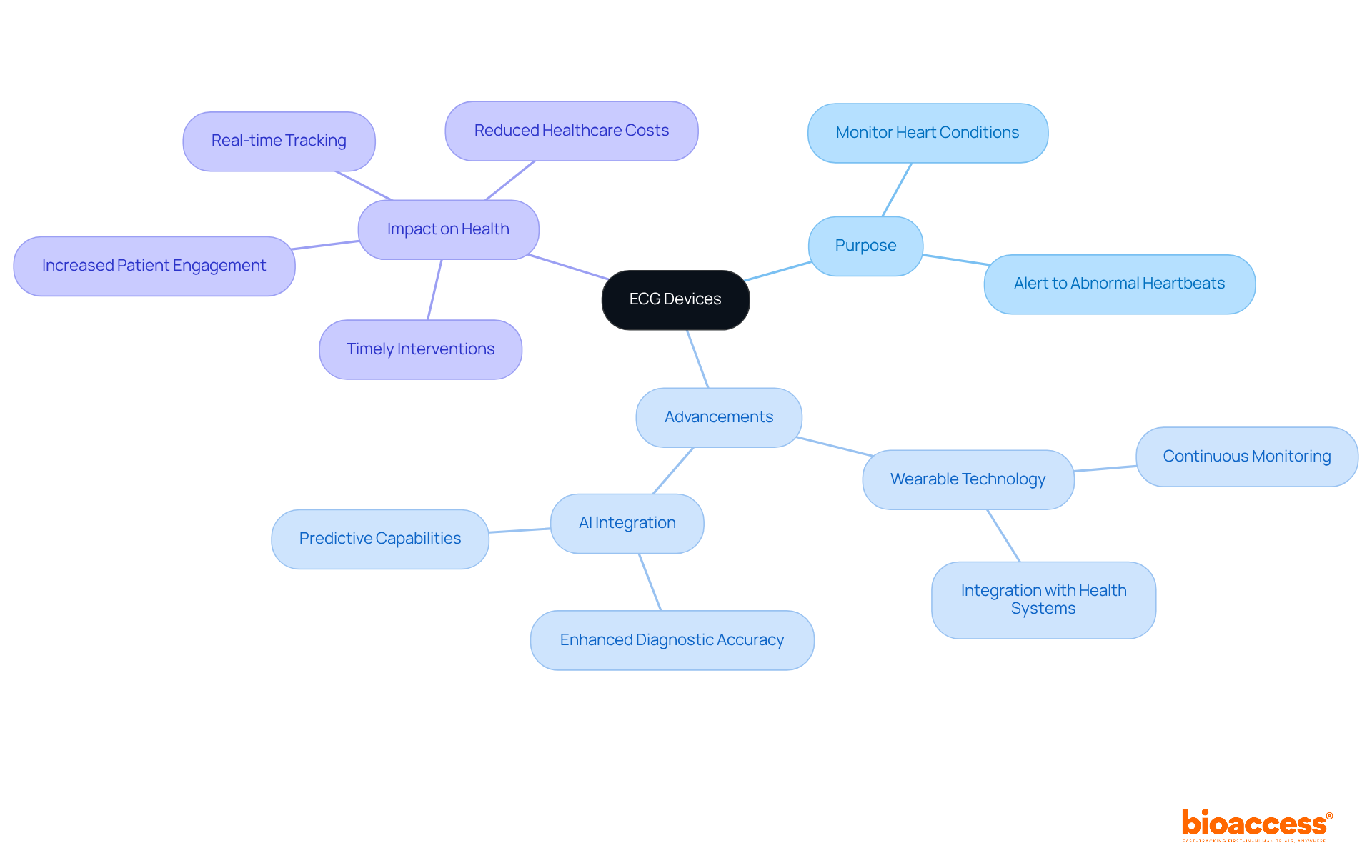
Electrocardiogram (ECG) instruments are essential for monitoring heart conditions, providing critical insights into heart rhythm and function. Recent advancements in wearable ECG technology now facilitate continuous monitoring, empowering patients to track their heart health in real-time. These devices can alert users to abnormal heartbeats, potentially preventing serious cardiac events.
Furthermore, the integration of AI in ECG analysis significantly enhances the accuracy of readings, enabling timely interventions. As a result, these innovations are transforming the landscape of modern cardiac care, underscoring their invaluable role in patient health management.
The transformative power of biomedical devices in patient care is evident through the various innovations discussed. These devices not only enhance monitoring capabilities but also empower patients to take charge of their health, ultimately leading to improved outcomes and a more proactive approach to healthcare.
Key examples, such as:
illustrate the significant strides made in technology. Each of these devices plays a crucial role in managing chronic conditions, facilitating timely interventions, and fostering a collaborative relationship between patients and healthcare providers. Moreover, organizations like bioaccess® are streamlining clinical research, ensuring that these innovations reach the market swiftly and efficiently.
Reflecting on the future of healthcare, it is clear that the integration of advanced biomedical technologies will continue to shape patient care significantly. As these devices become more accessible and user-friendly, they will not only enhance individual health management but also contribute to a more efficient healthcare system. Embracing these advancements is essential for both patients and providers to navigate the evolving landscape of modern medicine effectively.
What is bioaccess® and what does it specialize in?
bioaccess® is an organization that specializes in accelerating clinical research for Medtech innovations, focusing on early-phase clinical trials and facilitating the transition of medical devices from concept to market.
How quickly can bioaccess® achieve ethical approvals for clinical trials?
bioaccess® can achieve ethical approvals in an impressive timeframe of 4-6 weeks.
What advantage does bioaccess® provide in terms of enrollment rates for clinical trials?
bioaccess® achieves a 50% quicker enrollment rate for individuals compared to traditional markets, which is crucial for Medtech companies.
How many sites has bioaccess® activated, and in what timeframe?
bioaccess® has activated over 50 sites in less than 8 weeks.
What regions does bioaccess® ensure compliance with FDA/EMA/MDR regulations?
bioaccess® ensures compliance across LATAM, Eastern Europe, and Australia.
Why are early-stage trials important in clinical research?
Early-stage trials are essential for validating ideas and ensuring that innovative technologies effectively meet user needs.
Can you provide an example of bioaccess®'s collaboration with other firms?
An example is bioaccess®'s collaboration with Welwaze Medical Inc. for the launch of the Celbrea® medical product in Colombia.
What role do wearable medical devices play in patient monitoring?
Wearable medical devices, such as smartwatches and fitness trackers, revolutionize patient monitoring by providing immediate wellness information and empowering users to manage their health proactively.
How does the Apple Watch contribute to health monitoring?
The Apple Watch tracks heart rate and alerts users to irregularities, with a positive predictive value of 98.2% for identifying abnormal heart rhythms.
What impact do continuous glucose monitors (CGMs) have on individuals with type 1 diabetes?
CGMs have been shown to lower hemoglobin A1c levels in individuals with type 1 diabetes, improving health outcomes.
What is the sensitivity of wearable electrocardiography tools for detecting seizures?
Wearable electrocardiography tools exhibit a sensitivity of 91% for detecting tonic-clonic seizures.
How does AI enhance the capabilities of wearable medical devices?
AI integration enables predictive analytics, allowing wearables to achieve 94% accuracy in detecting conditions like atrial fibrillation and providing personalized health insights.
What barriers to adoption exist for wearable medical devices?
Potential barriers include perceived complexity and accessibility issues that need to be addressed to maximize the benefits of wearable devices.
What is the anticipated future significance of wearable technology in healthcare?
The significance of wearable technology in chronic disease management and preventive care is expected to grow, making it an essential element of modern healthcare.