


This article presents key insights into PET myocardial perfusion and its critical implications for clinical research and practice. It underscores the importance of advanced imaging techniques and innovations—such as artificial intelligence and new radiotracers—in enhancing diagnostic accuracy. These advancements play a pivotal role in improving patient outcomes, particularly in the assessment and management of coronary artery disease.
As healthcare professionals, how can we leverage these innovations to address the challenges we face in clinical settings? The collaboration between technology and clinical practice is essential for advancing patient care.
The landscape of PET myocardial perfusion imaging is rapidly evolving, driven by groundbreaking research and innovative technologies that promise to enhance diagnostic accuracy and patient outcomes. As the medical community increasingly recognizes the significance of myocardial blood flow assessment, understanding the complexities of conditions such as coronary microvascular dysfunction becomes paramount. Amidst these advancements, clinicians face a critical question: how can they effectively differentiate between epicardial and microvascular dysfunction to optimize treatment strategies? This article delves into seven key insights that illuminate the current state and future potential of PET myocardial perfusion, offering valuable perspectives for clinical research and practice.
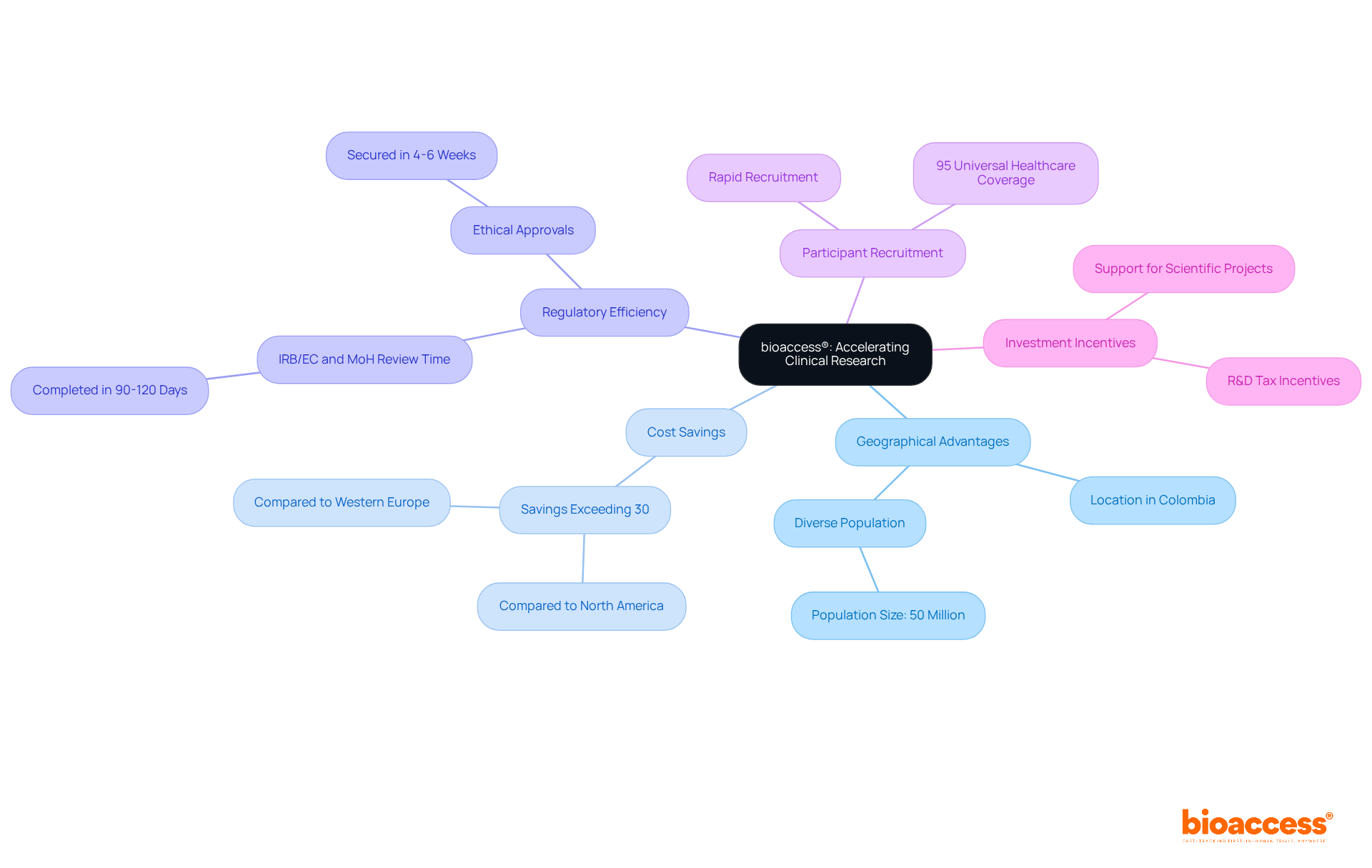
Bioaccess® effectively leverages its geographical advantages to accelerate clinical research for pet myocardial perfusion studies. Colombia emerges as a prime location, offering significant cost savings exceeding 30% compared to North America and Western Europe. Additionally, the regulatory process is notably swift, with the total IRB/EC and MoH (INVIMA) review completed in just 90-120 days. This efficiency is further bolstered by a diverse population exceeding 50 million, with 95% covered by universal healthcare, facilitating rapid participant recruitment.
