


Effective pharmacovigilance services are essential for enhancing clinical trials, as they ensure the safety of investigational medications and improve the integrity of research data. This article underscores that robust monitoring systems can significantly mitigate the risks associated with adverse drug reactions (ADRs). Furthermore, it emphasizes the integration of advanced technologies, such as AI, to streamline drug safety monitoring and ensure compliance with regulatory standards. Ultimately, these measures foster trust in clinical research outcomes, reinforcing the need for reliable pharmacovigilance practices.
Pharmacovigilance stands as a pivotal element in the realm of clinical trials, safeguarding participant health while ensuring the reliability of research findings. With adverse drug reactions contributing significantly to hospital admissions, the integration of effective pharmacovigilance services is essential for enhancing drug safety monitoring. As the landscape evolves with the introduction of advanced technologies and regulatory complexities, clinical trial sponsors face the pressing challenge of optimizing their pharmacovigilance strategies.
How can they navigate these challenges effectively?
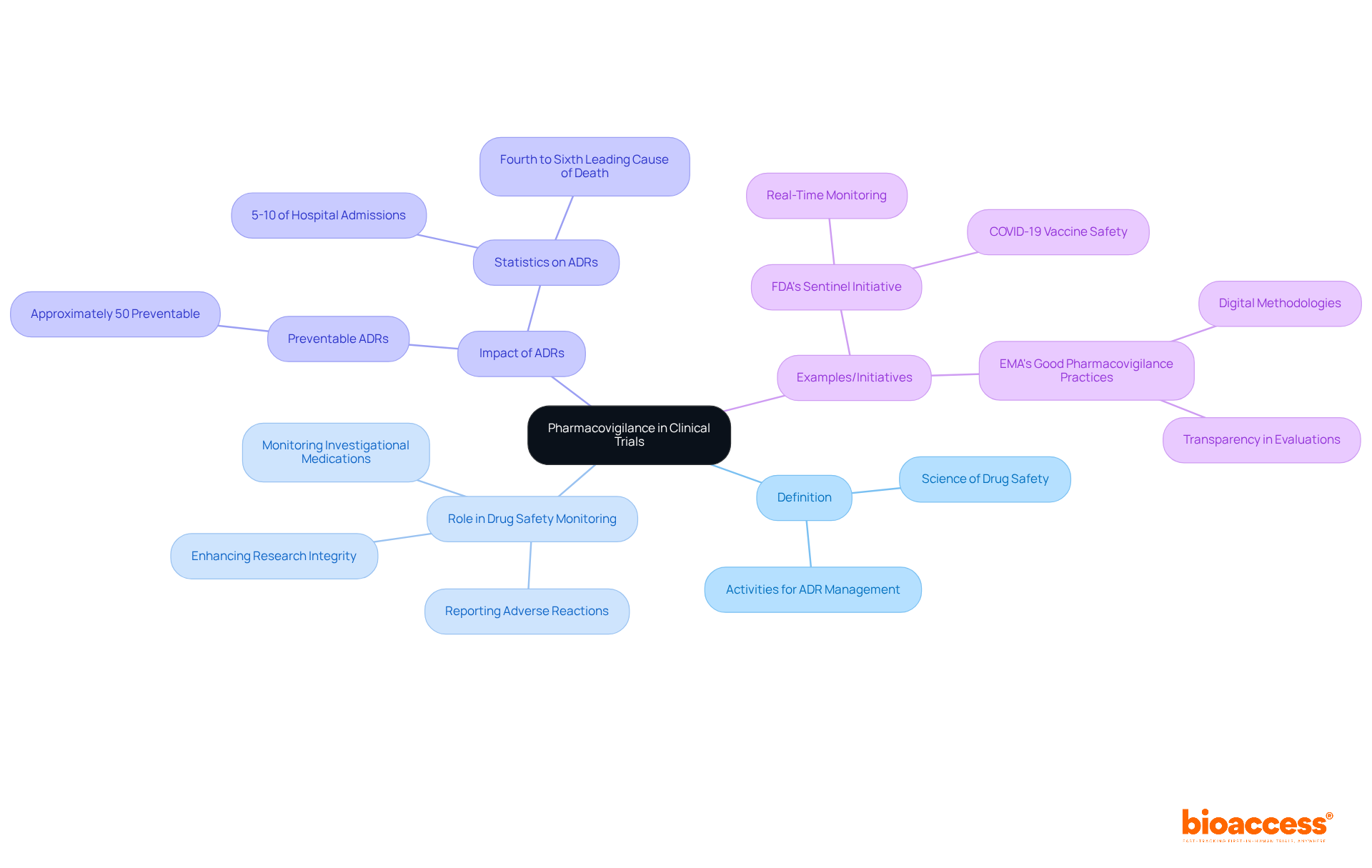
Pharmacovigilance service encompasses the science and activities dedicated to the detection, assessment, understanding, and prevention of adverse drug reactions (ADRs) and other drug-related issues. In the context of medical studies, drug safety monitoring is critical for overseeing the safety of investigational medications, ensuring that any adverse reactions are reported and addressed without delay. Statistics indicate that ADRs account for 5-10% of all hospital admissions, underscoring the necessity for robust monitoring systems to mitigate risks during studies.
The pharmacovigilance service plays a crucial role in effective drug safety monitoring, which not only safeguards participants but also enhances the integrity of research data, vital for regulatory decisions and public health policies. For example, the FDA's Sentinel Initiative has illustrated the efficacy of active surveillance in real-time drug safety monitoring, particularly during the COVID-19 pandemic.
