


The article defines accuracy and precision in clinical research as critical concepts that ensure the reliability of measurements.
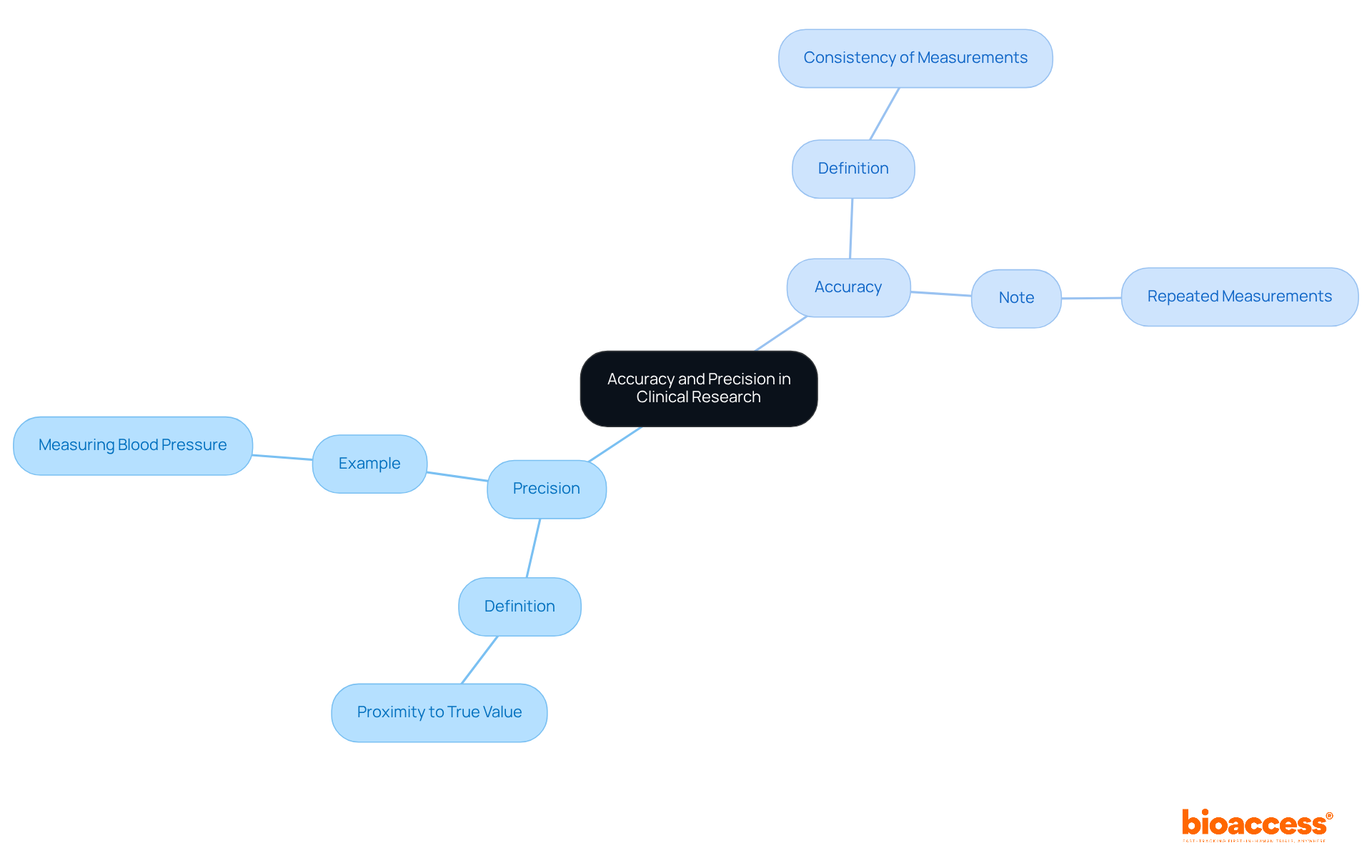
Accuracy pertains to the closeness of a measurement to the true value, while precision indicates the consistency of repeated measurements.
Understanding these definitions is essential for designing studies and interpreting results correctly.
Real-world examples and strategies for improving measurement reliability reinforce their importance, collectively underscoring the necessity of accuracy and precision in achieving valid research conclusions.
In the intricate world of clinical research, accuracy and precision are foundational pillars that shape the integrity of study outcomes. Understanding these terms transcends mere academic exercise; it is essential for ensuring that research findings accurately reflect the true state of health conditions and treatment effects.
However, navigating the complexities of measurement and data collection presents a significant challenge, where even minor deviations can result in substantial misinterpretations.
How can researchers effectively define and enhance accuracy and precision to safeguard the validity of their studies and ultimately improve patient care?
