


Biocompatibility labs serve as specialized facilities dedicated to evaluating the compatibility of healthcare materials and devices with biological systems. Their critical function is to ensure that these materials do not provoke adverse reactions in human tissues. This article underscores the significance of these labs in the medical device development process, illustrating how rigorous testing protocols—such as cytotoxicity and irritation assessments—are essential for meeting regulatory standards. Such thorough evaluations not only enhance patient safety but also reinforce the credibility of medical innovations in the field. In an ever-evolving Medtech landscape, the role of biocompatibility labs becomes increasingly vital as they address key challenges and contribute to the advancement of healthcare solutions.
Biocompatibility labs serve a pivotal function in healthcare, ensuring that medical devices and materials are safe for human use. As the demand for innovative medical technologies escalates, the importance of these specialized facilities becomes increasingly clear; they not only adhere to stringent regulatory standards but also prioritize patient safety. Yet, with evolving regulations and the complexities of biological interactions, how can manufacturers effectively navigate the intricate landscape of biocompatibility testing to ensure their products meet both safety and efficacy benchmarks?
Biocompatibility labs serve as specialized establishments dedicated to evaluating the compatibility of healthcare instruments and materials with biological systems. Their primary objective is to ensure that these items do not elicit adverse biological responses upon contact with human tissues. This assessment is vital for the development of safe and effective healthcare devices, enabling manufacturers to adhere to stringent regulatory standards and prioritize patient safety.
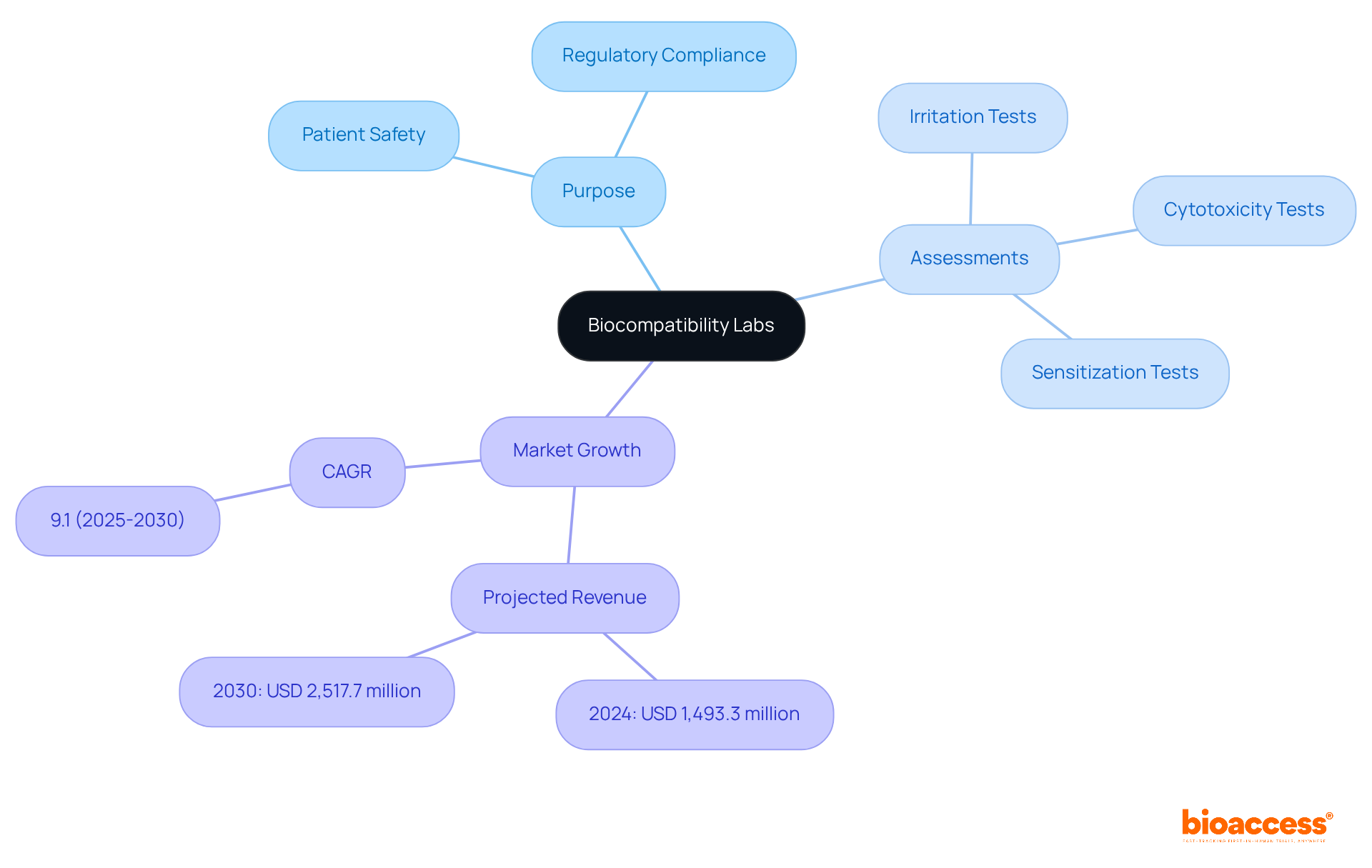
The importance of compatibility evaluation is underscored by the escalating demand for innovative medical technologies. For example, the global biocompatibility tests market generated approximately USD 1,493.3 million in 2024 and is projected to reach USD 2,517.7 million by 2030, representing a compound annual growth rate (CAGR) of 9.1% from 2025 to 2030. This growth is propelled by factors such as increasing healthcare expenditures and a rising prevalence of chronic illnesses, necessitating the creation of safe, implantable solutions.
Biocompatibility evaluation encompasses a variety of assessments, including:
These assessments are critical for determining the safety of substances used in healthcare instruments. For instance, cytotoxicity evaluation identifies substances harmful to cells, while irritation assessment investigates the potential for materials to provoke inflammation. Such rigorous evaluation protocols are essential for ensuring that healthcare instruments, ranging from pacemakers to orthopedic implants, are safe for patient use.
