


Ensuring compliance with clinical trial data privacy is paramount in today's research landscape. Best practices in this area encompass a thorough understanding of regulatory frameworks, such as GDPR and HIPAA, alongside the implementation of robust data security measures. By enhancing transparency in clinical trial processes and training staff on privacy best practices, organizations can significantly bolster their compliance efforts.
Adhering to these regulations is not just about following the law; it’s about safeguarding participant information and maintaining trust in clinical research. Strong security protocols and effective communication are essential components that contribute to this trust. As the Medtech landscape evolves, the role of organizations like Bioaccess becomes increasingly vital in addressing these key challenges.
In conclusion, collaboration among stakeholders is crucial for navigating the complexities of clinical trial data privacy. By taking proactive steps and fostering a culture of compliance, organizations can ensure they are not only meeting regulatory requirements but also enhancing the integrity of their research efforts.
Navigating the complex landscape of clinical trial data privacy compliance presents a formidable challenge for research organizations, especially as regulations evolve and cyber threats intensify. Understanding frameworks like GDPR and HIPAA is crucial; however, mere awareness is insufficient. Organizations must actively implement robust security measures and cultivate transparency to safeguard sensitive information and uphold participant trust.
How can clinical research entities effectively balance compliance with the ever-changing demands of data privacy while ensuring the integrity of their studies? This article explores best practices that empower organizations not only to meet regulatory standards but also to enhance their overall data security and ethical research practices.
To ensure clinical trial data privacy and compliance with privacy regulations, clinical research entities must have a solid grasp of essential frameworks such as the General Data Protection Regulation (GDPR) and the Health Insurance Portability and Accountability Act (HIPAA). These regulations delineate the protocols for collecting, processing, and storing personal information, underscoring the necessity for organizations to ensure clinical trial data privacy by conducting regular audits to evaluate compliance and adapt to legislative changes. Notably, the ICH E6(R3) guidelines stress the significance of data integrity and traceability, which are crucial for maintaining participant trust and ensuring the validity of outcomes while upholding clinical trial data privacy.