In the realm of medical research, it is essential to define accuracy and precision, with precision being a critical concept that refers to the proximity of a measured value to the actual or accepted value. For instance, when a medical trial measures blood pressure, precision indicates how closely the recorded blood pressure aligns with the patient's true blood pressure. Conversely, accuracy pertains to the consistency of repeated measurements. If multiple blood pressure readings yield similar results, these measurements are deemed precise, irrespective of their accuracy. Grasping these definitions is essential to define accuracy and precision for effectively designing studies and interpreting results, as they lay the foundation for reliable clinical research.
In clinical research, it is important to define accuracy and precision, as they are paramount for several reasons. They ensure that the information gathered is used to define accuracy and precision in reflecting the true condition of the subjects being examined, which is essential for drawing valid conclusions.
For instance, in ReGelTec's Early Feasibility Study on HYDRAFIL™ for addressing chronic low back pain in Colombia, upholding high standards of correctness and exactness was crucial for the effective treatment of eleven patients with degenerative disc disease.
To avoid potentially harming patients, it is crucial to define accuracy and precision, as inaccurate or imprecise data can lead to incorrect assumptions about treatment efficacy. Furthermore, regulatory authorities define accuracy and precision as essential requirements to authorize medical trials and their results.
Partnerships, such as the collaboration between GlobalCare Clinical Trials and bioaccess™, which aim to enhance trial ambulatory services in Colombia, have demonstrated success by achieving over a 50% decrease in recruitment time and 95% retention rates.
Thus, maintaining these standards is not merely a matter of scientific integrity; it is also a legal and ethical obligation to define accuracy and precision.

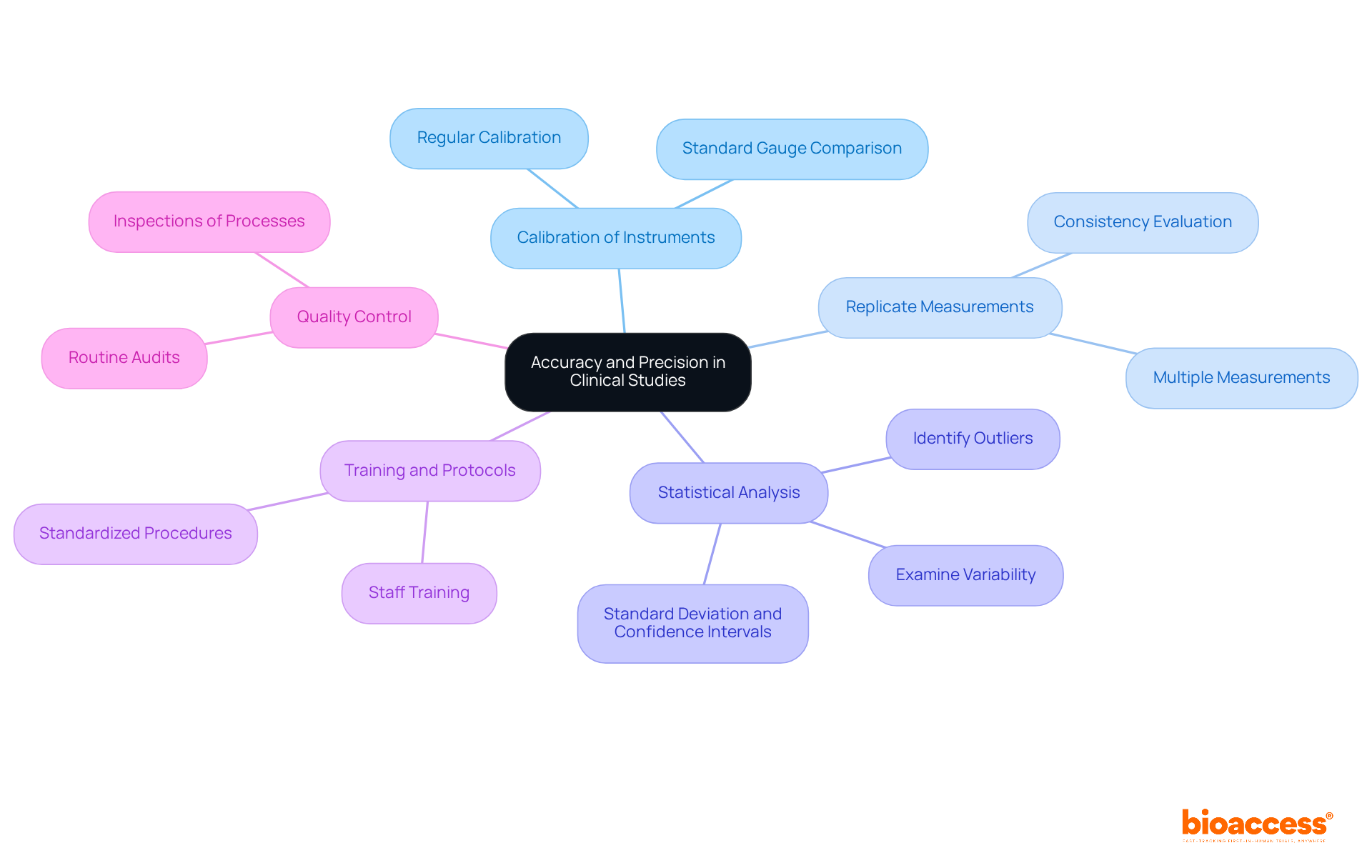
To accurately define accuracy and precision in clinical studies, researchers must employ several essential strategies.
