


This article emphasizes the critical insights related to pharmacoeconomics that Clinical Research Directors must consider in their work. It underscores the necessity of integrating pharmacoeconomics into clinical trials, which is vital for enhancing decision-making, optimizing health outcomes, and securing funding. Such integration is not merely beneficial; it is essential for effectively navigating the evolving healthcare landscape. By recognizing the importance of pharmacoeconomics, Clinical Research Directors can better position their research within the broader context of healthcare needs and funding opportunities.
The landscape of clinical research is rapidly evolving, with pharmacoeconomics emerging as a crucial element in optimizing health outcomes and ensuring the economic viability of new therapies. By understanding the principles of pharmacoeconomics, Clinical Research Directors can navigate budget constraints while enhancing decision-making processes that impact patient care. However, as the demand for cost-effective solutions grows, a pressing question arises: how can these directors effectively integrate pharmacoeconomic evaluations into their research strategies to meet the challenges of an increasingly complex healthcare environment?
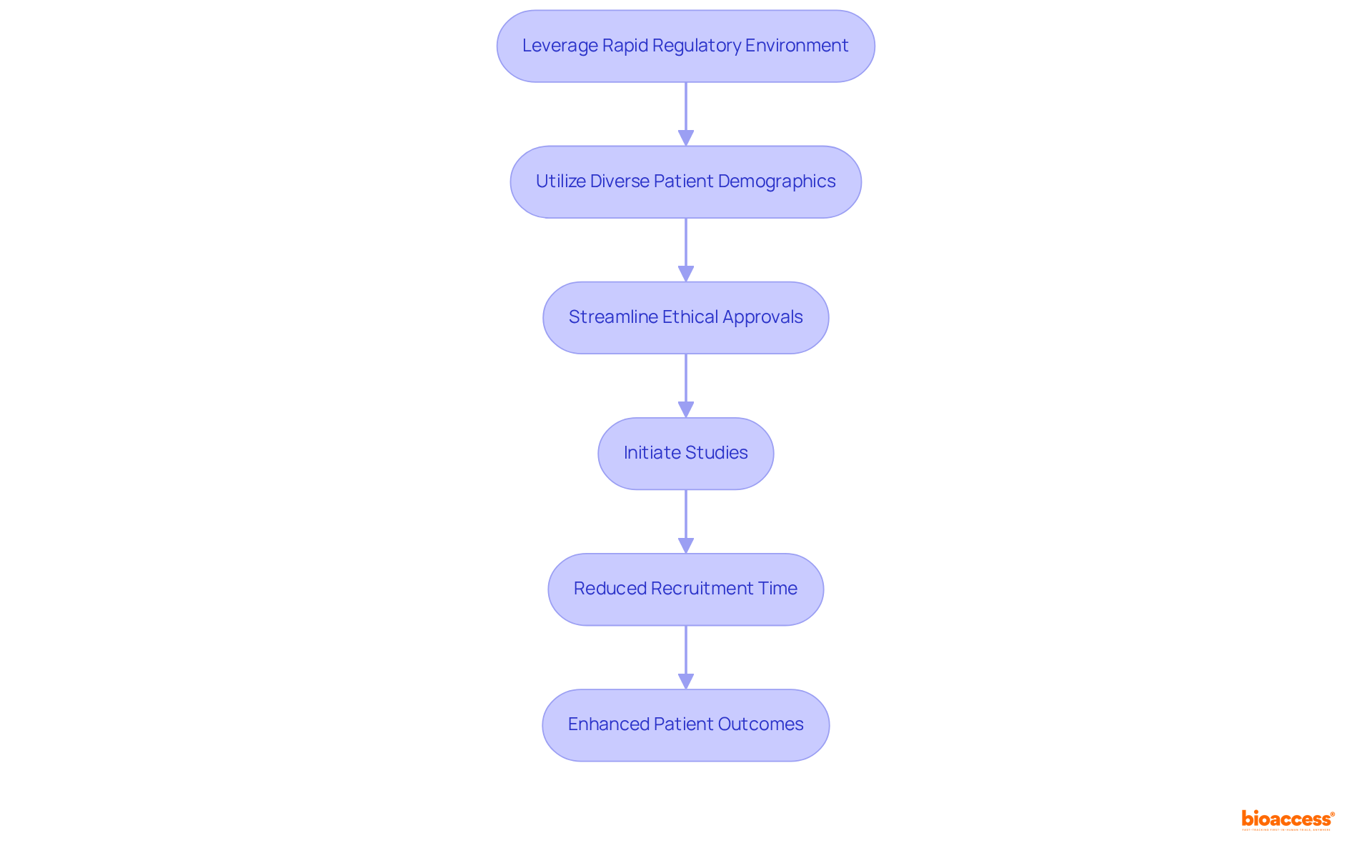
bioaccess® leverages the rapid regulatory environment of Latin America, the diverse patient demographics of the Balkans, and Australia's streamlined pathways to secure ethical approvals in an impressive 4-6 weeks. This pioneering research flexibility empowers Research Directors to initiate studies with remarkable speed, significantly shortening the time to market for innovative therapies.
Notably, a collaboration with Global Care Research Trials has demonstrated over a 50% reduction in recruitment time, underscoring the efficacy of this approach. As we look ahead to the evolving medical research landscape in 2025, the capacity to adeptly navigate these expedited processes not only enhances research capabilities but also fosters improved patient outcomes.
By integrating local expertise with efficient regulatory frameworks, bioaccess® establishes itself as a frontrunner in facilitating swift advancements in Medtech and Biopharma, ultimately benefitting the entire healthcare ecosystem.