By fostering trust in clinical research outcomes, drug safety monitoring stands as a cornerstone of ethical clinical trial management, ultimately contributing to improved patient safety and confidence in new therapies.
Pharmacovigilance service encompasses a range of activities, including spontaneous reporting systems, cohort studies, and case-control studies. The incorporation of technologies such as electronic health records (EHRs), artificial intelligence (AI), and machine learning (ML) is revolutionizing drug safety monitoring practices. These advanced tools facilitate real-time monitoring of adverse drug reactions (ADRs), significantly enhancing data analysis capabilities and improving signal detection. For instance, AI algorithms can analyze vast datasets to identify potential safety signals more efficiently than traditional methods. Recent findings indicate that AI has enhanced processing times for causality assessments from days to hours, demonstrating its efficiency in monitoring drug safety. By utilizing these technologies, study sponsors can improve their pharmacovigilance service, ensuring a proactive approach to medication safety. However, it is essential to recognize the challenges associated with AI integration, such as data quality issues and the need for regulatory alignment. Integrating expert perspectives, like those from Russ Altman, who highlights the transformative potential of AI in drug safety monitoring, can further reinforce these claims. Additionally, practical examples, such as the implementation of a Bayesian network at UFPorto, illustrate the effectiveness of AI technologies in real-world scenarios. To effectively apply AI and ML in drug safety monitoring, clinical trial sponsors should consider the following steps:
By addressing common pitfalls in AI implementation, sponsors can avoid misapplications and enhance the overall impact of their drug safety efforts.