At bioaccess, we offer comprehensive clinical trial management services that include:
Engaging legal experts, such as Katherine Ruiz, a specialist in regulatory affairs for medical devices and in vitro diagnostics in Colombia, can further assist organizations in effectively navigating the complexities of compliance. This collaboration reinforces a commitment to ethical research practices, ensuring that your clinical trials not only meet regulatory standards but also uphold the highest ethical benchmarks.

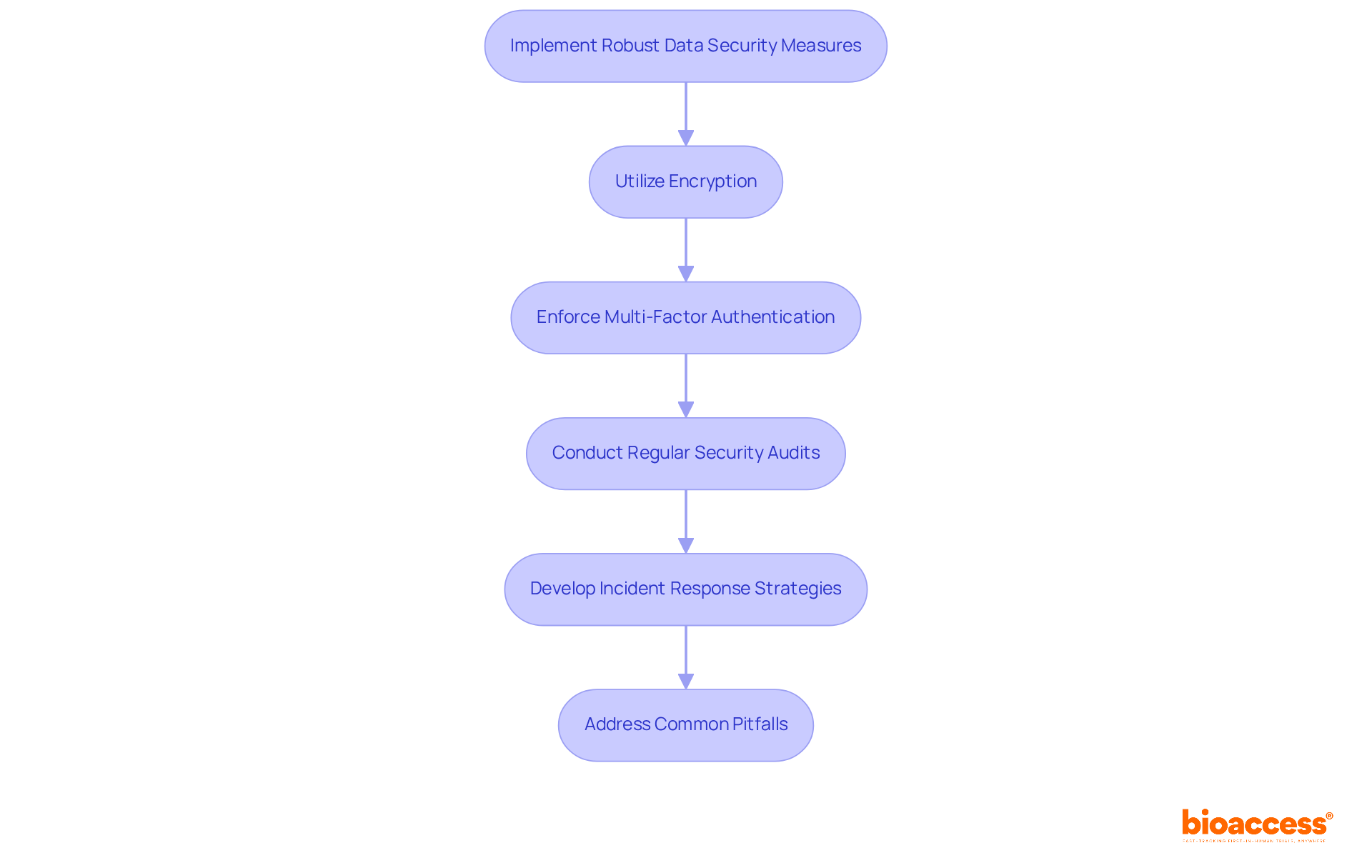
Implementing strong information security measures is crucial to protect clinical trial data privacy. Organizations must utilize encryption for information both at rest and in transit, ensuring that sensitive details remain protected from unauthorized access. Current trends reveal that hacking accounted for a staggering 79.7% of healthcare information breaches in 2023, underscoring the urgent need for robust security protocols.
To bolster security, multi-factor authentication (MFA) should be enforced across all systems managing personal information, adding an essential layer of protection. Regular security audits and vulnerability assessments are vital for identifying potential weaknesses within the system. For example, the PH Tech MOVEit breach illustrates how compromised information can lead to significant legal consequences, emphasizing the importance of maintaining information integrity and traceability.
Moreover, organizations should develop incident response strategies to swiftly and effectively address potential information breaches while ensuring clinical trial data privacy. The financial impact of a healthcare information breach is staggering, with costs reaching an average of $7.42 million in 2025. This reality highlights the necessity of implementing the security measures discussed.
Additionally, organizations must remain vigilant about common pitfalls in data security practices. Neglecting regular updates and failing to adequately train staff can lead to the misapplication of these critical principles. By addressing these challenges, organizations can enhance their security posture and protect sensitive information effectively.
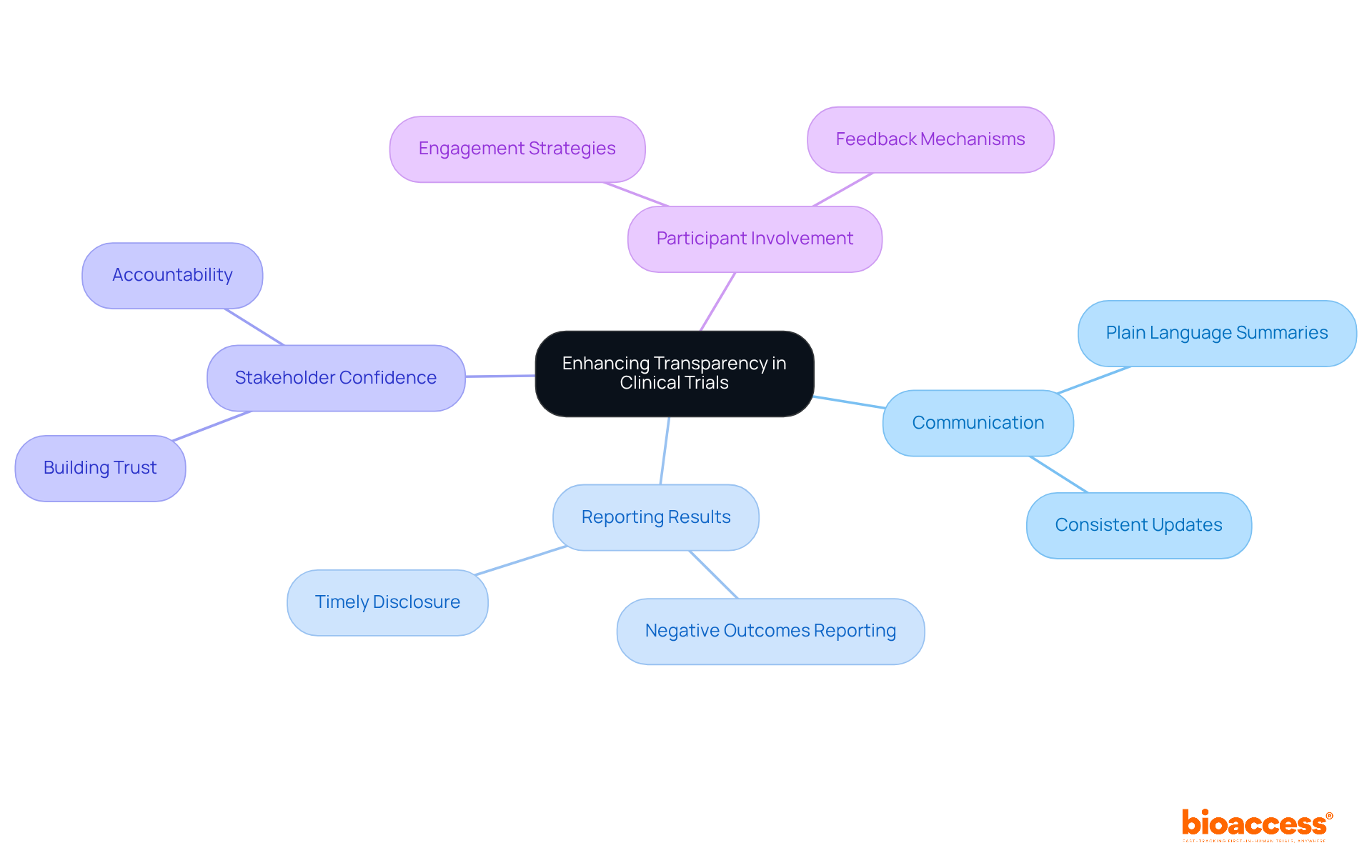
Improving openness in clinical research procedures is essential for building confidence among participants and stakeholders. Organizations must ensure that all study information—including objectives, methodologies, and potential risks—is communicated clearly. This can be accomplished through plain language summaries and consistent updates on trial progress. As of October 2025, 66,640 medical studies are registered, with a significant percentage available on platforms like ClinicalTrials.gov. This not only meets regulatory requirements but also enhances accountability.