Expert insights highlight the significance of a biocompatibility lab in the healthcare product development process. As regulatory frameworks tighten, the biocompatibility lab's role in providing reliable safety data becomes increasingly crucial. By employing advanced assessment techniques and adhering to international standards, compatibility facilities contribute significantly to the overall safety statistics of medical devices, ultimately enhancing patient outcomes and fostering trust in medical innovations.
The concept of compatibility with living organisms has undergone a profound transformation since its inception. Initially, evaluations were primarily focused on fundamental toxicological assessments, heavily reliant on animal models. However, as healthcare technology has progressed, so too has the understanding of compatibility with living systems, leading to the development of standardized evaluation protocols such as those outlined in ISO 10993. This evolution underscores a heightened awareness of the critical need to evaluate the interactions between medical devices and biological systems in a biocompatibility lab, ensuring that the materials used are safe for human application.
Today, a biocompatibility lab employs a diverse array of methodologies, integrating both in vitro and in vivo assessments to deliver a comprehensive analysis of product safety. The ISO 10993 series, consisting of at least 18 parts, has emerged as a foundational reference in this domain, guiding manufacturers in executing thorough evaluations in a biocompatibility lab that meet regulatory requirements. For instance, ISO 10993-1:2018 emphasizes the importance of assessing the biological risks associated with device materials, while ISO 10993-23:2021 provides updated guidance on skin irritation assessments, advocating for the use of reconstructed human epidermis (RhE) assays in place of traditional animal testing.
Statistical analyses have revealed significant correlations between various physicochemical properties of materials and their biological responses, thereby refining the evaluation process. Notably, a common oversight among companies regarding compatibility with biological materials is the neglect of necessary evaluations, which can lead to regulatory challenges. Case studies highlight the practical ramifications of these advancements; for example, investigations into the influence of porosity in biomaterials have demonstrated that specific pore sizes can enhance vascularization and mitigate fibrosis, resulting in improved healing outcomes. As the landscape of compatibility evaluation continues to evolve, ongoing updates to ISO standards reflect the industry's commitment to ensuring the safety and efficacy of health products, a focus that is often assessed in a biocompatibility lab within an increasingly complex regulatory framework. Akash Sharma emphasizes that compatibility evaluation is a crucial component of healthcare product development, underscoring its importance in meeting regulatory standards.

In the realm of clinical research, the biocompatibility lab plays a pivotal role, characterized by its strict adherence to regulatory standards and protocols, particularly those established by INVIMA, the Colombia National Food and Drug Surveillance Institute. INVIMA plays a crucial role in overseeing the marketing and manufacturing of health products, including medical devices, ensuring compliance with health standards essential for public safety.