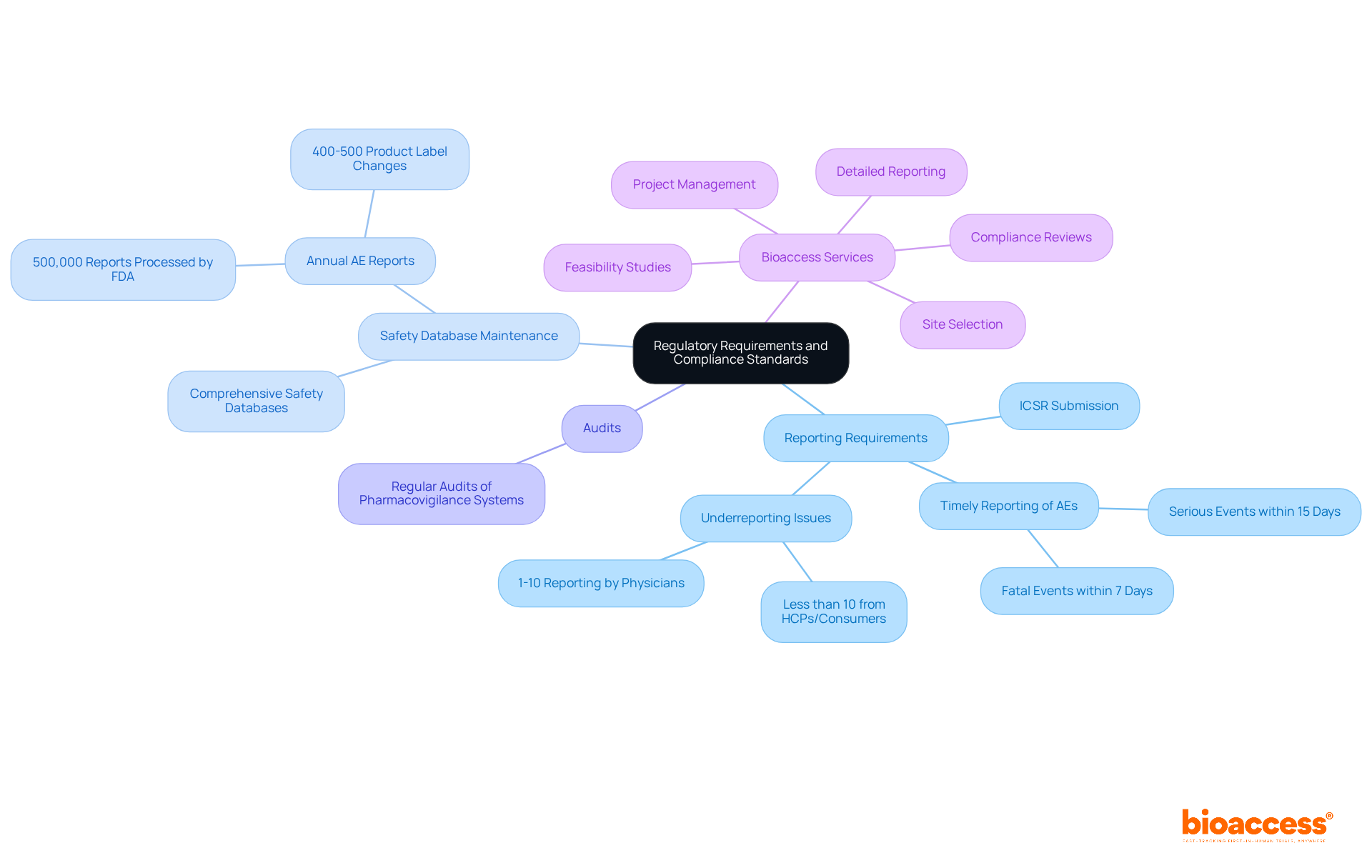
Regulatory requirements for drug safety monitoring are critical in clinical research, varying across regions with organizations such as the FDA, EMA, and WHO establishing essential guidelines. Compliance standards necessitate:
For instance, the FDA mandates that sponsors submit Individual Case Safety Reports (ICSRs) for serious harmful events within 15 calendar days, while fatal or life-threatening incidents must be reported within 7 days. With an estimated 1-10% of significant negative events reported by physicians, the importance of accurate and timely reporting cannot be overstated. Furthermore, the FDA processes approximately 500,000 adverse event reports annually, resulting in an average of 400-500 product label changes each year. This underscores the necessity for research sponsors to remain vigilant and adhere to these regulations.
Bioaccess provides extensive clinical study management services as part of its pharmacovigilance service, designed to ensure compliance with these regulatory requirements. Our services include:
Consistent training and updates on regulatory changes are vital for safety monitoring teams, ensuring they are informed and capable of upholding the integrity of their studies.