By capitalizing on these strengths, bioaccess® secures ethical approvals in an impressive 4-6 weeks, substantially reducing overall timelines by up to 50% relative to traditional markets. Moreover, investments in scientific, technological, and innovative projects in Colombia are supported by substantial R&D tax incentives, enhancing the attractiveness of conducting clinical trials in the region.
This streamlined approach guarantees that cutting-edge technologies for PET myocardial perfusion reach patients more promptly, reinforcing bioaccess®'s commitment to delivering fast, cost-effective, and high-quality research for Medtech and biopharma startups.
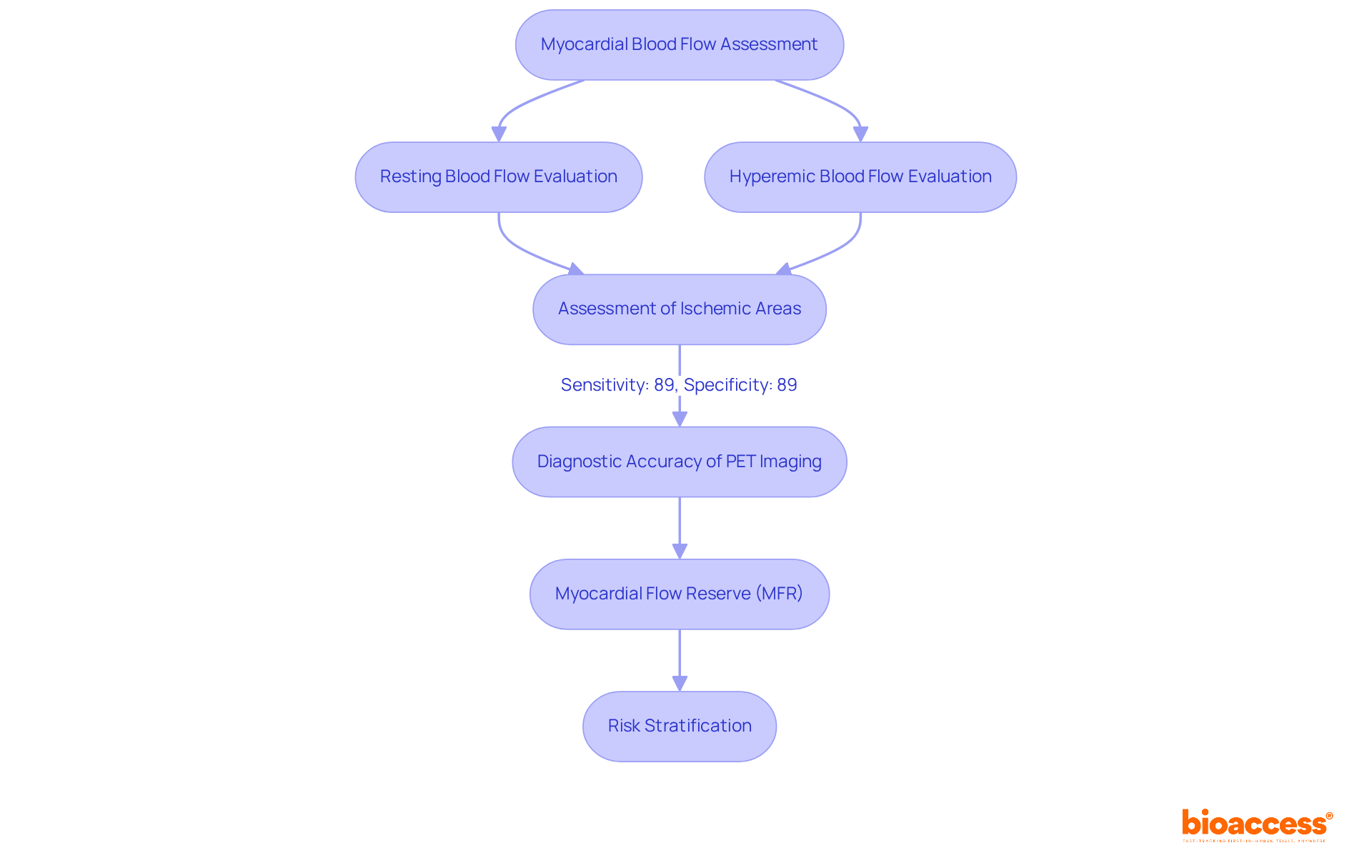
Evaluating pet myocardial perfusion through PET scans is crucial for identifying coronary artery disease (CAD), as it measures blood flow to the heart muscle. By utilizing radiotracers, PET scans visualize blood flow dynamics, allowing clinicians to assess both resting and hyperemic (stress-induced) blood flow. This dual evaluation is essential for recognizing ischemic areas and assessing pet myocardial perfusion reserve, which reflects the severity of artery blockages. Recent studies demonstrate that PET imaging offers superior diagnostic accuracy for CAD compared to traditional methods, with average sensitivity and specificity rates around 89% for detecting at least one coronary artery with ≥50% stenosis.
