


The article defines medical devices as essential tools intended for the diagnosis, prevention, or treatment of diseases. Understanding their intended use and regulatory classifications is crucial. This definition is supported by outlining key concepts such as:
These organizations ensure that medical devices meet stringent safety and effectiveness standards throughout their lifecycle, underscoring the importance of compliance in the Medtech landscape.
Understanding medical devices is crucial for anyone involved in healthcare research and development. These instruments, ranging from simple bandages to complex MRI machines, play a pivotal role in diagnosing, treating, and monitoring health conditions. This article provides a comprehensive step-by-step guide that empowers researchers to navigate the intricate landscape of medical device definitions, classifications, and regulatory compliance.
However, with evolving regulations and the impending changes set for 2025, how can researchers ensure their products meet the necessary standards while also addressing market needs?
Healthcare instruments encompass a diverse array of items utilized for clinical purposes. The FDA defines medical devices as any tool, apparatus, implement, machine, contrivance, implant, in vitro reagent, or similar article intended for use in the diagnosis, prevention, or treatment of disease. Understanding the following key concepts is essential:
In Colombia, the regulatory environment is overseen by the National Institute for the Surveillance of Medicines and Foods, which plays a vital role in ensuring the safety, effectiveness, and quality of healthcare products. As a Level 4 health authority recognized by the Pan American Health Organization/World Health Organization, the agency is responsible for inspecting and supervising the marketing and manufacturing of health products, including therapeutic instruments. This oversight involves ensuring adherence to technical standards and best practices, which is essential for researchers to consider when developing new equipment. The Directorate for Health Instruments and other Technologies within INVIMA specifically emphasizes these aspects, ensuring that health instruments meet established standards.
Recent updates indicate that by 2025, the FDA will enforce new rules impacting medical equipment classifications, underscoring the significance of intended use in establishing oversight pathways. For instance, the FDA's statistics reveal that products categorized differently may have distinct requirements for clinical evidence depending on their intended application. This highlights the importance for researchers to articulate the aim of their