The article emphasizes the essential elements of crafting a successful plan for clinical research, highlighting the necessity of:
Each section delineates structured steps and best practices, such as:
These strategies collectively ensure that the research is well-organized and strategically positioned for success.
Crafting a successful plan for clinical research is a pivotal step that can dictate the trajectory of a study and its potential impact on healthcare. By clearly defining study objectives and hypotheses, researchers establish a solid foundation that enhances the reliability and relevance of their findings. However, navigating the complexities of target populations, study designs, and regulatory requirements presents significant challenges.
How can researchers ensure that their plans not only meet ethical standards but also optimize participant recruitment and resource allocation?
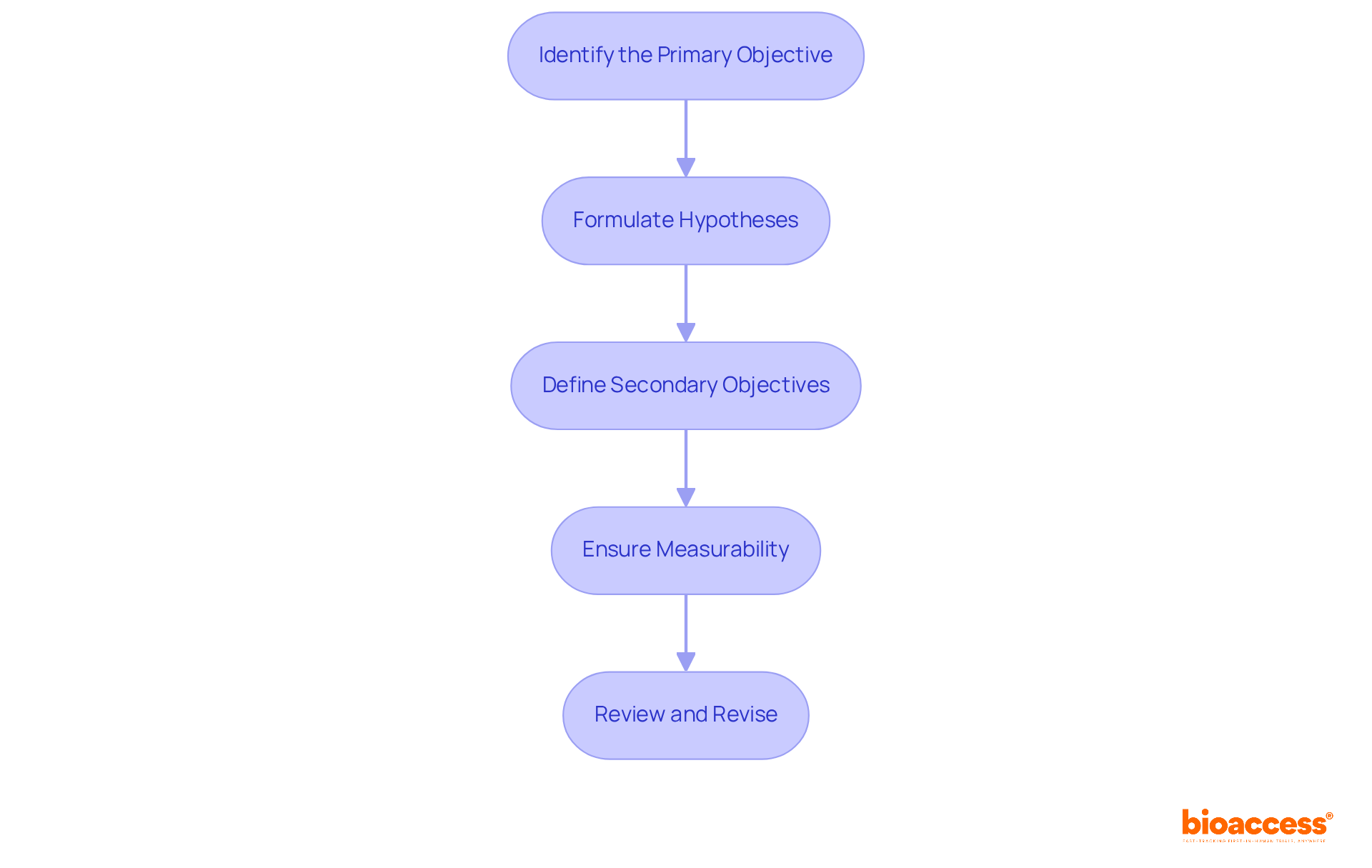
Identify the Primary Objective: Begin by pinpointing the main goal of your study. Clearly articulate the specific question that is outlined in the plan of the study you aim to answer. For instance, when evaluating a new drug, your primary objective may be to assess its efficacy against a placebo.