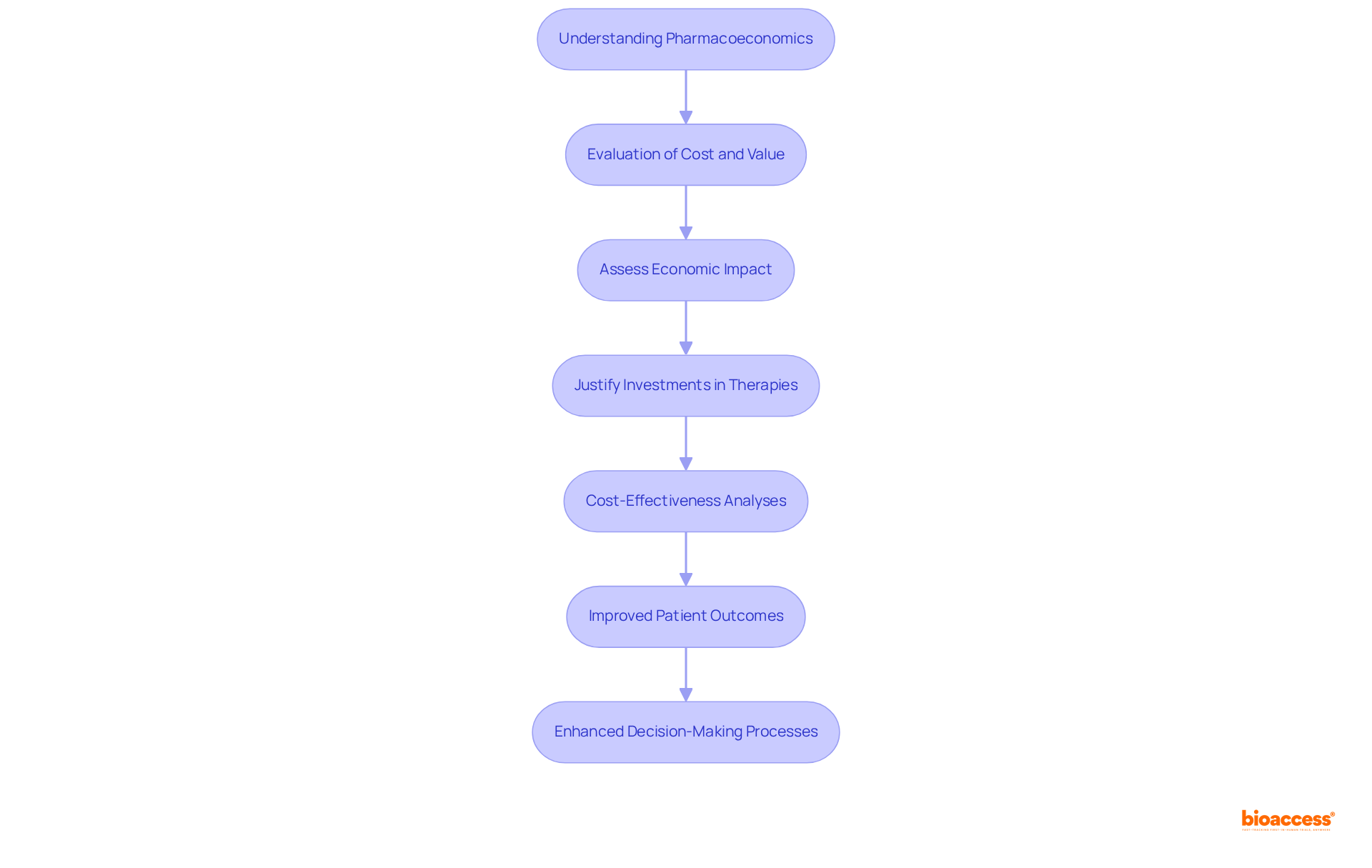
The role of pharmacoeconomics is critical in analyzing the cost and value of pharmaceuticals and medical interventions. Understanding pharmacoeconomics principles enables Trials Directors to assess the economic impact of their studies, ensuring optimal health outcomes while navigating budget constraints. This expertise is essential for justifying investments in new therapies and securing funding from stakeholders.
As we approach 2025, the importance of pharmacoeconomics in clinical trials is highlighted by its capacity to enhance decision-making processes. The rapid expansion of the biologics market, with a projected compound annual growth rate of 15% until 2027, makes pharmacoeconomics evaluations increasingly pertinent. For example, cost-effectiveness analyses in Medtech studies have shown that specific interventions can yield significant savings while simultaneously improving patient outcomes. These analyses not only provide a framework for evaluating new technologies but also assist in the effective prioritization of resources.
Clinical Research Directors recognize the transformative potential of pharmacoeconomics in influencing health outcomes. As one director noted, "Integrating pharmacoeconomics assessments into our trials enables us to make a persuasive argument for the acceptance of new treatments, guaranteeing that we achieve both therapeutic and economic objectives." This viewpoint emphasizes the dual commitment to patient care and fiscal responsibility, which is becoming increasingly crucial in today's healthcare environment.
The profound impact of pharmacoeconomics on health outcomes in medical trials is significant. By integrating these analyses into their research strategies, Clinical Research Directors can foster the development of cost-effective solutions that advance medical technology while enhancing the overall efficiency of healthcare delivery. Furthermore, with bioaccess® providing ethical approvals in just 4-6 weeks and achieving enrollment 50% faster than traditional markets, the integration of pharmacoeconomics evaluations can significantly improve research processes.