Moreover, the capability to measure myocardial flow reserve (MFR) enhances risk stratification, as lower MFR values correlate with adverse cardiac events. For example, a study involving over 900 individuals revealed that reduced MFR acts as an independent predictor of poor prognosis. The integration of advanced tracers such as fluorine-18-flurpiridaz, currently in phase III trials, holds promise for enhancing diagnostic capabilities in CAD detection. Additionally, the effective radiation dose for stress-rest rubidium scans in 3D mode could be reduced to approximately 1.85 mSv, a critical factor for safety considerations.
In summary, pet myocardial perfusion imaging emerges as a powerful tool in the clinical assessment of myocardial blood flow, significantly influencing management and outcomes.
Microvascular dysfunction (CMD) represents a critical challenge in cardiovascular health, characterized by impaired blood flow regulation within the heart's small vessels. This condition often leads to ischemic symptoms, even in the absence of significant epicardial artery disease. Various factors, including endothelial dysfunction, inflammation, and metabolic disturbances, contribute to the prevalence of CMD. Notably, studies reveal that CMD affects approximately 41% of patients experiencing chest pain with nonobstructive coronary artery disease, with women at a higher risk compared to men—54% prevalence in women versus 51% in men. This dysfunction can severely impact PET myocardial perfusion assessment, as it alters flow reserve measurements essential for accurate diagnosis.
Endothelial dysfunction is pivotal in the pathophysiology of CMD, significantly affecting blood vessels' ability to dilate properly. This impairment can lead to misinterpretations in PET scans, where the evaluation of PET myocardial perfusion may fail to accurately reflect underlying microvascular abnormalities. For instance, PET scans indicate that two-thirds of individuals with CMD exhibit some form of microvascular dysfunction, often disconnected from traditional noninvasive functional testing outcomes.
Research underscores that the presence of CMD can result in substantial discrepancies in PET myocardial perfusion imaging outcomes. This highlights the necessity for clinicians to account for microvascular abnormalities when interpreting results. As recent studies emphasize, understanding the mechanisms of CMD is essential for improving diagnostic precision and tailoring treatment approaches for individuals experiencing ischemic symptoms without obstructive heart artery disease. Furthermore, the average age of individuals with CMD is approximately 47 years, with a standard deviation of 10 years, and the prevalence of diabetes ranges from 7% to 12% among affected groups. This data underscores the importance of considering these factors during clinical evaluations.

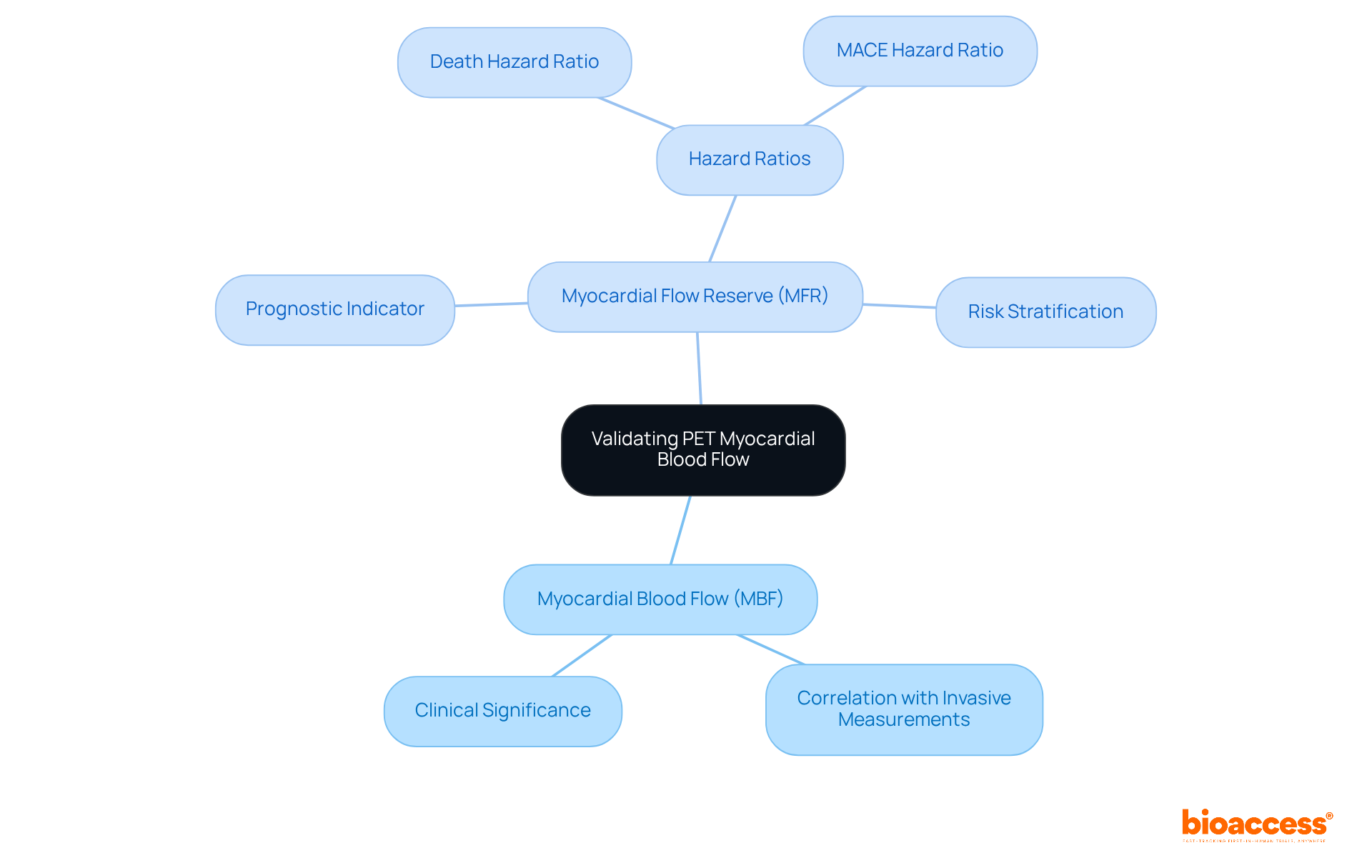
Validating pet myocardial perfusion and myocardial blood flow (MBF) necessitates a comprehensive comparison of PET measurements with established clinical outcomes. Research demonstrates a strong correlation between PET-derived MBF values and invasive measurements, affirming the reliability of PET myocardial perfusion in assessing cardiac health. MFR, defined as the ratio of hyperemic to resting MBF, serves as a critical prognostic indicator, enabling clinicians to effectively stratify risk in patients with suspected coronary artery disease (CAD).