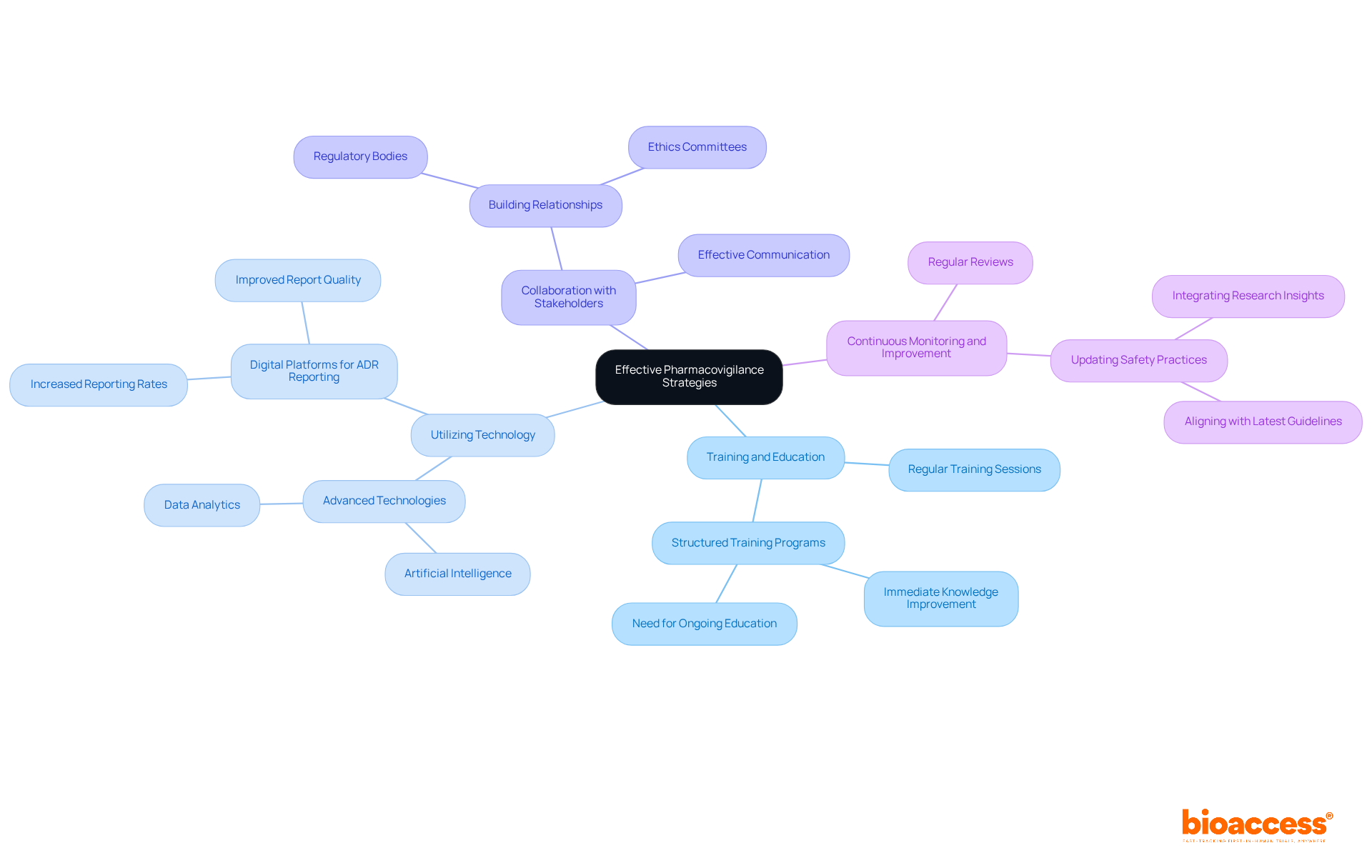
To implement effective safety monitoring strategies, clinical trial sponsors must establish a strong safety system that includes clear protocols for reporting and managing negative events. Key strategies include:
Training and Education: Regular training sessions for staff on medication safety practices and regulatory requirements are essential. Studies have shown that structured training programs significantly enhance knowledge retention and reporting accuracy. For instance, a program at Dokuz Eylul University demonstrated that students' understanding of adverse drug reactions (ADRs) improved immediately after training, although long-term retention highlighted the need for ongoing education.