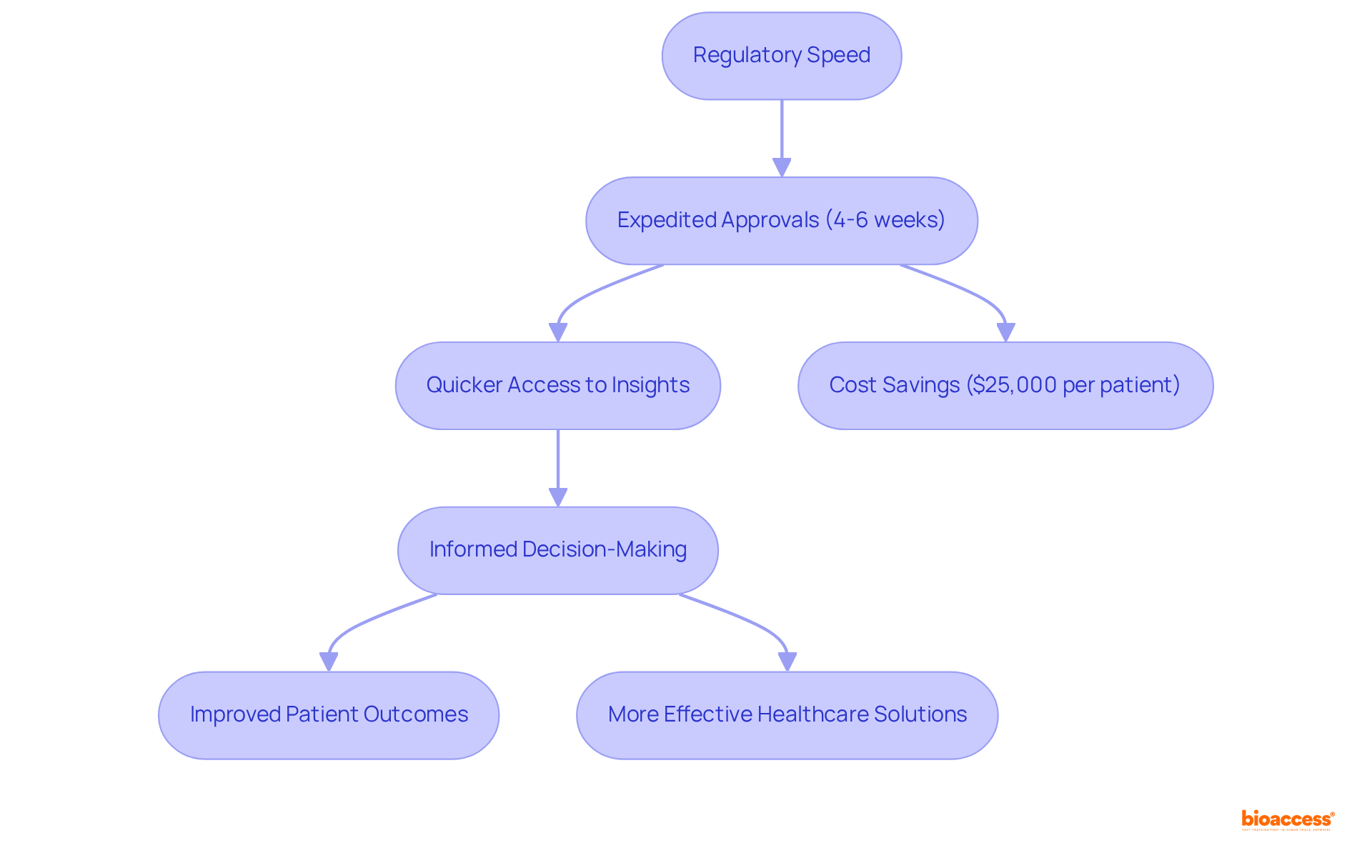
Regulatory speed is paramount in enhancing the efficiency of research trials, particularly in pharmacoeconomics, where timely data is essential for evaluating cost-effectiveness. By utilizing regions renowned for their expedited regulatory processes, such as Latin America, Clinical Research Directors can significantly expedite trial timelines.
For example, ethical approvals in Latin America are generally granted within 4 to 6 weeks, allowing for quicker access to vital insights that shape market access and reimbursement strategies. This rapid pace not only enhances the overall efficiency of medical trials but also supports informed decision-making, ultimately leading to improved patient outcomes and more effective healthcare solutions.
The capacity to conduct trials more swiftly translates into considerable cost savings, with estimates indicating reductions of $25,000 per patient when employing streamlined processes, particularly through expedited enrollment and FDA-ready data. As the Medtech sector evolves, the strategic advantage of regulatory speed in pharmacoeconomics becomes substantial, which is emphasized by John Babitt's statement that 'CROE support is essential for Medtech startups maneuvering through the intricacies of trials and market entry.'