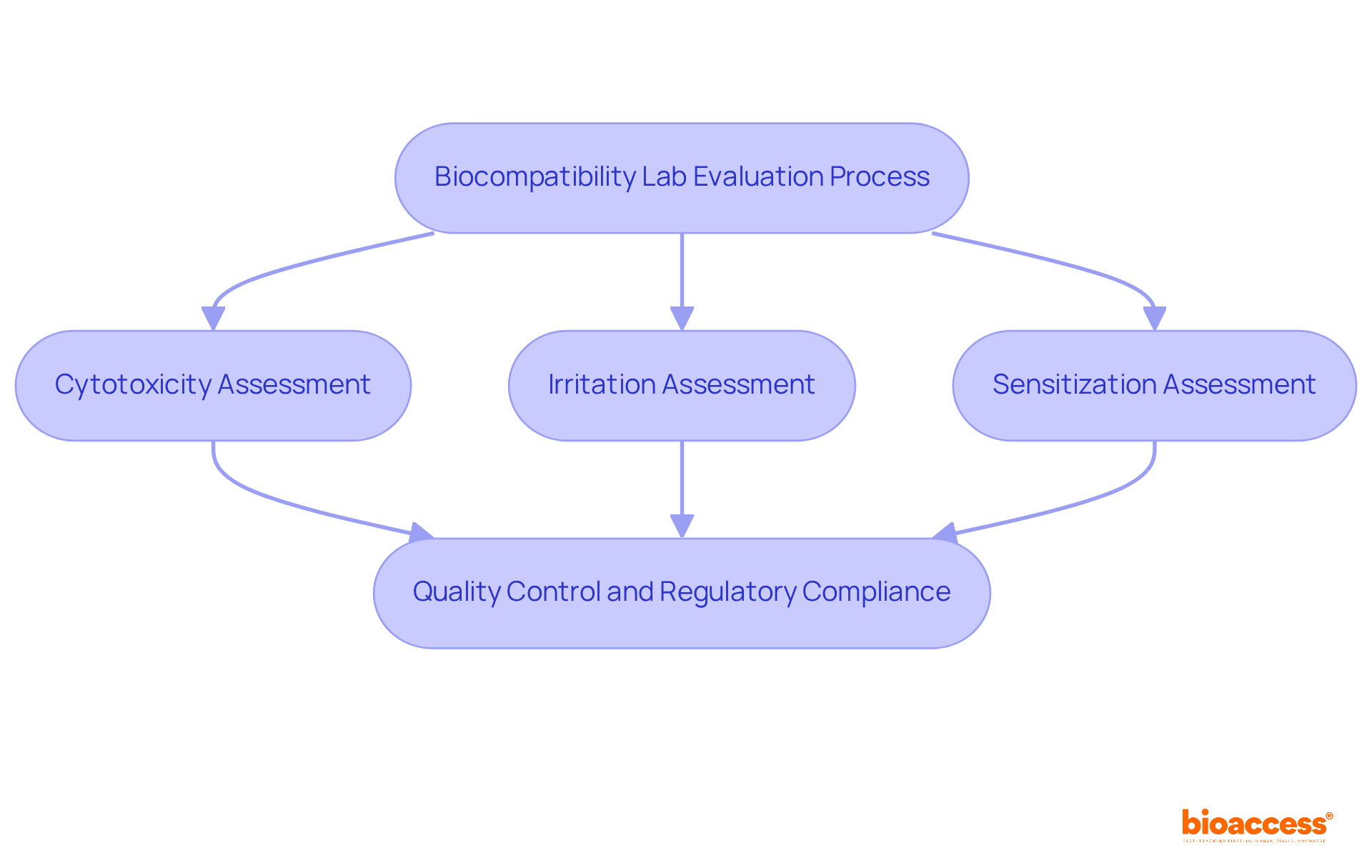
The evaluation procedures in compatibility laboratories include:
These tests employ various methodologies, such as advanced cell culture assays and established animal models, to guarantee comprehensive safety evaluations. Furthermore, the biocompatibility lab is required to uphold rigorous quality control measures, ensuring the reliability and reproducibility of its results, which are critical for regulatory submissions and market approval.