equipment clearly, ensuring compliance with evolving oversight criteria and facilitating smoother navigation through the approval process. By comprehending these essential concepts and recognizing the role of the agency, particularly the Directorate for Medical Equipment, researchers can effectively define medical devices and convey their product's intention while enhancing their understanding of the compliance landscape.

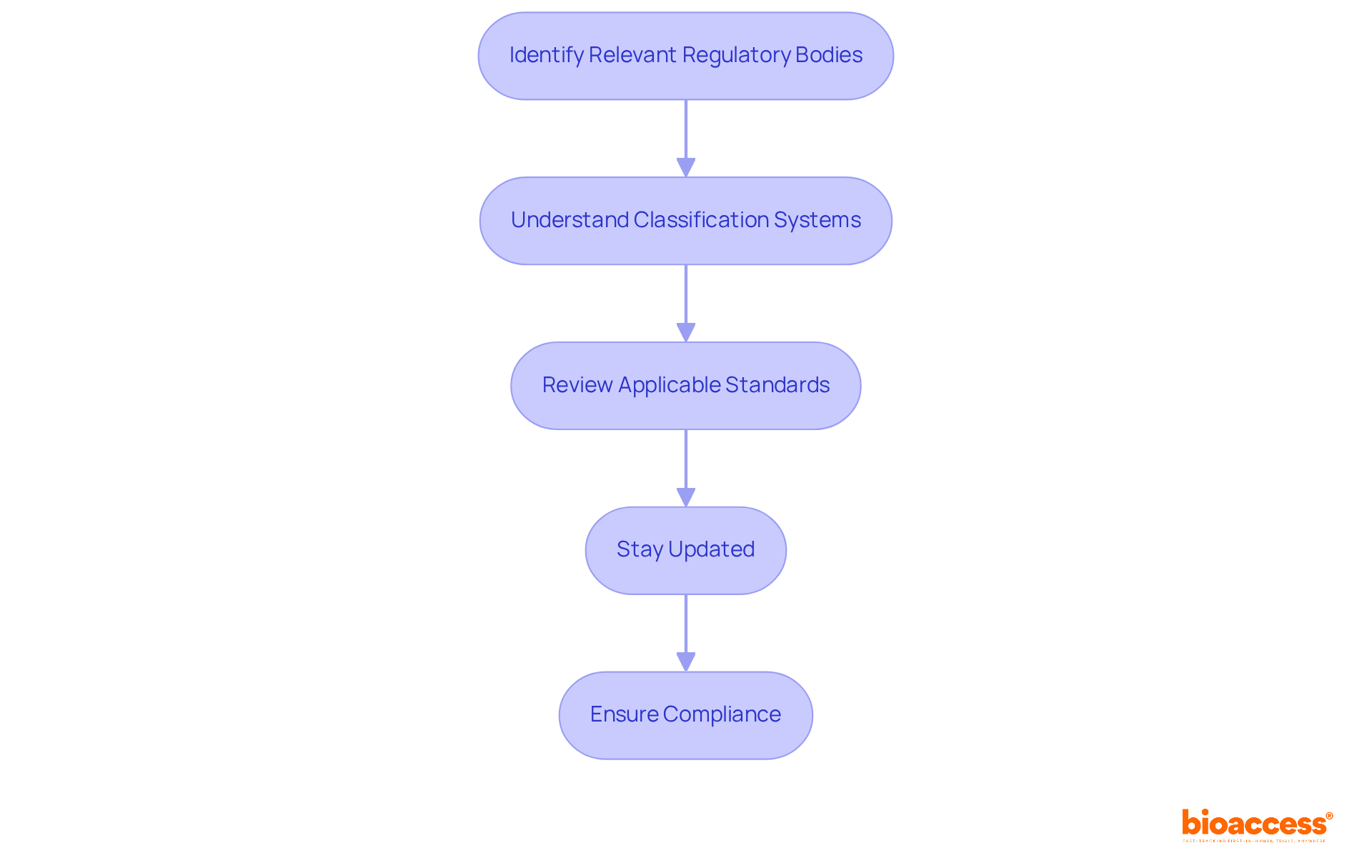
Navigating the regulatory environment for healthcare products necessitates a comprehensive understanding of how to define medical devices according to the key regulations and standards governing the industry. It is essential to consider the following steps:
Identify Relevant Regulatory Bodies: Depending on your target market, familiarize yourself with key organizations such as the FDA in the United States, the EMA in Europe, and the TGA in Australia. In Colombia, INVIMA (Colombia National Food and Drug Surveillance Institute), established in 1992 under the Ministry of Health and Social Protection, plays a critical role in inspecting and overseeing the promotion and production of health products, including medical equipment.
Understand Classification Systems: Medical instruments are categorized into three classes (I, II, III) based on their risk levels. Class I products typically encounter minimal regulatory oversight, while Class III items, deemed high-risk, require thorough pre-market approval, including clinical data submissions. The regulatory agency aims to define medical devices and manage medical equipment, ensuring adherence to these classifications through its Directorate for Medical Equipment and other Technologies.
Review Applicable Standards: Compliance with established standards is paramount. For example, ISO 13485 outlines requirements for quality management systems, whereas IEC 60601 addresses electrical safety. The regulatory authority recommends technical standards for the manufacturing, marketing, surveillance, and quality assurance of devices that define medical devices, which researchers must consider.
Stay Updated: The regulatory environment is dynamic, with frameworks continually evolving. Regularly review updates from pertinent authorities to ensure ongoing compliance with the latest regulations and guidelines. As a Level 4 health authority recognized by PAHO/WHO, INVIMA is equipped to execute health regulation functions, safeguarding the safety, efficacy, and quality of healthcare products.
By adhering to these steps, researchers can effectively navigate the compliance framework, ensuring their healthcare products meet all essential criteria for successful authorization.