Calibration of Instruments: Regular calibration of measurement tools is crucial to ensure accurate readings. For instance, blood pressure monitors should be calibrated against a standard gauge to maintain reliability.
Replicate Measurements: Conducting multiple measurements of the same variable is vital to evaluate accuracy. Consistent results indicate that the measurements are precise, reinforcing the study's credibility.
Statistical Analysis: Utilizing statistical techniques to examine variability and identify outliers is a necessary practice. Techniques such as standard deviation and confidence intervals help define accuracy and precision, providing a robust analytical framework.
Training and Protocols: It is imperative that all staff involved in data collection are well-trained and adhere to standardized procedures. This minimizes variability in measurements, ensuring the integrity of the data collected.
Quality Control: Implementing quality control measures throughout the study is essential for continuously monitoring data integrity. This can encompass routine audits and inspections of information-gathering processes, solidifying the study's reliability.
Several tools and resources are essential for enhancing the ability to define accuracy and precision in clinical research, particularly when utilizing the comprehensive clinical trial management services offered by bioaccess®.
Clinical Information Management Systems (CIMS) play a pivotal role in facilitating information collection and ensuring consistency across various locations, significantly minimizing errors. bioaccess® employs advanced Clinical Data Management Systems (CDMS) to enhance information integrity throughout all phases of clinical trials.
Electronic Information Collection (EIC) systems allow for instant information entry and oversight, thereby improving information precision. With bioaccess®'s expertise in First-In-Human and Pivotal Studies, Electronic Data Capture (EDC) systems are optimized for swift and accurate information collection.
Statistical Software, such as SPSS or R, conducts complex analyses to evaluate information accuracy and precision, providing valuable insights into variability and reliability. bioaccess® leverages these tools to ensure robust statistical analysis in all medical studies, backed by over 20 years of experience in the Medtech sector.
Training Programs are crucial investments for staff, focusing on best practices for information collection and management to minimize human error. bioaccess® offers tailored training programs designed to help clinical research teams uphold high standards of accuracy.
Quality Assurance Tools are instrumental in implementing regular audits and checks of data integrity, ensuring that discrepancies are promptly identified and addressed. bioaccess® emphasizes quality assurance throughout the trial process, particularly in Post-Market Clinical Follow-Up Studies (PMCF), to maintain regulatory excellence.

Understanding the concepts of accuracy and precision is fundamental in clinical research, serving as the bedrock for reliable and valid study outcomes. Accurately defining these terms not only enhances the integrity of research but also ensures that the data collected truly reflects the conditions of the subjects involved. This clarity is crucial for making informed decisions about treatment efficacy and patient safety.
Throughout this article, we have highlighted key strategies for improving accuracy and precision in clinical studies. These strategies include:
Furthermore, utilizing advanced tools such as Clinical Information Management Systems and Electronic Data Capture systems can significantly enhance data integrity. The collaboration between organizations like GlobalCare Clinical Trials and bioaccess™ exemplifies the benefits of maintaining high standards in clinical research.
Ultimately, the significance of accuracy and precision extends beyond scientific rigor; it embodies a commitment to ethical research practices and patient welfare. As the landscape of clinical trials continues to evolve, prioritizing these principles will lead not only to more reliable results but also to fostering trust in the medical research community. Researchers are encouraged to adopt best practices and leverage available resources to uphold these essential standards, ensuring that their findings contribute positively to medical advancements and patient care.
What is precision in clinical research?
Precision in clinical research refers to the proximity of a measured value to the actual or accepted value. It indicates how closely a recorded measurement aligns with the true value.
What does accuracy mean in the context of clinical research?
Accuracy pertains to the consistency of repeated measurements. If multiple measurements yield similar results, they are considered precise, regardless of whether they are accurate.
Why are accuracy and precision important in clinical research?
Understanding accuracy and precision is essential for effectively designing studies and interpreting results, as they form the foundation for reliable clinical research.