Notably, studies reveal that for each 1 mL·g·min decrease in stress MBF, the adjusted hazard ratios for death and major adverse cardiovascular events (MACE) are 1.93 and 2.14, respectively. This underscores the significance of MFR in clinical decision-making. Furthermore, the pooled hazard ratio for adverse cardiovascular events in individuals with impaired MFR is reported at 2.19, indicating a markedly higher risk compared to those with preserved MFR. Such evidence advocates for the integration of MFR assessment into routine clinical practice, enhancing risk stratification and management strategies for individuals with CAD.
PET myocardial perfusion imaging plays a crucial role in diagnosing individuals with angina who do not exhibit obstructive artery disease (CAD) on angiography. In these instances, PET myocardial perfusion can uncover underlying cardiac microvascular dysfunction (CMD) by revealing reduced hyperemic myocardial blood flow (MBF). This ability is especially important, as research indicates that CMD is found in approximately 54% of individuals with symptoms, according to a study involving 239 symptomatic individuals. Significantly, CMD has been associated with heightened risks of adverse outcomes, including myocardial infarction and death, due to impaired PET myocardial perfusion, even in individuals without obstructive coronary atherosclerosis.
Furthermore, PET scans are essential for assessing individuals with heart failure, where CMD can exacerbate symptoms even with normal left ventricular function. Recent findings from a systematic review and meta-analysis highlight that 81% of hospitalized patients with heart failure with preserved ejection fraction (HFpEF) exhibit some form of CMD, underscoring the necessity for accurate diagnosis and management strategies. Cardiologists emphasize the importance of PET in these scenarios, advocating for increased awareness and utilization of this imaging technique to tailor treatment effectively. As one cardiologist noted, "Greater awareness among physicians of ischemia with no obstructive coronary arteries is urgently needed for proper diagnosis and patient-tailored management."
By identifying CMD through PET myocardial perfusion, clinicians can enhance management stratification, ultimately improving clinical outcomes and quality of life. Additionally, it is crucial to recognize that CMD prevalence varies by gender, with women being more frequently diagnosed, which may influence treatment approaches. The variability in diagnostic methods for CMD also calls for standardized reporting to enhance the accuracy of assessments and improve care for individuals.

Accurate diagnosis and treatment planning depend critically on distinguishing between epicardial and microvascular dysfunction. Positron Emission Tomography (PET) imaging plays a pivotal role in this process, allowing clinicians to assess both dysfunction types through the evaluation of myocardial blood flow (MBF) and myocardial flow reserve (MFR).
Typically, epicardial dysfunction is characterized by reduced MBF during stress testing, whereas microvascular dysfunction may present with preserved MBF but impaired MFR. This distinction is essential, as an abnormal MFR of less than 1.7 correlates with an increased risk of major adverse cardiovascular events.
Notably, research indicates that nearly 53% of individuals experiencing chest discomfort without obstructive coronary artery disease exhibit signs of inducible myocardial ischemia, underscoring the necessity for comprehensive evaluations. Alarmingly, almost two-thirds of individuals with nonobstructive coronary artery disease (CAD) may suffer from microvascular dysfunction (CMD), highlighting its prevalence and significance.