Formulate Hypotheses: Develop a testable hypothesis grounded in your main goal. In the plan of the study, a well-structured hypothesis should be both clear and specific, such as 'Drug A will significantly reduce symptoms of Condition X compared to a placebo.' Research indicates that approximately 70% of clinical studies succeed when their goals are clearly outlined, underscoring the importance of this step.
Define Secondary Objectives: Consider additional inquiries that may arise during your research. The plan of the study could involve investigating side effects or the drug's impact on quality of life, thereby providing a broader context for your findings.
Ensure Measurability: Confirm that your goals and hypotheses are measurable through quantitative or qualitative methods. This clarity will enhance the plan of the study by streamlining data collection and analysis, thereby improving the reliability of your results.
Review and Revise: After drafting your objectives and hypotheses, critically evaluate them for clarity and feasibility. Engaging colleagues or mentors for feedback can refine your focus in the plan of the study, ensuring that your research is positioned for success. As noted by experts, the iterative process of hypothesis formulation is vital for advancing clinical research effectively.
Define the Target Population: Identifying the specific group of individuals for your research is crucial. Consider factors such as age, gender, health status, and geographical location. For instance, if your research focuses on a new diabetes medication, your target population could be adults aged 30-65 with Type 2 diabetes. Clear definitions are essential in the plan of the study, as they ensure that research with well-defined populations produces more dependable results and enhances the relevance of findings to real-world situations.
Choose the Research Design: Selecting a research design that aligns with your research objectives is vital. Common designs include randomized controlled experiments (RCTs), cohort studies, and case-control studies. If your goal is to compare the effectiveness of two treatments, an RCT would be the most suitable choice. In 2025, innovative designs such as adaptive studies are gaining traction, allowing for modifications based on interim results, thus enhancing efficiency and patient involvement.
Consider Sample Size: Calculating the necessary sample size to achieve statistically significant results is imperative. This calculation should factor in the expected effect size, population variability, and the desired statistical power. Current guidelines suggest that larger sample sizes lead to more reliable conclusions, but they also require careful resource management to avoid exposing more patients to potential risks.
Recruitment Strategies: Developing a comprehensive plan for participant recruitment is essential. This may involve outreach through clinics, advertisements, or collaborations with healthcare providers. Ethical and inclusive recruitment methods are crucial, as around 80% of clinical studies encounter delays or closures due to recruitment issues. Involving patients via their healthcare professionals can greatly enhance recruitment rates, as research indicates that 73% of patients favor receiving information about clinical trials from their physicians.
Pilot Testing: Prior to large-scale execution, consider conducting a pilot examination to evaluate your recruitment strategies and research procedures. This preliminary phase can help identify potential issues and refine your approach, ensuring a smoother transition to the plan of the study. Pilot testing is especially beneficial in intricate studies, where logistical challenges can influence participant engagement and data quality.

Identify Relevant Regulations: Begin by familiarizing yourself with the regulations governing clinical research in your region, including guidelines from the FDA, EMA, and local ethics committees. Understanding these regulations is crucial for ensuring compliance and safeguarding participant rights. At bioaccess®, we specialize in navigating these regulatory landscapes, providing tailored solutions that expedite the clinical trial process for Medtech startups in Latin America.
Prepare Required Documentation: Gather all essential documents for submission, such as the research protocol, informed consent forms (ICFs), and investigator brochures. These documents must be clear, comprehensive, and aligned with ethical standards. Notably, the FDA mandates that ICFs be reviewed and approved by an ethics committee before submission. Our expertise ensures that all documentation meets local requirements, facilitating a smoother approval process.