Furthermore, with Latin America representing 10% of the world's study sites and the diverse patient demographics in the Balkans, the potential for enhanced trial efficiency and market access strategies is significant.
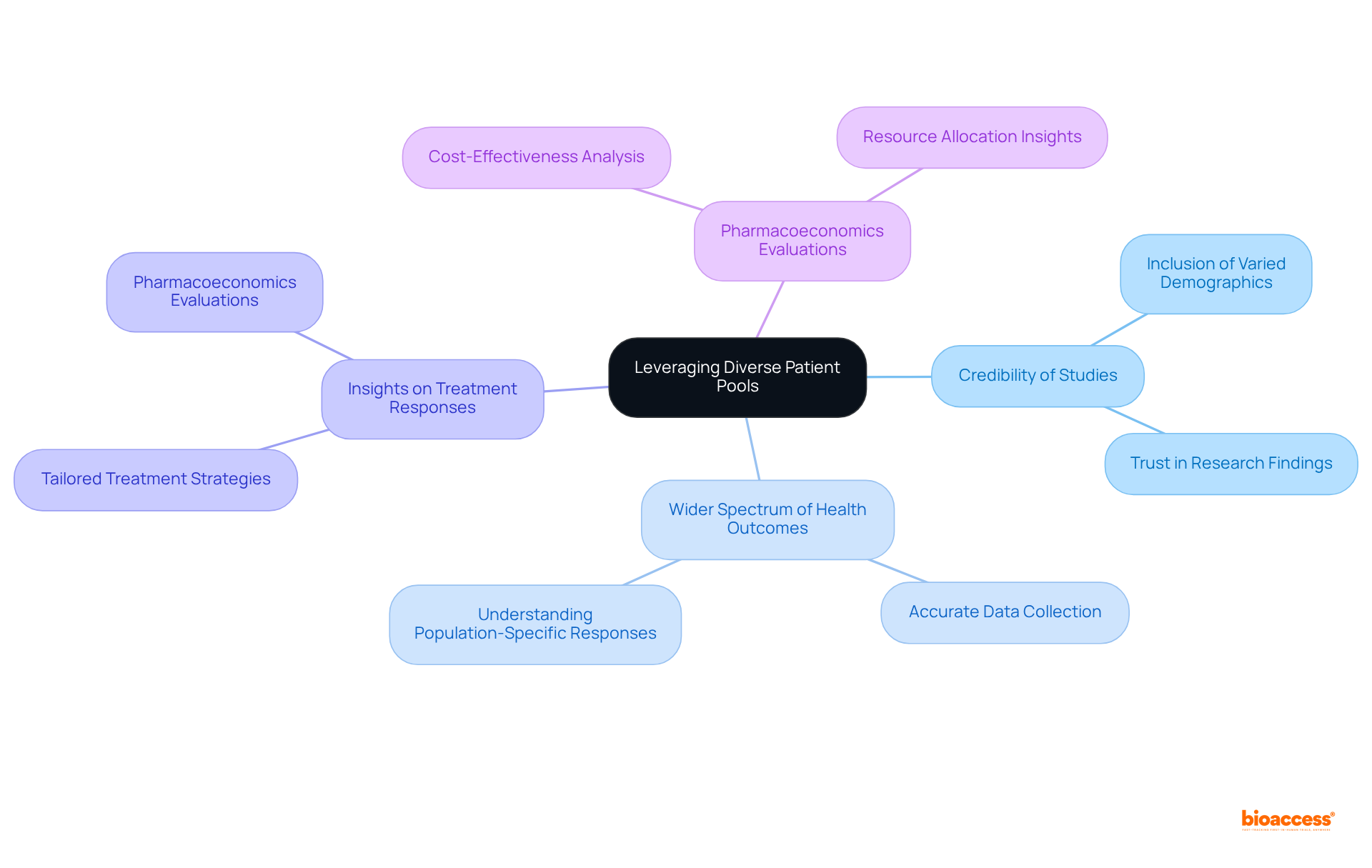
The inclusion of varied patient groups is essential for enhancing the credibility of clinical studies. Conducting research in regions characterized by diverse demographics, such as the Balkans, allows Clinical Research Directors to collect data that accurately reflects a wider spectrum of health outcomes. This diversity not only enriches the study itself but also facilitates a deeper understanding of how different populations respond to treatments. Such insights are critical for effective pharmacoeconomics evaluations, highlighting the necessity for comprehensive research strategies that incorporate diverse patient demographics.
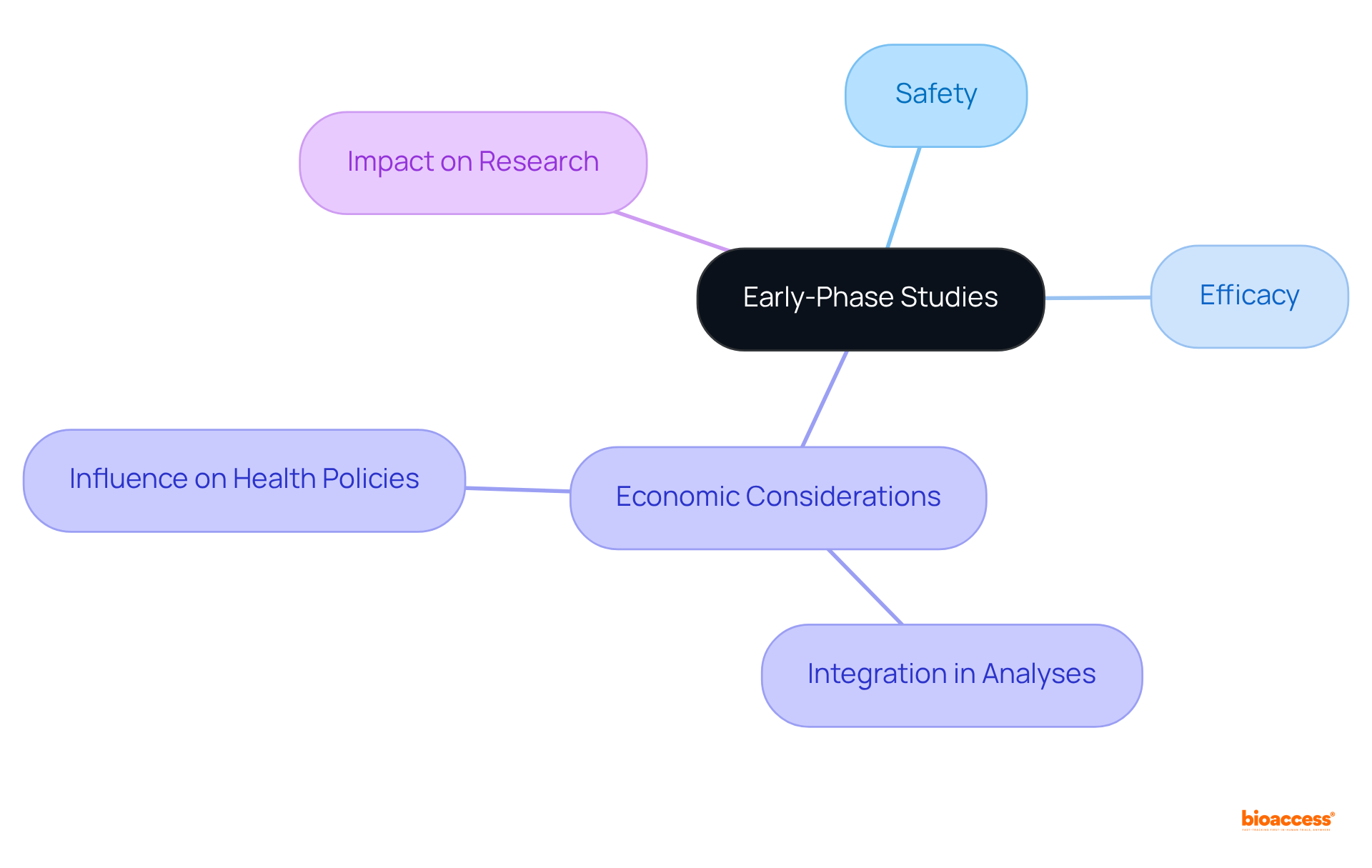
Early-phase studies, especially first-in-human (FIH) and early-feasibility studies (EFS), are essential in generating foundational data on safety and efficacy, which are critical for pharmacoeconomics evaluations. These studies provide initial insights into a treatment's potential value, which significantly influences pharmacoeconomics and decision-making processes.