Katherine Ruiz, a specialist in regulatory matters for healthcare instruments, underscores the significance of these evaluation protocols in meeting INVIMA's criteria. The designation of INVIMA as a Level 4 health authority by PAHO/WHO further emphasizes the importance of these regulatory frameworks in ensuring the safety, efficacy, and quality of healthcare products.
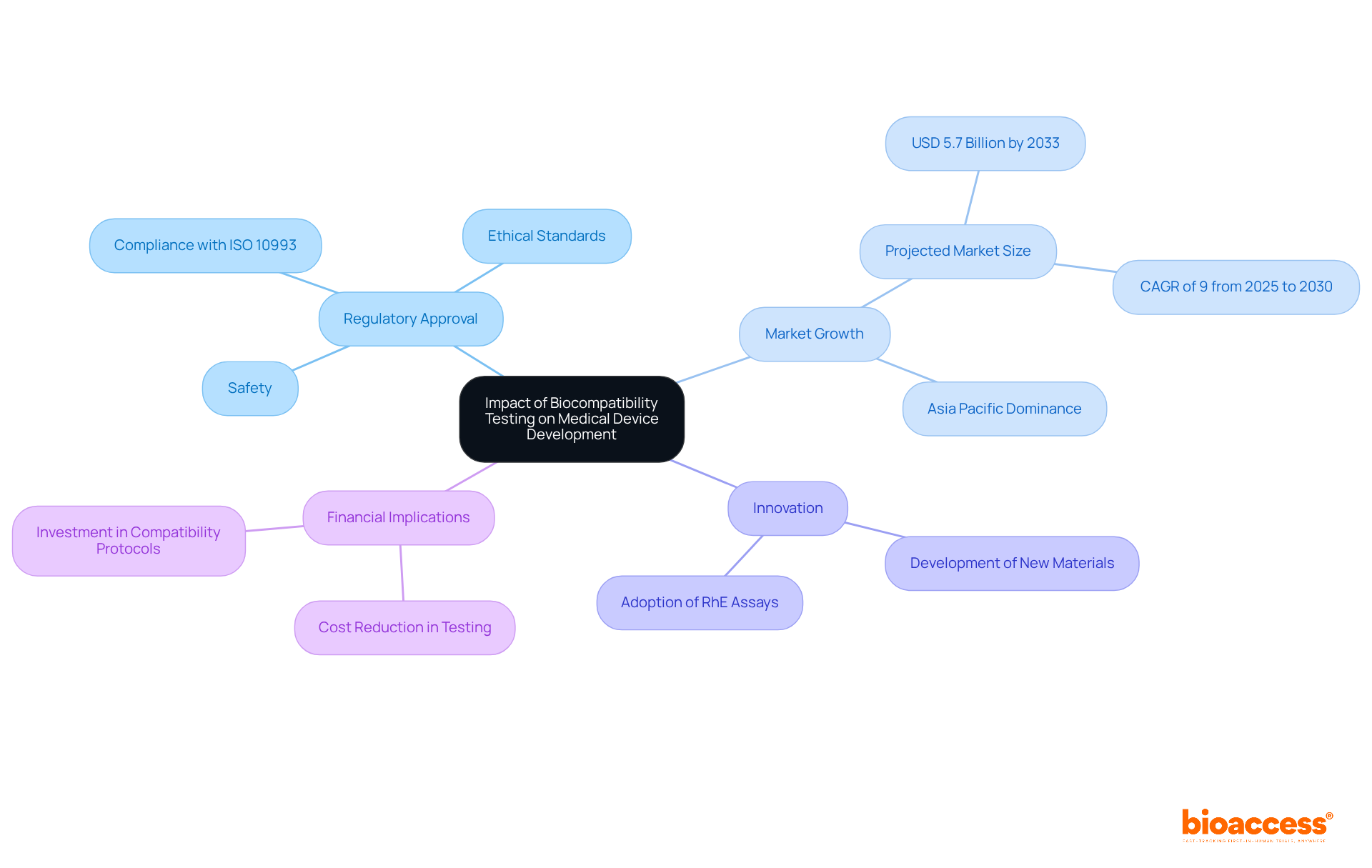
The biocompatibility lab evaluation stands as a cornerstone in the development of medical apparatus, significantly influencing each phase from initial design to market launch. By confirming the biocompatibility lab results of materials used in devices, manufacturers can substantially reduce the likelihood of adverse biological reactions, thereby enhancing patient safety. Effective compatibility evaluations in a biocompatibility lab often serve as a prerequisite for regulatory approval, directly affecting the timeline and costs associated with bringing a product to market. Notably, the market for compatibility evaluations is projected to reach USD 5.7 billion by 2033, reflecting a growing emphasis on safety and efficacy in device development.