Submit for Ethical Review: Submit your research for evaluation by an Institutional Review Board (IRB) or Ethics Committee (EC). This process assesses the ethical dimensions of your research, ensuring participant safety and informed consent. Statistics suggest that the average duration for ethics consent can take up to 48 days, significantly affecting the overall trial start-up timeline.
Address Feedback: Be prepared to address any feedback or concerns raised by the IRB/EC. This may involve revising your protocol or consent forms to meet ethical standards. Collaborating with the review board positively can simplify the endorsement process and improve the quality of your research. Successful ethical endorsement processes often hinge on thorough documentation and proactive communication.
Secure Final Consent: Once all concerns are addressed, secure final consent before commencing the study. Keep a thorough log of all communications and consents for future reference. Incorporating insights from industry leaders can further enhance the authority of your approach. Furthermore, take note of the FDA's guidance released in May 2023 to support decentralized trials, which is pertinent to current ethical review practices. Lastly, consider the statistic that 11% of sites fail to enroll a single patient, highlighting the challenges faced in recruitment and the importance of addressing ethical considerations effectively.

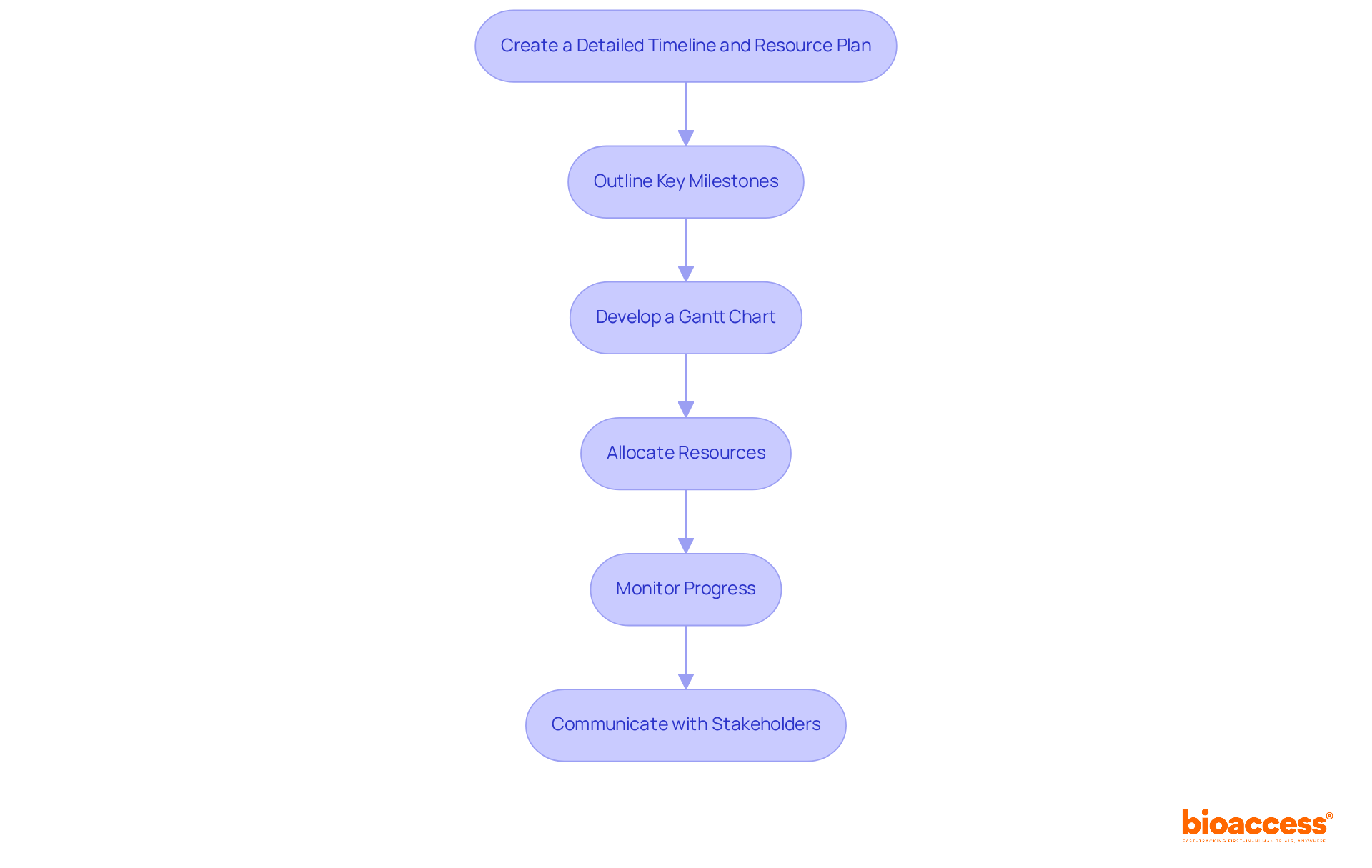
Outline Key Milestones: Identify the major milestones in your research, such as protocol approval, participant recruitment, data collection, and analysis. This structured approach, which is part of the plan of the study, helps visualize the overall timeline and ensures that critical phases are not overlooked.