For instance, the outcomes from FIH studies can guide the development of pharmacoeconomics analyses, ensuring that economic considerations are integrated from the outset of medical investigations. As highlighted by Hugo C Turner from the MRC Centre for Global Infectious Disease Analysis, 'Economic evidence is increasingly being used for informing health policies.' This underscores the imperative for Clinical Research Directors to prioritize these early-phase studies, thereby effectively informing subsequent research phases.
By adopting this approach, they can enhance the relevance of economic evaluations and ensure that resource allocation aligns with the demonstrated value of innovative treatments. Furthermore, with over 15 years of experience in the field, bioaccess® acknowledges the importance of incorporating economic factors from the beginning, a strategy that can significantly impact the success of medical studies.
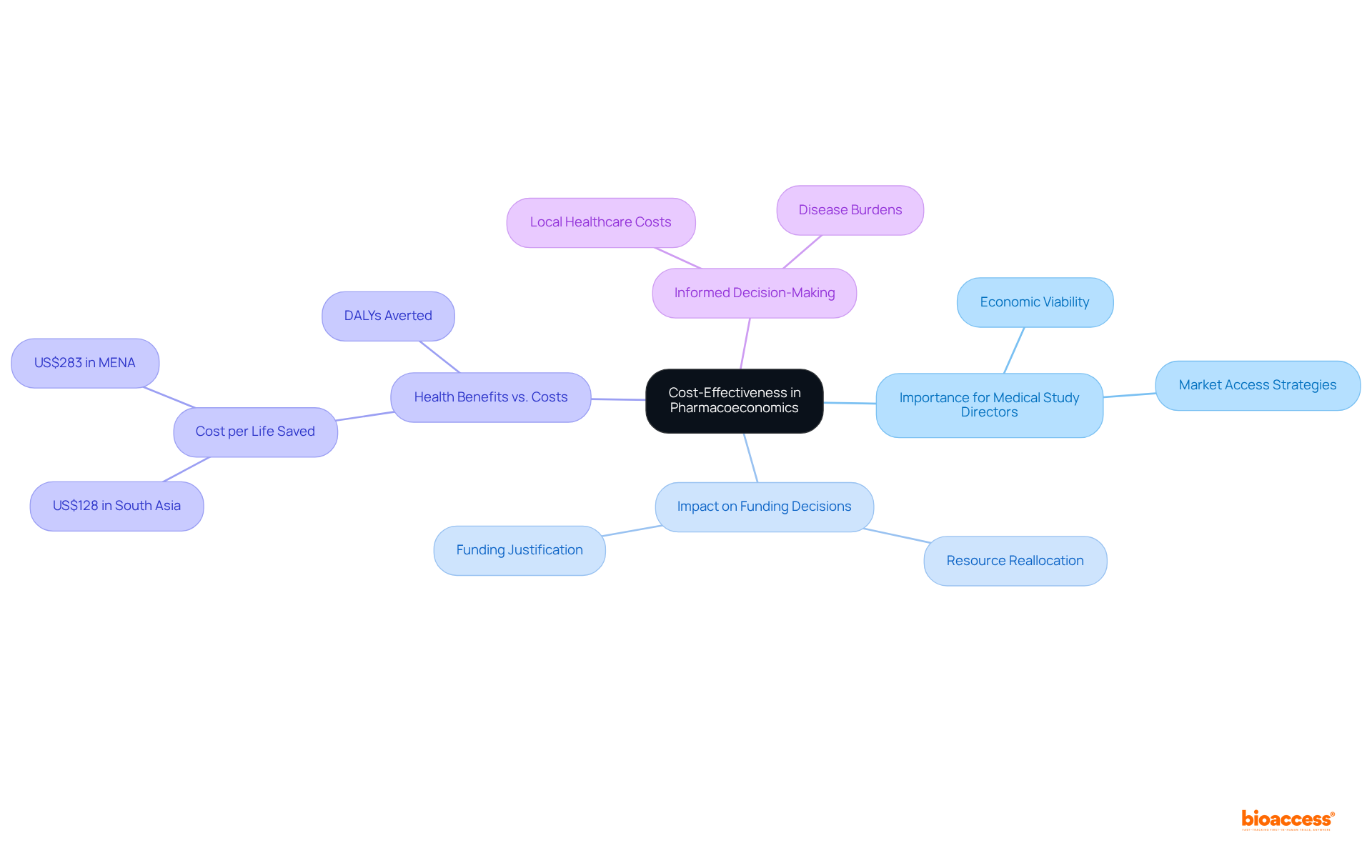
Cost-effectiveness stands as a cornerstone in pharmacoeconomics research, rigorously evaluating the relative costs and health outcomes of diverse interventions. For Medical Study Directors, incorporating pharmacoeconomics evaluations into clinical trials is essential for demonstrating the economic viability of new treatments. This analytical framework not only aids in securing funding but also strengthens market access strategies by delivering compelling evidence of a treatment's value.
Recent findings underscore that effective pharmacoeconomics analyses can profoundly impact funding decisions by illuminating interventions that provide significant health benefits at reduced costs. For example, reallocating resources toward more cost-effective interventions has been shown to double the number of life years saved across various healthcare settings.
Moreover, grasping the intricacies of these analyses—such as accounting for local healthcare costs and disease burdens—can foster informed decision-making and enhance patient outcomes. By prioritizing cost-effectiveness, Healthcare Investigation Directors can more effectively advocate for innovative therapies that address pressing health challenges through the lens of pharmacoeconomics.