Organizations prioritizing compatibility in their development processes are more likely to achieve favorable outcomes. This focus enables them to demonstrate compliance with regulatory standards, fostering trust with healthcare providers and patients alike. Integrating compatibility evaluations during the design phase not only ensures safety but also encourages innovation. Manufacturers are driven to investigate new materials and technologies that enhance device performance while adhering to stringent safety requirements.
Recent case studies underscore the significance of a biocompatibility lab in regulatory approval. For instance, a validation study revealed that reconstituted human epidermis (RhE) assays could produce results comparable to traditional in vivo evaluations, leading to their recognition as the preferred method for irritation assessment. This transition not only expedites the approval process but also reduces reliance on animal testing, aligning with ethical standards and regulatory expectations.
Moreover, the financial implications of compatibility evaluations are substantial. With the market for these evaluations expected to grow at a CAGR of 9% from 2025 to 2030, stakeholders must consider the financial aspects of assessments in their strategic planning. By investing in robust compatibility evaluation protocols, companies can mitigate potential delays and costs linked to regulatory non-compliance, ultimately facilitating a smoother path to market entry.
In conclusion, a biocompatibility lab is integral to the evaluation of medical devices, influencing regulatory approval processes, fostering innovation, and ensuring patient safety. As the industry evolves, it is imperative for manufacturers to remain informed about regulatory updates and advancements in testing methodologies to thrive in a competitive landscape.
Biocompatibility labs are indispensable in the healthcare industry, ensuring that medical devices and materials are safe for human use. Their primary function is to evaluate the compatibility of these products with biological systems, effectively preventing adverse reactions and promoting patient safety. As the demand for innovative medical technologies escalates, the critical nature of rigorous biocompatibility testing cannot be overstated.
Throughout this article, several key points have been emphasized, including the diverse assessments conducted in biocompatibility labs, such as:
The evolution of biocompatibility testing methods, particularly the incorporation of ISO standards, illustrates the increasing recognition of the necessity for comprehensive evaluations. Moreover, the influence of these labs on medical device development is profound, affecting regulatory approval processes and fostering innovation while ensuring adherence to safety standards.
Ultimately, the significance of biocompatibility testing extends beyond mere regulatory compliance; it is a vital component of healthcare product development that directly impacts patient outcomes. Manufacturers are urged to prioritize compatibility evaluations in their design processes, as this not only enhances safety but also propels innovation in medical technologies. By remaining informed about current trends and advancements in biocompatibility testing, stakeholders can play a crucial role in contributing to a safer and more effective healthcare landscape.
What is the purpose of biocompatibility labs?
Biocompatibility labs evaluate the compatibility of healthcare instruments and materials with biological systems to ensure they do not cause adverse biological responses when in contact with human tissues.
Why is biocompatibility evaluation important?
It is vital for the development of safe and effective healthcare devices, helping manufacturers meet regulatory standards and prioritize patient safety, especially given the increasing demand for innovative medical technologies.
What is the projected growth of the biocompatibility tests market?
The global biocompatibility tests market generated approximately USD 1,493.3 million in 2024 and is projected to reach USD 2,517.7 million by 2030, with a compound annual growth rate (CAGR) of 9.1% from 2025 to 2030.
What factors are driving the growth of the biocompatibility tests market?
The growth is driven by increasing healthcare expenditures and a rising prevalence of chronic illnesses, which necessitate the creation of safe, implantable solutions.
What types of assessments are included in biocompatibility evaluation?
Biocompatibility evaluation includes assessments such as cytotoxicity, irritation, and sensitization tests.
What does cytotoxicity evaluation determine?
Cytotoxicity evaluation identifies substances that are harmful to cells.
What does irritation assessment investigate?
Irritation assessment investigates the potential for materials to provoke inflammation.
How do biocompatibility labs contribute to patient safety?
By employing advanced assessment techniques and adhering to international standards, biocompatibility labs provide reliable safety data that enhances patient outcomes and fosters trust in medical innovations.