Utilizing Technology: Advanced technologies such as artificial intelligence and data analytics can significantly enhance signal detection and streamline reporting processes. Digital platforms for ADR reporting have been shown to increase reporting rates and improve the quality of reports, making it easier for healthcare professionals to comply with regulatory requirements.
Collaboration with Stakeholders: Building strong relationships with regulatory bodies, ethics committees, and other stakeholders fosters a collaborative environment for addressing safety concerns. Effective communication and partnership can lead to more comprehensive safety monitoring and quicker responses to potential issues.
Continuous Monitoring and Improvement: Regularly reviewing and updating safety practices based on feedback and new regulatory developments ensures that the system remains effective and compliant. This involves modifying training programs to align with the latest guidelines and integrating insights gained from earlier research studies.
By adopting these strategies, organizations can enhance their pharmacovigilance service efforts, ultimately leading to safer clinical trials and improved patient outcomes.
Pharmacovigilance stands as a cornerstone of clinical trials, crucial for ensuring drug safety and the protection of participants. By systematically monitoring adverse drug reactions and implementing robust safety systems, pharmacovigilance not only enhances the integrity of research data but also nurtures public trust in new therapies. The critical nature of these services cannot be overstated, as they play a pivotal role in shaping ethical clinical trial management and improving patient outcomes.
Throughout this article, we have explored various dimensions of pharmacovigilance, including its definition, the methods and technologies employed, and the regulatory requirements that govern its practice. Key insights reveal that the integration of advanced technologies such as artificial intelligence and machine learning can significantly bolster drug safety monitoring, enabling real-time analysis and efficient signal detection. Furthermore, the emphasis on compliance with regulatory standards and the implementation of effective safety monitoring strategies showcases the multifaceted approach essential for successful pharmacovigilance.
Ultimately, the significance of pharmacovigilance in clinical research transcends mere compliance; it embodies a vital commitment to patient safety and the advancement of medical science. As the landscape of drug development continues to evolve, embracing innovative technologies and fostering collaboration among stakeholders will be imperative for enhancing pharmacovigilance efforts. Organizations are encouraged to prioritize these practices not only to meet regulatory demands but also to ensure the highest standards of safety and efficacy in clinical trials, ultimately benefiting patients and the broader healthcare community.
What is pharmacovigilance?
Pharmacovigilance is the science and activities dedicated to the detection, assessment, understanding, and prevention of adverse drug reactions (ADRs) and other drug-related issues.
Why is pharmacovigilance important in clinical trials?
Pharmacovigilance is critical in clinical trials for overseeing the safety of investigational medications, ensuring that any adverse reactions are promptly reported and addressed, thereby safeguarding participants and enhancing the integrity of research data.
What percentage of hospital admissions are attributed to adverse drug reactions (ADRs)?
ADRs account for 5-10% of all hospital admissions.
How does pharmacovigilance contribute to regulatory decisions and public health policies?
Effective drug safety monitoring through pharmacovigilance provides vital data that informs regulatory decisions and public health policies, ultimately enhancing patient safety.
Can you provide an example of pharmacovigilance in action?
The FDA's Sentinel Initiative is an example of active surveillance in real-time drug safety monitoring, which demonstrated its efficacy during the COVID-19 pandemic.
What role does drug safety monitoring play in clinical research outcomes?
Drug safety monitoring fosters trust in clinical research outcomes, serving as a cornerstone of ethical clinical trial management and contributing to improved patient safety and confidence in new therapies.