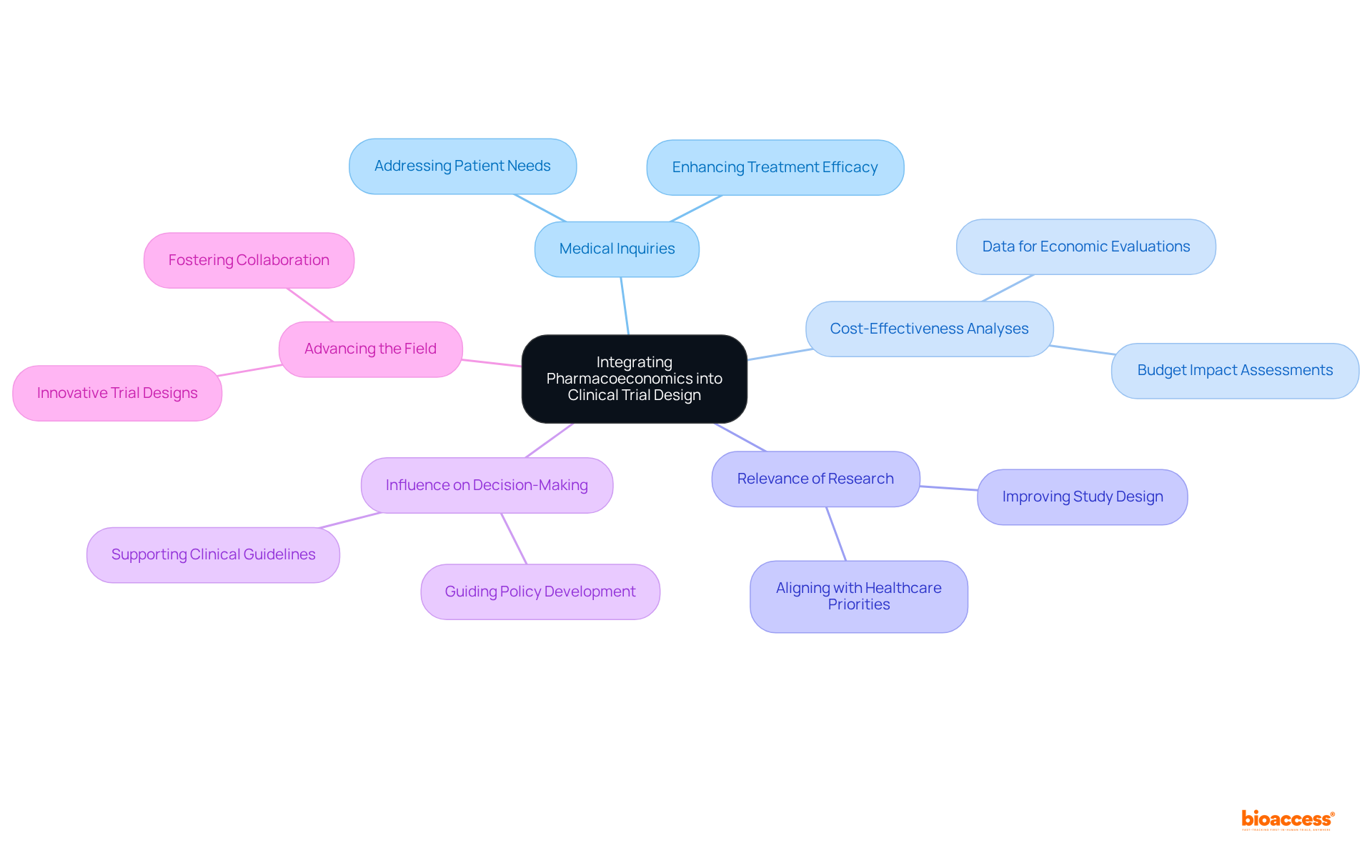
Incorporating pharmacoeconomics into trial design is essential for ensuring that studies effectively address both medical and pharmacoeconomic inquiries. By incorporating pharmacoeconomics during the planning phase, Trial Directors can develop studies that yield data essential for cost-effectiveness analyses. This strategic approach not only enhances the relevance of their research but also significantly influences healthcare decision-making. Ultimately, the inclusion of pharmacoeconomics in trial design is imperative for advancing the field and ensuring that clinical research meets the demands of both patients and healthcare systems.
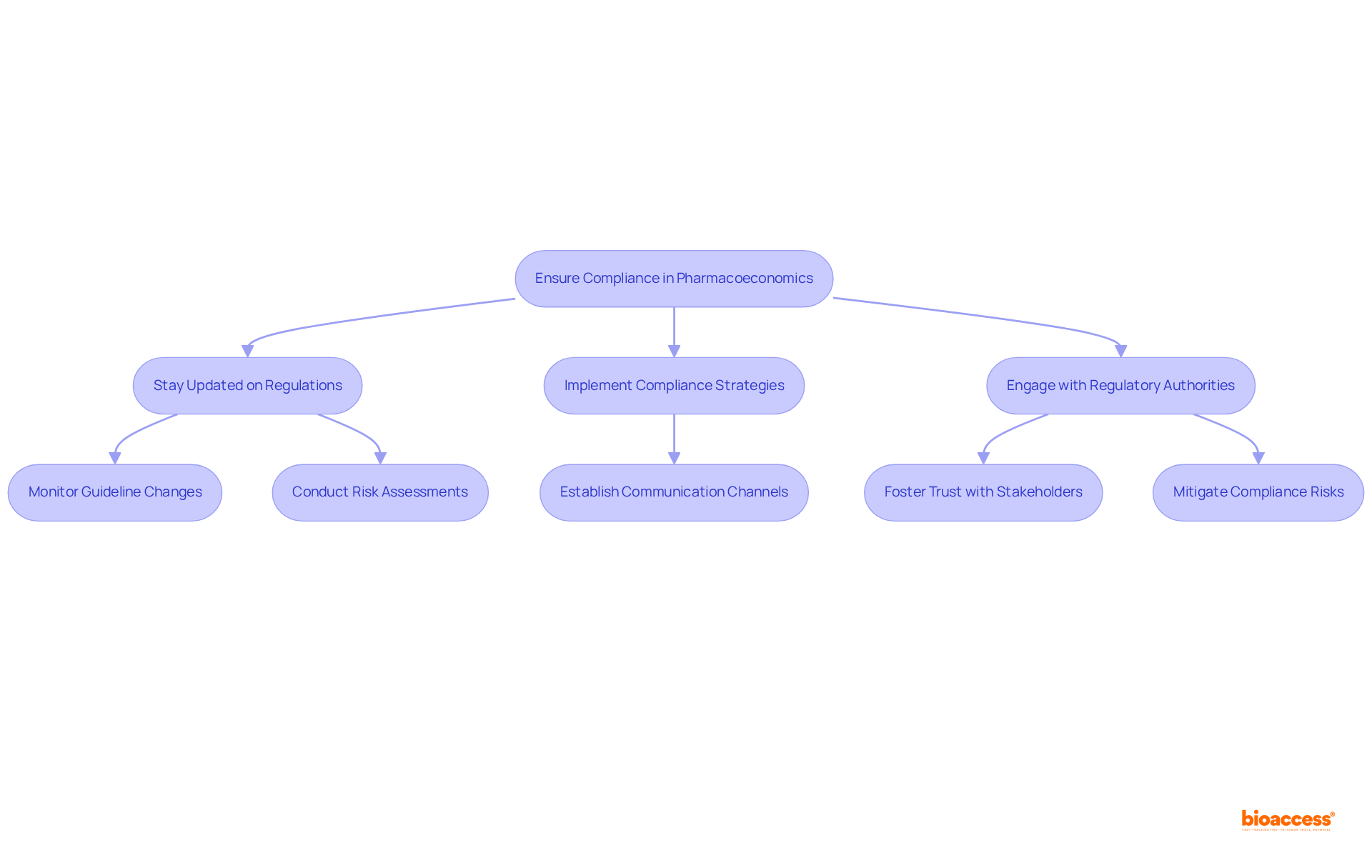
Adherence to regulations is paramount in pharmacoeconomics studies, directly influencing the integrity and credibility of trials. Trial Directors must remain vigilant regarding evolving guidelines, such as the recently approved E22 Guideline by the ICH Assembly in June 2023, to ensure their studies uphold the highest standards. Effective navigation of these regulations not only enhances the reliability of findings but also fosters trust with stakeholders, including regulatory bodies and funding agencies.