Furthermore, the average sensitivity of PET myocardial perfusion for detecting at least one coronary artery with over 50% stenosis is 90%, which reinforces the diagnostic accuracy of PET technology. By leveraging PET imaging to accurately identify these dysfunctions, healthcare providers can formulate targeted therapeutic strategies, ultimately enhancing outcomes for patients.
As researchers emphasize, individualized treatment strategies based on distinct disease endotypes are crucial for optimizing patient care.

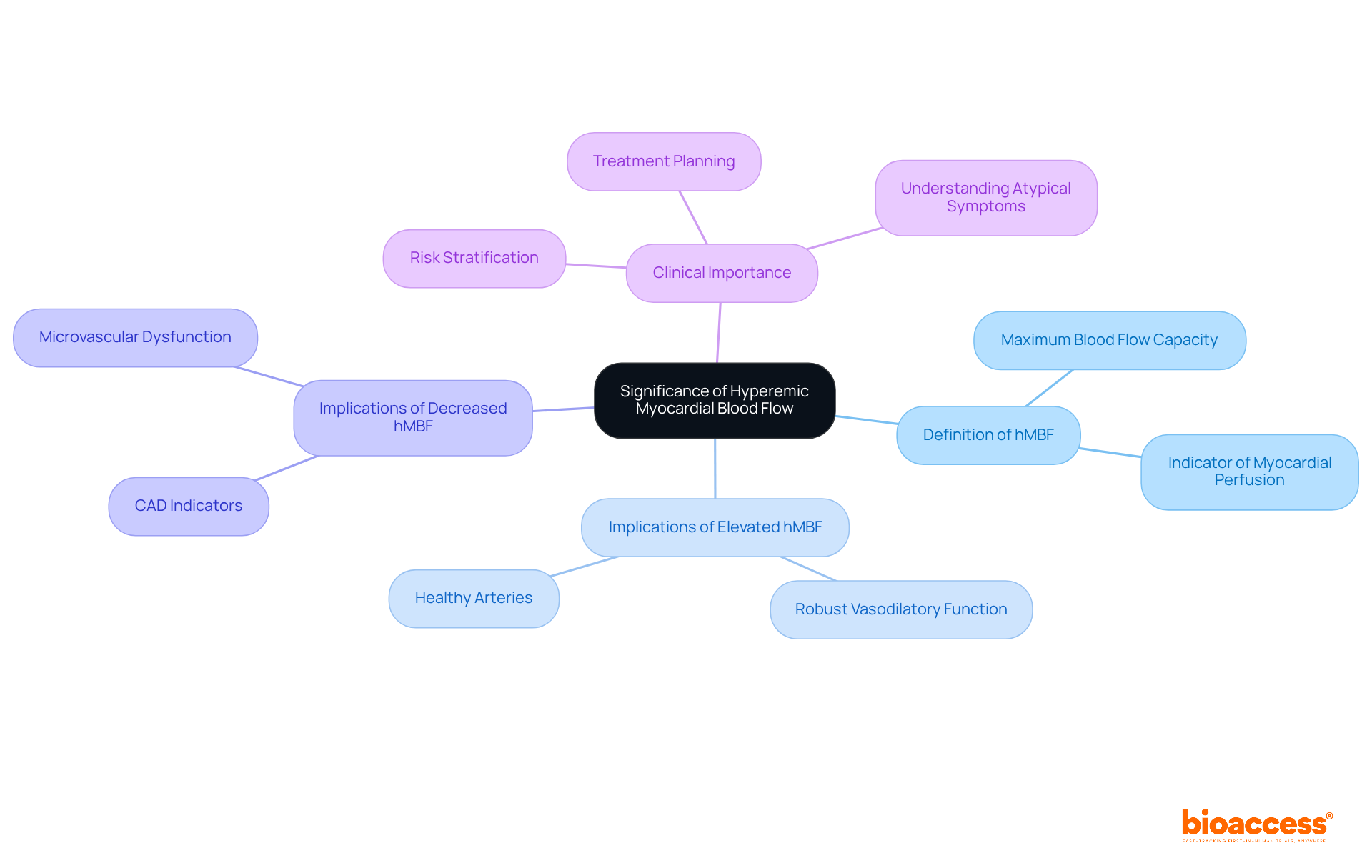
Hyperemic myocardial blood flow (hMBF) is a critical indicator of pet myocardial perfusion in positron emission tomography (PET) assessments, as it reflects the heart's maximum blood flow capacity during stress. Elevated hMBF is associated with robust vasodilatory function of the heart's blood vessels, signifying healthy arteries. Conversely, decreased hMBF may indicate significant artery disease (CAD) or microvascular dysfunction, necessitating comprehensive evaluation.
Accurate assessment of pet myocardial perfusion is essential for effective risk stratification and treatment planning in individuals suspected of having CAD. Research has shown that a hyperemic MBF below 2.65 mL/min/g correlates with reduced flow reserve (CFR), underscoring its significance in identifying individuals at risk for major adverse cardiovascular events (MACE).
Furthermore, cardiologists assert that a thorough understanding of hMBF dynamics can enhance clinical decision-making, particularly in populations presenting atypical symptoms or those without obstructive CAD. The relationship between hMBF and vascular dilatory function is paramount, as it aids not only in diagnosing CAD but also in informing treatment strategies aimed at improving outcomes for patients.