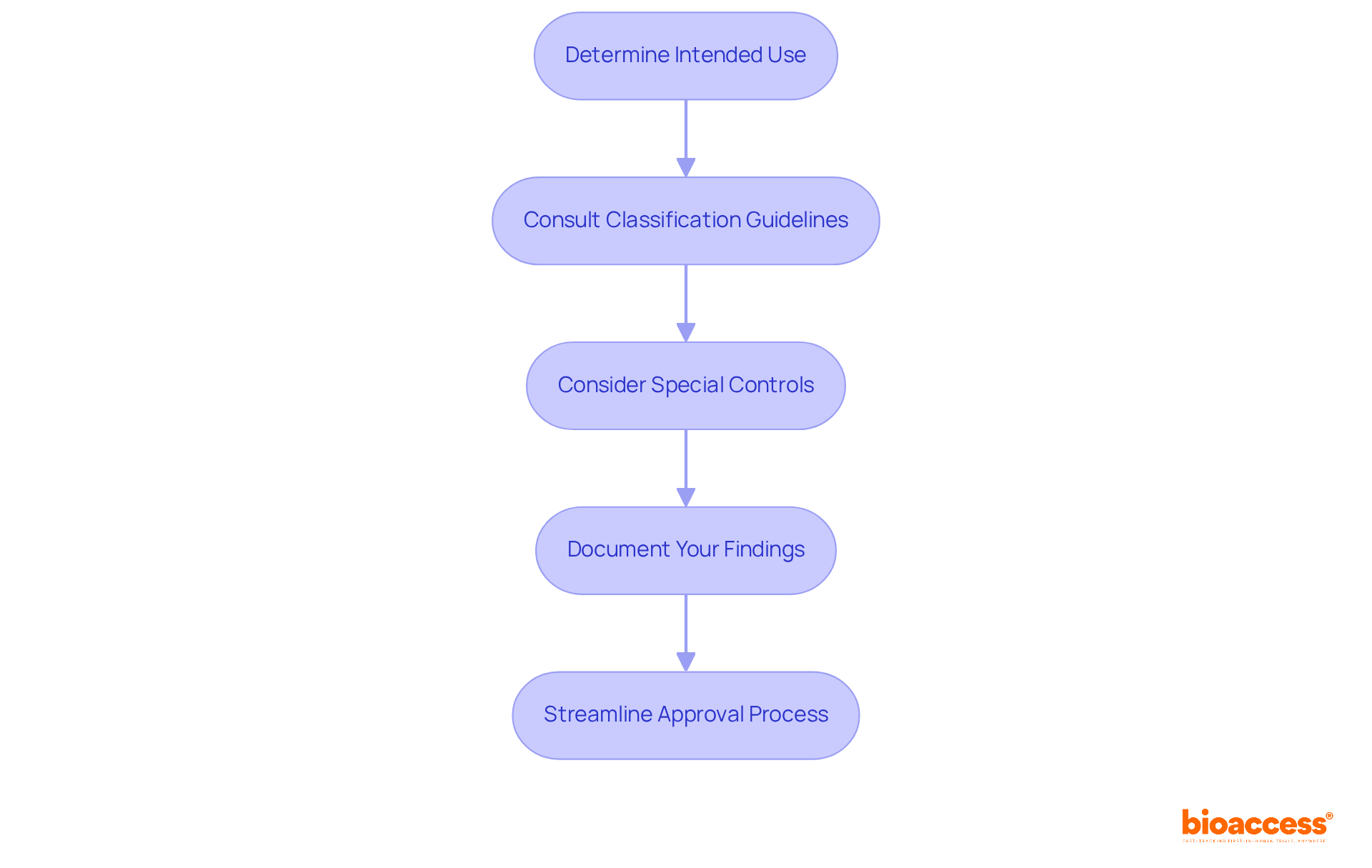
In order to define medical devices, classifying medical equipment necessitates a comprehensive understanding of the various categories and their associated regulatory requirements, particularly within the context of Colombia's regulatory framework. To effectively approach this classification, consider the following steps:
By accurately categorizing health products and following INVIMA's guidelines, researchers can streamline the approval process and ensure compliance with applicable regulations.