Transparency in reporting results, including negative outcomes, is crucial for advancing medical knowledge and sustaining public trust in clinical research. By emphasizing participant communication, entities can establish a more knowledgeable and involved participant base. Ultimately, this approach results in more successful study outcomes.
Consider the implications of these practices: how can your organization enhance transparency and communication? The path forward is clear—prioritize openness to foster trust and improve the overall landscape of clinical research.
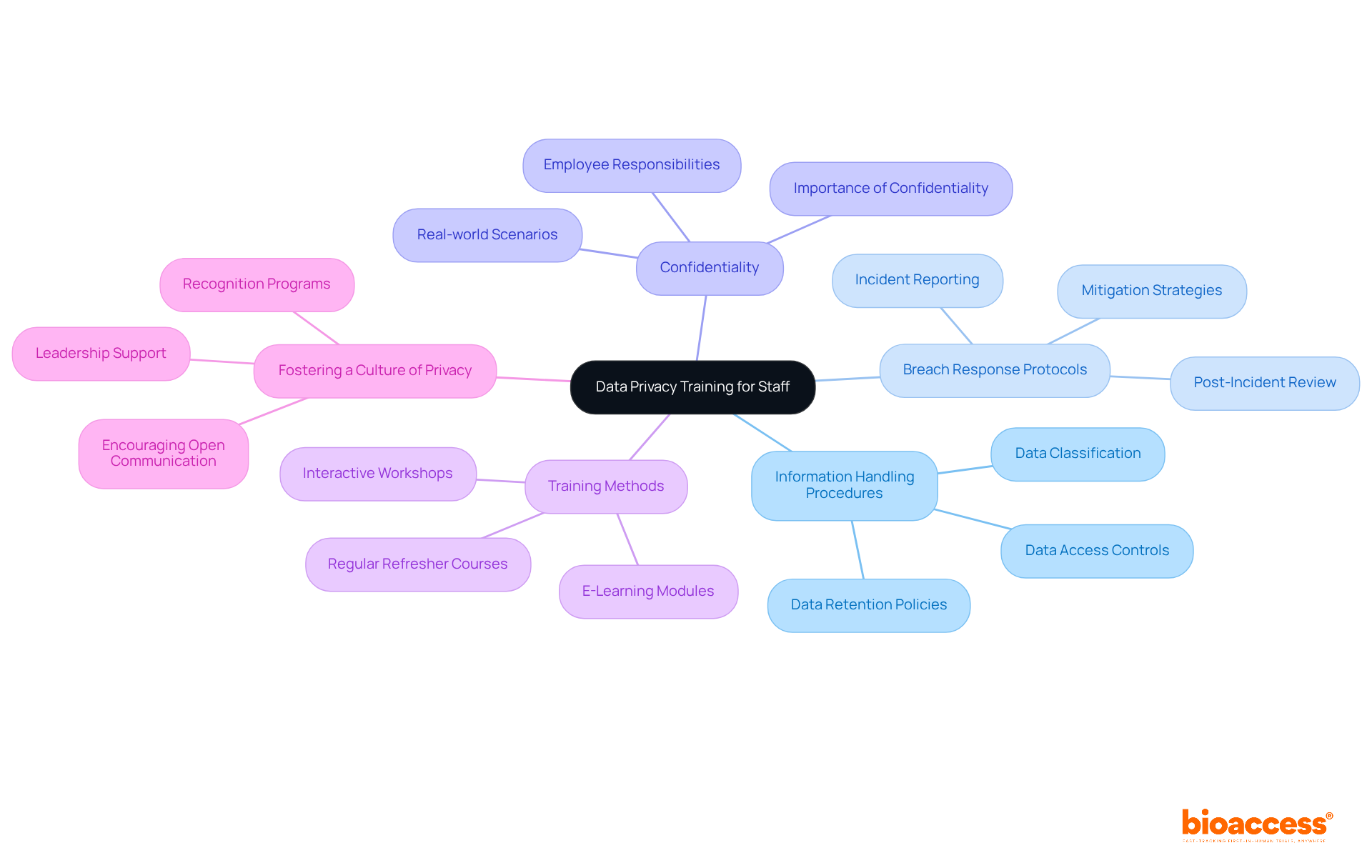
Educating personnel on privacy best practices is crucial for ensuring compliance and safeguarding sensitive participant information in the context of clinical trial data privacy. Notably, 31% of organizations believe they are investing more resources into regulatory adherence, which includes mandating privacy education for their research teams. This acknowledgment highlights the significance of maintaining confidentiality and following regulations to ensure clinical trial data privacy.
Training sessions should cover essential topics such as:
Regular refresher courses are essential to keep staff updated on evolving regulations and best practices, especially since 56% of compliance professionals dedicate their time to identifying and assessing risks.
For instance, incorporating real-world scenarios into training enhances understanding and retention of vital concepts, making the learning process more effective. Furthermore, fostering a culture of clinical trial data privacy within the organization encourages employees to prioritize participant confidentiality in their daily tasks, ultimately contributing to a more secure clinical trial environment.
Organizations like Secureframe exemplify effective training programs by offering comprehensive training on data privacy and security best practices, significantly reducing the risk of data breaches.
Ensuring compliance with clinical trial data privacy is not just a regulatory obligation; it’s a cornerstone of ethical research. Organizations involved in research must have a comprehensive understanding of regulatory frameworks like GDPR and HIPAA to safeguard personal information and maintain participant trust. By implementing robust data security measures, enhancing transparency in research processes, and providing thorough staff training, organizations can create a secure environment that prioritizes participant confidentiality and ethical practices.