Assessing resting myocardial blood flow (rMBF) is crucial in PET scans, as it establishes a baseline for evaluating pet myocardial perfusion. Normal rMBF values typically range from 0.7 to 1.2 mL/g/min. Deviations from this range may indicate underlying cardiac conditions such as ischemia and heart failure. For instance, a study revealed that global rMBF at rest averaged 0.93 ± 0.42 mL/min/g, while global MBF during stress was 3.58 ± 1.14 mL/min/g. This highlights the significance of these measurements in clinical evaluations.
Clinicians utilize rMBF data and pet myocardial perfusion to assess cardiac health and determine the need for further diagnostic testing or interventions. Notably, elevated resting MBF has been associated with adverse cardiovascular outcomes, as indicated by the finding that 'Elevated Rest MBF was associated with increased cardiovascular outcomes.' This underscores the necessity for precise rMBF evaluations in managing patients undergoing pet myocardial perfusion. Furthermore, understanding normal rMBF values is essential for interpreting myocardial flow physiology, especially in diverse populations where demographic factors may influence these measurements.
Importantly, there was no significant difference in MBF between sexes at rest (p = 0.88) or during stress (p = 0.61). Ongoing research into rMBF values and their clinical implications remains vital for enhancing cardiovascular care. Additionally, the effective radiation doses for rest and stress examinations were approximately 4.16 ± 0.73 mSv and 4.22 ± 0.56 mSv, respectively, which are critical for clinical safety considerations. The intraclass correlation coefficients (ICC) for resting myocardial blood flow (rMBF) between fast and slow profiles ranged from 0.91 to 0.93, indicating the reliability of these measurements.

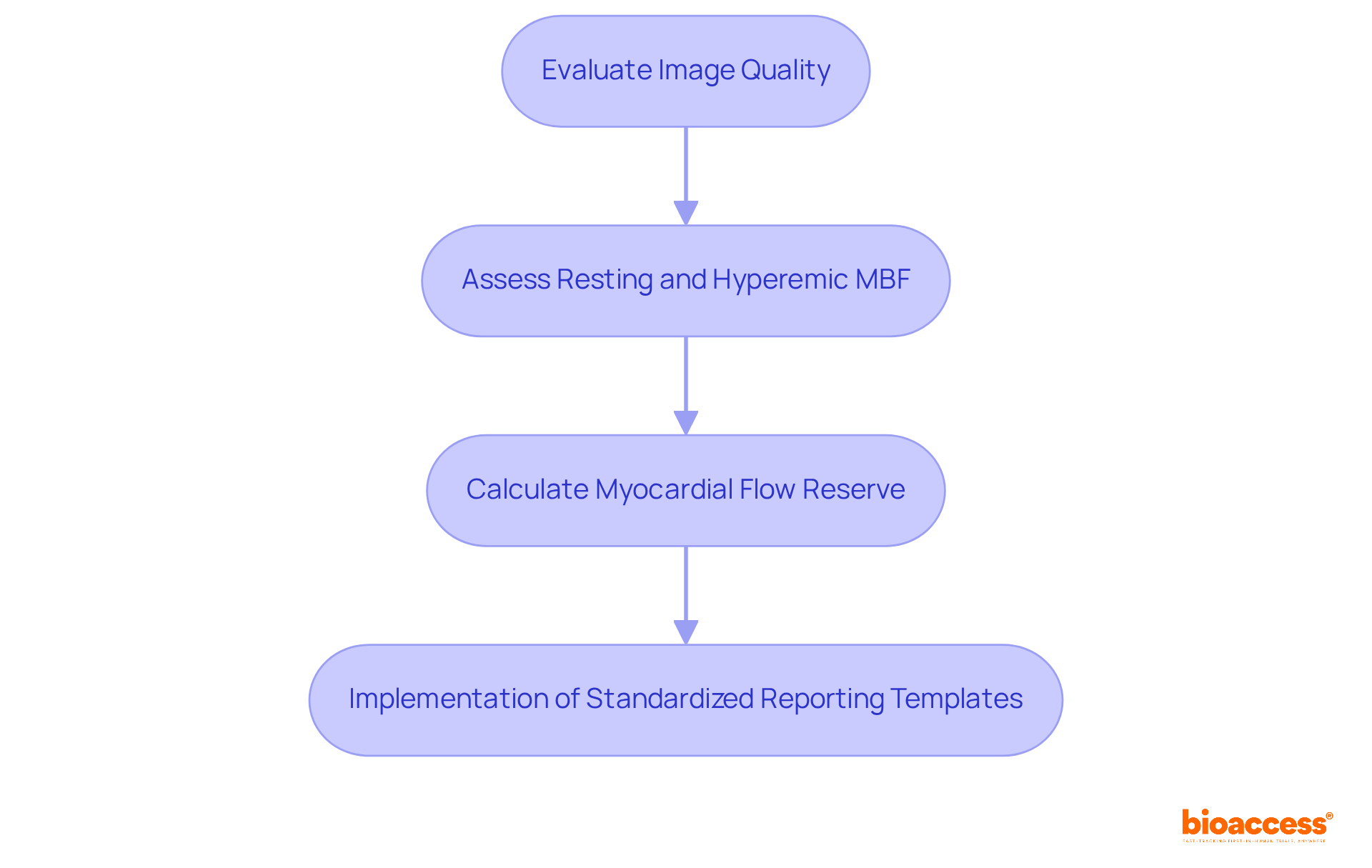
A systematic approach is required for interpreting and reporting PET myocardial perfusion imaging (MPI) results to ensure both accuracy and clarity. Clinicians must:
The implementation of standardized reporting templates is crucial for facilitating effective communication among healthcare providers, ensuring that essential information is conveyed clearly and concisely. This practice not only enhances clinical decision-making but also significantly improves care outcomes.