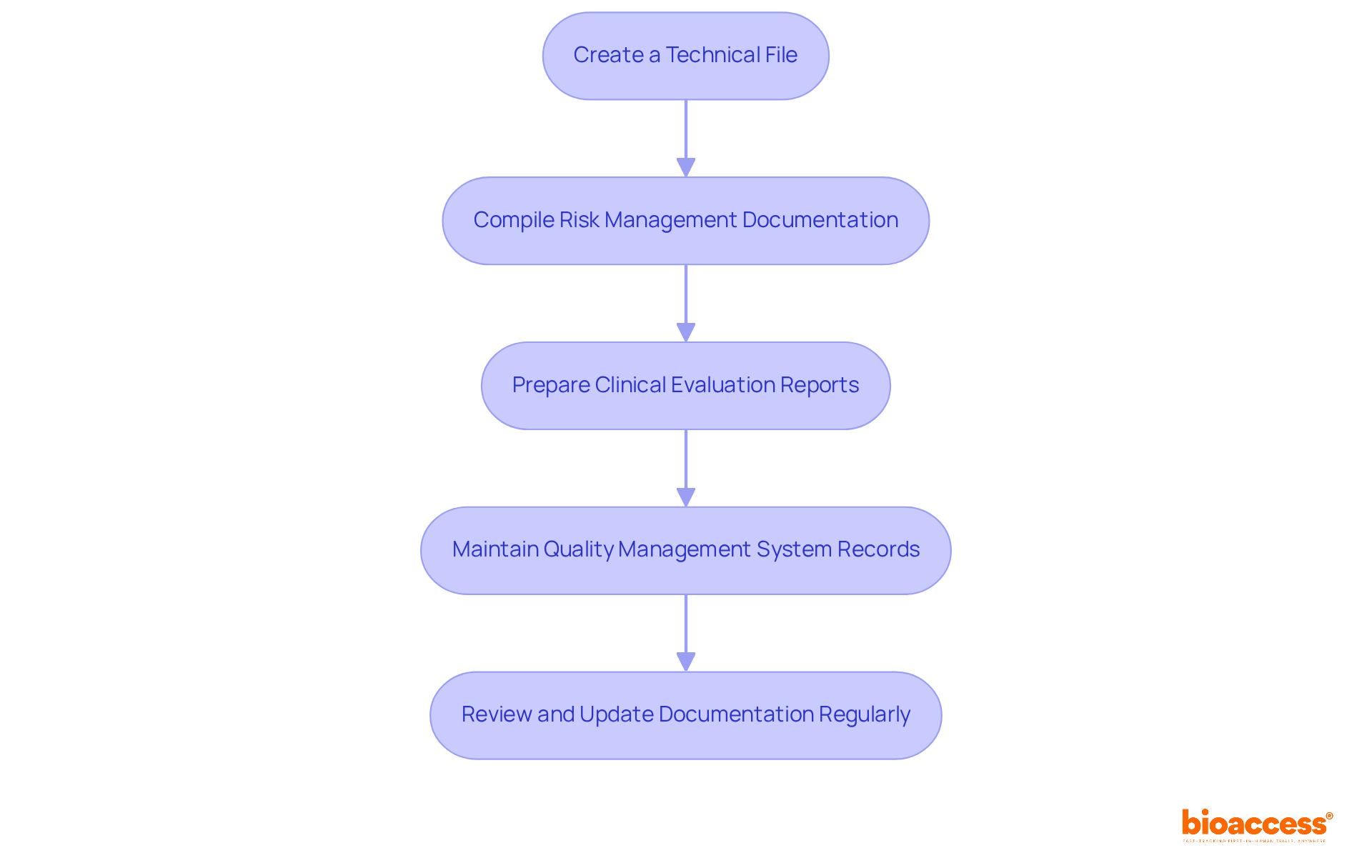
Recording medical equipment is essential for guaranteeing transparency and adherence throughout the compliance process. Here are the essential steps to follow:
Create a Technical File: This file must encompass comprehensive details about the apparatus, including its intended use, design specifications, and manufacturing processes. A well-organized technical document is essential for proving adherence to standards and can greatly affect approval rates.