Develop a Gantt Chart: Create a Gantt chart to visually map out the timeline. This chart should encompass all tasks, their durations, and dependencies, facilitating easy tracking of progress and adjustments as needed. The use of Gantt charts in project management is crucial, as they provide a clear overview of the project’s status and help in anticipating potential delays.
Allocate Resources: Evaluate the resources necessary for each stage of the research, including personnel, equipment, and budget. Efficient resource distribution is crucial; research shows that almost 50% of clinical experiments encounter delays due to insufficient resource planning. Ensuring that necessary resources are available when needed can significantly enhance the efficiency of the trial.
Monitor Progress: Regularly review the timeline and resource allocation to keep the research on track. This proactive monitoring allows for timely adjustments to the plan of the study, accommodating unforeseen challenges and minimizing disruptions.
Communicate with Stakeholders: Maintain open lines of communication with all stakeholders regarding the timeline and any changes. Regular updates foster transparency and ensure alignment with the study's goals, which is essential for successful collaboration. As Peter Drucker noted, understanding the customer—here, the stakeholders—is key to ensuring that the project meets its objectives.
Crafting a successful plan for clinical research is essential for ensuring that studies are not only effective but also ethical and compliant with regulations. By focusing on clearly defined objectives, measurable hypotheses, and a well-structured study design, researchers can pave the way for impactful findings that contribute to medical advancements. This comprehensive approach is vital in enhancing the reliability and relevance of research outcomes.
Key components discussed include:
Each step, from defining objectives to securing ethical approvals, plays a critical role in the overall success of the clinical research process. Moreover, the emphasis on resource planning and timeline management highlights the necessity of careful preparation and ongoing communication among stakeholders to avoid common pitfalls that can delay or derail studies.
Ultimately, the significance of a meticulously crafted study plan cannot be overstated. It not only streamlines the research process but also safeguards the rights and well-being of participants. By adhering to best practices and being proactive in addressing challenges, researchers can enhance the integrity and impact of their work, ultimately advancing the field of clinical research. Engaging with these principles is not just beneficial; it is essential for anyone dedicated to making meaningful contributions to healthcare through research.
What is the primary objective in a study?
The primary objective is the main goal of the study, which involves clearly articulating the specific question that the study aims to answer, such as assessing the efficacy of a new drug against a placebo.
How should hypotheses be formulated in a study?
Hypotheses should be developed as testable statements grounded in the main goal of the study. They need to be clear and specific, for example, stating that 'Drug A will significantly reduce symptoms of Condition X compared to a placebo.'
What are secondary objectives in a study?
Secondary objectives are additional inquiries that may arise during research, such as investigating side effects or the impact of a drug on quality of life, which provide broader context for the findings.
Why is measurability important in study objectives and hypotheses?
Measurability is important because it ensures that the goals and hypotheses can be assessed through quantitative or qualitative methods, enhancing data collection and analysis, and improving the reliability of the results.
What should be done after drafting study objectives and hypotheses?
After drafting, it is essential to critically evaluate them for clarity and feasibility. Engaging colleagues or mentors for feedback can help refine the focus of the study, positioning the research for success.
How does the clarity of study goals impact clinical studies?
Research indicates that approximately 70% of clinical studies succeed when their goals are clearly outlined, highlighting the significance of clearly defined objectives and hypotheses in the study plan.