For instance, studies indicate that structured reporting can lead to a 49% increase in diagnostic accuracy and a notable rise in satisfaction among referring physicians, who rated the necessity of structured findings sections at 5.97 on a 7-point scale. Radiologists have expressed that structured reports enhance completeness and clarity, with their necessity rated at 6.07 on a 7-point scale.
Furthermore, the ISCHEMIA trial revealed a significant reduction in cardiovascular death in the invasive strategy arm (adjusted HR = .78 [95% CI: .63-.96]), underscoring the importance of accurate reporting in guiding treatment decisions. By adopting these best practices, healthcare professionals can optimize the interpretation and reporting of PET myocardial perfusion, ultimately benefiting patient management and outcomes.
Examples of structured reporting templates used in PET myocardial perfusion scans include those that standardize the assessment of MBF and MFR, which further enhances the clarity and utility of the reports.
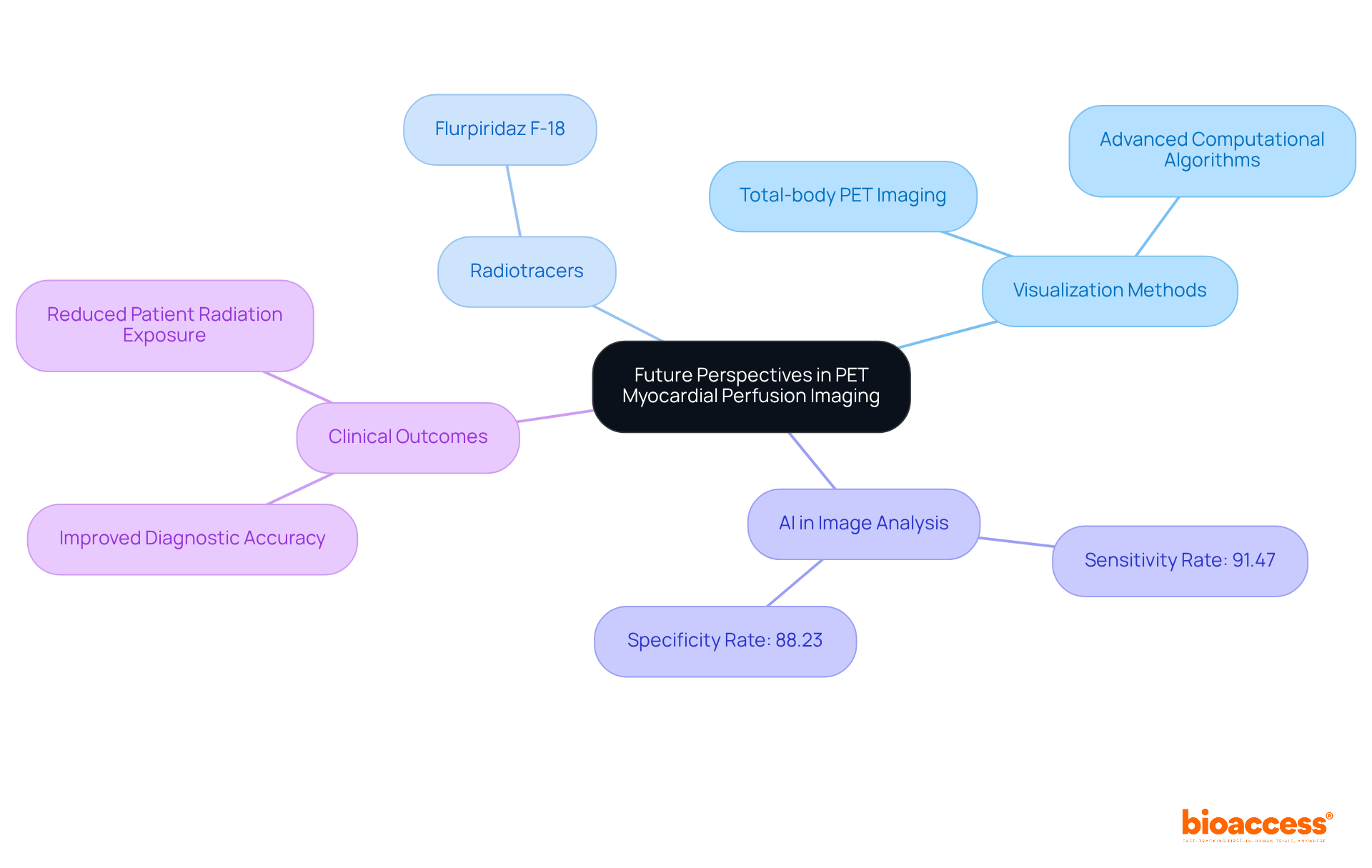
The future of pet myocardial perfusion scans is on the verge of significant advancement, propelled by ongoing research focused on improving visualization methods and creating new radiotracers. Innovations such as total-body PET imaging and advanced computational algorithms are expected to improve image quality and diagnostic accuracy.