Compile Risk Management Documentation: Conduct a thorough risk assessment to identify potential hazards linked to the equipment. Recording these risks not only assists in compliance but also improves the safety profile of the product, which is essential for regulatory submissions.
Prepare Clinical Evaluation Reports: If relevant, include data from clinical studies that support the safety and effectiveness of the product. These reports are crucial for illustrating the clinical advantages of the equipment and are frequently examined during the approval procedure.
Maintain Quality Management System (QMS) Records: Ensure that all processes related to the product's development and manufacturing are documented in accordance with ISO 13485. A robust QMS is fundamental for maintaining compliance and ensuring product quality.
Review and Update Documentation Regularly: As regulations evolve and new data emerges, it is imperative to keep all documentation current. Frequent updates guarantee that the technical file and related documents represent the most current information and compliance needs.
In Colombia, the National Institute for the Surveillance of Medicines and Foods plays a crucial role in monitoring the compliance of health instruments. As a Level 4 health authority recognized by the Pan American Health Organization/World Health Organization, INVIMA ensures that health products meet safety, efficacy, and quality standards. Katherine Ruiz, a specialist in compliance matters for healthcare products and in vitro diagnostics, highlights the significance of following these best practices. By adhering to these steps and leveraging the comprehensive services offered by bioaccess, researchers can establish a thorough documentation process that supports compliance and facilitates successful regulatory submissions, ultimately helping to define medical devices and accelerating the path to market for innovative solutions.
Understanding the definition and classification of medical devices is crucial for researchers and developers aiming to navigate the complex landscape of healthcare products. Grasping essential concepts such as intended use and indications for use, along with the regulatory frameworks established by authorities like INVIMA and the FDA, enables stakeholders to ensure that their innovations are effective and compliant with existing standards.
This article delves into the intricacies of defining medical devices, emphasizing the importance of accurately categorizing these products according to their intended use and associated risk levels. Key insights include the necessity of maintaining thorough documentation, adhering to classification systems, and staying updated with evolving regulations. These elements are vital for facilitating smoother approval processes and ensuring that new medical devices meet both safety and efficacy standards.
In a rapidly changing regulatory environment, it is imperative for researchers to remain proactive in their approach to compliance. By prioritizing clear definitions, robust documentation, and alignment with regulatory bodies, the path to market for innovative medical solutions can be significantly expedited. Emphasizing the importance of these practices not only enhances product safety but also contributes to the overall advancement of healthcare technology.
What are medical devices according to the FDA?
The FDA defines medical devices as any tool, apparatus, implement, machine, contrivance, implant, in vitro reagent, or similar article intended for use in the diagnosis, prevention, or treatment of disease.
What is meant by "intended use" of a medical device?
Intended use refers to the specific purpose of the device, whether it is for diagnosis, treatment, or monitoring. It is crucial for the classification and approval processes of medical devices.
What are "indications for use" in the context of medical devices?
Indications for use are the specific conditions or diseases that the medical device is designed to address. Clearly specifying these indications helps align the device with compliance standards and market demands.
Can you provide examples of medical devices?
Medical devices range from basic items like bandages to complex machinery such as MRI machines. Understanding these categories helps in identifying the scope of research and development efforts.
Who regulates medical devices in Colombia?
In Colombia, the regulatory environment for medical devices is overseen by the National Institute for the Surveillance of Medicines and Foods (INVIMA), which ensures the safety, effectiveness, and quality of healthcare products.
What is the role of INVIMA in regulating medical devices?
INVIMA inspects and supervises the marketing and manufacturing of health products, including therapeutic instruments, ensuring adherence to technical standards and best practices.
What upcoming changes are expected from the FDA regarding medical equipment classifications?
By 2025, the FDA will enforce new rules impacting medical equipment classifications, emphasizing the importance of intended use in establishing oversight pathways.
Why is it important for researchers to articulate the intended use of their medical devices?
Clearly articulating the intended use is essential for compliance with evolving oversight criteria and facilitates smoother navigation through the approval process, as different classifications may have distinct requirements for clinical evidence.