Key insights emphasize the necessity of:
Organizations must recognize the evolving nature of data privacy regulations and invest in continuous education and training for their teams. This multifaceted approach not only protects sensitive information but also fosters a culture of accountability and trust within clinical trials.
Ultimately, the commitment to best practices in clinical trial data privacy compliance is critical. Organizations are encouraged to assess their current practices, invest in necessary improvements, and prioritize the protection of participant data. By doing so, they contribute to the advancement of medical knowledge while upholding the highest standards of integrity and trust in clinical research.
What are the key regulatory frameworks for data privacy in clinical trials?
The key regulatory frameworks for data privacy in clinical trials include the General Data Protection Regulation (GDPR) and the Health Insurance Portability and Accountability Act (HIPAA). These regulations outline the protocols for collecting, processing, and storing personal information.
Why is it important for clinical research entities to understand these regulations?
It is important for clinical research entities to understand these regulations to ensure compliance with privacy laws, maintain participant trust, and uphold the validity of trial outcomes while ensuring clinical trial data privacy.
How can organizations ensure compliance with data privacy regulations?
Organizations can ensure compliance by conducting regular audits to evaluate adherence to privacy regulations and by adapting to legislative changes as necessary.
What do the ICH E6(R3) guidelines emphasize regarding data integrity?
The ICH E6(R3) guidelines emphasize the significance of data integrity and traceability, which are crucial for maintaining participant trust and ensuring the validity of clinical trial outcomes.
What services does bioaccess provide for clinical trial management?
Bioaccess offers comprehensive clinical trial management services, including feasibility studies, compliance reviews, trial setup and start-up processes, import permits, continuous project management, and detailed reporting on study status and adverse events.
How can legal experts assist organizations in clinical trials?
Engaging legal experts, such as specialists in regulatory affairs, can assist organizations in navigating compliance complexities, reinforcing a commitment to ethical research practices, and ensuring that clinical trials meet regulatory standards and ethical benchmarks.