The incorporation of artificial intelligence in image analysis is particularly revolutionary, optimizing workflows and facilitating the interpretation of complex datasets. Research indicates that AI applications can achieve combined sensitivity and specificity rates of 91.47% and 88.23%, respectively, in distinguishing conditions like heart artery disease.
These innovations are expected to enable more accurate assessments of pet myocardial perfusion, ultimately leading to better outcomes for patients managing coronary artery disease. As noted by leading researcher Marcelo Di Carli, "many of the challenging quantitative tasks will continue to be simplified and automated by artificial intelligence."
The advancement of radiotracers, such as Flurpiridaz F-18, underscores a commitment to improving diagnostic capabilities while reducing patient radiation exposure. The synergy of these innovations is likely to redefine clinical practices in cardiac imaging, empowering healthcare providers to deliver more effective and timely interventions.
The exploration of PET myocardial perfusion imaging offers essential insights into its significance in clinical research and patient care. By leveraging advanced technologies and methodologies, bioaccess® has established itself as a leader in facilitating efficient and cost-effective clinical trials within this domain. The advantages of conducting research in Colombia—including reduced costs and expedited regulatory processes—underscore the potential for accelerated access to innovative treatments for patients.
Key insights from the article emphasize the critical role of myocardial blood flow assessments in detecting coronary artery disease and understanding microvascular dysfunction. The capacity to distinguish between epicardial and microvascular issues through PET imaging is vital for accurate diagnosis and effective treatment planning. Moreover, the integration of advanced radiotracers and artificial intelligence is poised to significantly enhance diagnostic capabilities and improve patient outcomes.
As the field of PET myocardial perfusion imaging continues to advance, it is imperative for healthcare professionals to remain informed about the latest research and innovations. Embracing these advancements will not only enhance diagnostic accuracy but also ensure that patients receive timely and personalized interventions. The commitment to improving clinical practices through cutting-edge technology highlights the necessity of ongoing research and collaboration in advancing cardiovascular care.
What advantages does bioaccess® offer for clinical research in PET myocardial perfusion studies?
Bioaccess® leverages geographical advantages in Colombia, providing cost savings exceeding 30% compared to North America and Western Europe. The regulatory process is swift, with IRB/EC and MoH (INVIMA) reviews completed in 90-120 days, and ethical approvals secured in 4-6 weeks.
How does the population in Colombia contribute to clinical research for PET myocardial perfusion?
Colombia has a diverse population of over 50 million, with 95% covered by universal healthcare, which facilitates rapid participant recruitment for clinical trials.
What are the benefits of conducting clinical trials in Colombia according to bioaccess®?
Conducting clinical trials in Colombia is attractive due to significant cost savings, a fast regulatory process, and substantial R&D tax incentives that support scientific and innovative projects.
How does PET imaging assess myocardial blood flow?
PET imaging evaluates myocardial perfusion by using radiotracers to visualize blood flow dynamics, assessing both resting and stress-induced (hyperemic) blood flow, which is crucial for identifying coronary artery disease (CAD).
What is the diagnostic accuracy of PET imaging for coronary artery disease?
PET imaging offers superior diagnostic accuracy for CAD, with average sensitivity and specificity rates around 89% for detecting at least one coronary artery with ≥50% stenosis.
What is myocardial flow reserve (MFR) and why is it important?
Myocardial flow reserve (MFR) measures the capacity of blood flow to increase under stress conditions and is essential for risk stratification; lower MFR values correlate with adverse cardiac events.
What role does microvascular dysfunction (CMD) play in cardiovascular health?
Microvascular dysfunction (CMD) impairs blood flow regulation within small vessels of the heart, leading to ischemic symptoms even without significant epicardial artery disease, affecting approximately 41% of patients with chest pain and nonobstructive coronary artery disease.
How does CMD impact PET myocardial perfusion assessment?
CMD can alter flow reserve measurements essential for accurate diagnosis, leading to misinterpretations in PET scans, as it affects the blood vessels' ability to dilate properly.
What is the prevalence of CMD among different demographics?
CMD affects about 41% of patients with chest pain and nonobstructive coronary artery disease, with a higher prevalence in women (54%) compared to men (51%).
Why is it important for clinicians to consider CMD when interpreting PET imaging results?
Understanding CMD is crucial for improving diagnostic precision, as it can cause substantial discrepancies in PET myocardial perfusion imaging outcomes, especially in patients experiencing ischemic symptoms without obstructive heart artery disease.