For instance, organizations that prioritize compliance can significantly mitigate risks associated with non-adherence, which contributes to approximately 125,000 deaths annually in the United States due to medication nonadherence and is linked to up to 25% of all hospitalizations each year. Furthermore, as the pharmaceutical industry braces for stricter regulations in 2025, encompassing enhanced pharmacovigilance and sustainability requirements, the capacity to adapt to these changes will be essential.
Successful instances of navigating regulations include collaborations that leverage foreign clinical data to streamline compliance processes, illustrating that proactive engagement with regulatory authorities can lead to more efficient study approvals. As one Medical Study Director observed, "Navigating the changing environment of regulations demands not only awareness but an active approach to guarantee adherence and protect our studies."
Ultimately, a robust compliance framework safeguards the integrity of pharmacoeconomics studies and positions organizations favorably in a competitive landscape.
Pharmacoeconomics data is pivotal in shaping market access strategies, providing a robust framework for demonstrating the cost-effectiveness of new therapies. This data not only enhances reimbursement applications but also empowers Medical Study Directors to negotiate favorable terms with payers. Successful reimbursement applications often depend on comprehensive pharmacoeconomic analyses that demonstrate both the clinical benefits of a therapy and its economic value compared to existing treatments. Such an approach facilitates market entry and reinforces the long-term viability of new products in increasingly competitive healthcare landscapes.
Engaging with payers using solid cost-effectiveness data can lead to more favorable negotiations, ultimately enhancing patient access to innovative therapies. As the healthcare environment evolves, particularly with significant legislative changes and payer decisions, leveraging pharmacoeconomics insights becomes crucial for securing reimbursement and ensuring the sustainability of new medical advancements.
To maximize the impact of pharmacoeconomics data, Directors of Trials should consider early engagement with HTA agencies to understand evaluation criteria and proactively address potential concerns.

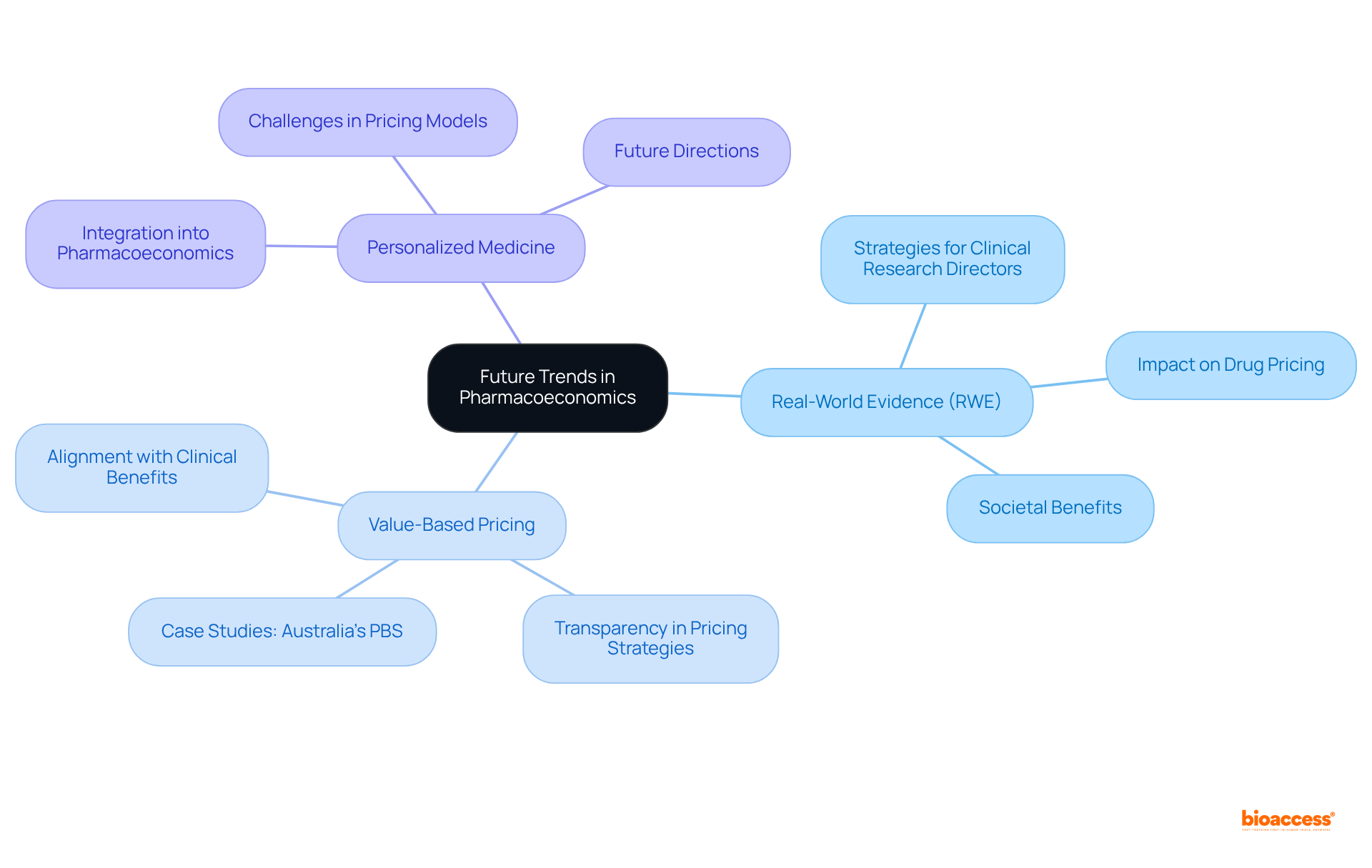
Future trends in pharmacoeconomics are increasingly influenced by the integration of real-world evidence (RWE) and value-based pricing, as well as the emergence of personalized medicine. Clinical Research Directors must proactively adjust their strategies to include RWE, which captures the complexities of patient experiences and treatment outcomes in everyday settings. This shift is crucial as real-world evidence (RWE) enhances the accuracy and generalizability of pharmacoeconomics models, allowing for more informed decision-making.
Value-based pricing is emerging as a pivotal approach, aligning drug prices with the clinical benefits they provide. This method not only addresses the rising costs of pharmaceuticals but also emphasizes the need for transparency in pricing strategies. Industry leaders have observed that the complexity of innovation and development costs complicates traditional pricing models, making value-based pricing a more viable alternative.
For instance, Australia's Pharmaceutical Benefits Scheme (PBS) has successfully implemented value-based pricing, approving over half of the 70 major drug submissions in 2020, demonstrating its effectiveness in reducing drug spending while ensuring patient access. Such examples emphasize the necessity for Trials Directors to adopt these evolving frameworks to sustain the relevance and impact of their studies.
Furthermore, the growing demand for RWE in pharmacoeconomics studies is underscored by a systematic review that identified economic factors as the most commonly referenced aspects in drug pricing conversations. This trend reflects a broader recognition of the importance of societal benefits and healthcare process improvements in determining drug value.
As the landscape of healthcare continues to evolve, Clinical Research Directors who prioritize the integration of RWE and value-based pricing into their research strategies will be better positioned to navigate the complexities of modern pharmacoeconomics, ultimately leading to more effective and patient-centered healthcare solutions.
The insights presented on pharmacoeconomics underscore its essential role in enhancing clinical research efficiency and informing decision-making for Clinical Research Directors. By grasping the economic implications of pharmaceuticals and medical interventions, professionals can adeptly navigate budget constraints while ensuring optimal health outcomes. The integration of pharmacoeconomics into clinical trial design not only supports the justification for new therapies but also aligns with the urgent demand for fiscal responsibility in healthcare.
Key arguments from the discussion highlight the significance of rapid regulatory processes, diverse patient demographics, and early-phase studies in shaping effective pharmacoeconomic evaluations. The capacity to conduct trials swiftly, especially in regions with expedited approval timelines, facilitates quicker access to crucial data that informs market access strategies. Moreover, leveraging diverse patient pools enriches research findings, ensuring that treatments are evaluated across a broad spectrum of demographics, which is vital for accurate pharmacoeconomic assessments.
As the healthcare landscape continues to evolve, it is imperative for Clinical Research Directors to adopt a proactive approach in integrating pharmacoeconomics into their strategies. This not only equips them to tackle future challenges but also enhances their ability to advocate for innovative therapies that deliver both clinical benefits and economic value. Emphasizing the importance of pharmacoeconomic data will ultimately lead to improved patient access to therapies and a more efficient healthcare system, ensuring that advancements in medical technology translate into tangible health outcomes for all.
What is bioaccess® and how does it benefit clinical research?
bioaccess® is a platform that leverages the rapid regulatory environment of Latin America, diverse patient demographics of the Balkans, and Australia's streamlined pathways to secure ethical approvals in 4-6 weeks. This flexibility allows Research Directors to initiate studies quickly, significantly reducing the time to market for innovative therapies.
How has bioaccess® demonstrated its effectiveness in clinical trials?
A collaboration with Global Care Research Trials has shown that bioaccess® can reduce recruitment time by over 50%, highlighting its efficacy in facilitating faster clinical research processes.
Why is pharmacoeconomics important in clinical trials?
Pharmacoeconomics is critical for analyzing the cost and value of pharmaceuticals and medical interventions. It helps Trials Directors assess the economic impact of their studies, ensuring optimal health outcomes while managing budget constraints and justifying investments in new therapies.
How is the biologics market influencing the role of pharmacoeconomics?
The biologics market is expected to grow at a compound annual growth rate of 15% until 2027, making pharmacoeconomics evaluations increasingly important for enhancing decision-making processes in clinical trials.
What are the benefits of integrating pharmacoeconomics into clinical research?
Integrating pharmacoeconomics allows Clinical Research Directors to make persuasive arguments for new treatments, ensuring both therapeutic and economic objectives are met. It also helps in the effective prioritization of resources and fosters the development of cost-effective solutions.
How does regulatory speed impact clinical trials in pharmacoeconomics?
Regulatory speed enhances the efficiency of research trials by allowing for quicker ethical approvals, typically within 4-6 weeks in regions like Latin America. This fast pace supports informed decision-making and leads to improved patient outcomes.
What are the financial implications of regulatory speed in clinical trials?
Utilizing expedited regulatory processes can lead to significant cost savings, with estimates suggesting reductions of $25,000 per patient, particularly through faster enrollment and obtaining FDA-ready data.
What is the significance of diverse patient demographics in clinical trials?
The diverse patient demographics in regions such as the Balkans enhance trial efficiency and market access strategies, contributing to more effective healthcare solutions and improved patient outcomes.