


This article delves into the treatment options and limitations associated with chronic total occlusion (CTO) of the right coronary artery (RCA). It underscores that effective management may encompass:
Among these, PCI emerges as a prevalent choice, albeit with its inherent technical challenges and variable success rates. Such factors necessitate meticulous patient selection and careful consideration of potential complications.
Chronic Total Occlusion (CTO) of the right coronary artery transcends mere medical terminology; it embodies a formidable challenge in cardiovascular health that can result in debilitating symptoms and severe complications. Recognizing the treatment options available for this condition is essential, as timely and effective interventions can greatly enhance patient outcomes.
However, the treatment landscape is complex and fraught with limitations, prompting critical inquiries regarding the optimal management of RCA occlusions. What strategies can healthcare providers employ to adeptly navigate these challenges and elevate patient care?
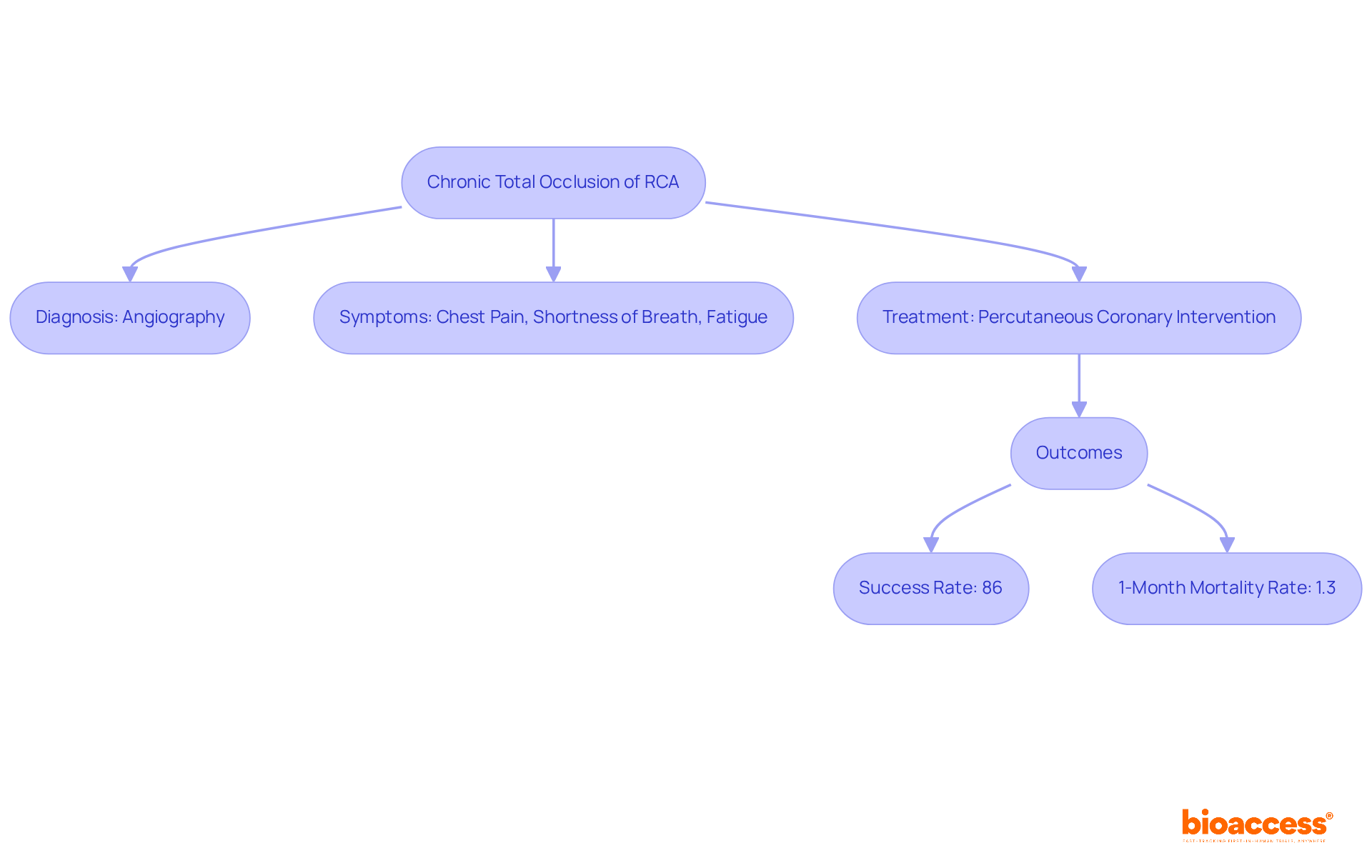
Chronic Total Occlusion (CTO) of the occluded RCA is marked by a complete blockage of the artery that lasts three months or longer, as shown by angiographic findings. This condition typically stems from atherosclerosis, where plaque accumulates in the arterial walls, culminating in a 100% occlusion. Such a blockage critically impairs blood flow to the heart muscle, potentially leading to symptoms like chest pain, shortness of breath, and fatigue.
Recognizing this definition is crucial for understanding the urgency and possible complications associated with occluded RCA; timely intervention can greatly influence patient outcomes. Recent studies reveal that CTOs are often identified through coronary angiography, a procedure that employs contrast dye to visualize blood flow and inform treatment strategies.
According to the Cleveland Clinic, effective management of occluded RCA CTO can enhance patient quality of life and mitigate the risk of severe complications. Notably, the procedural success rate of percutaneous coronary intervention (PCI) for CTO is reported to be as high as 86%, while the 1-month mortality rate for CTO PCI patients hovers around 1.3%. Furthermore, it is vital to acknowledge that CTO PCI procedures exhibit higher complication rates compared to non-CTO PCI, underscoring the need for meticulous consideration in treatment planning.
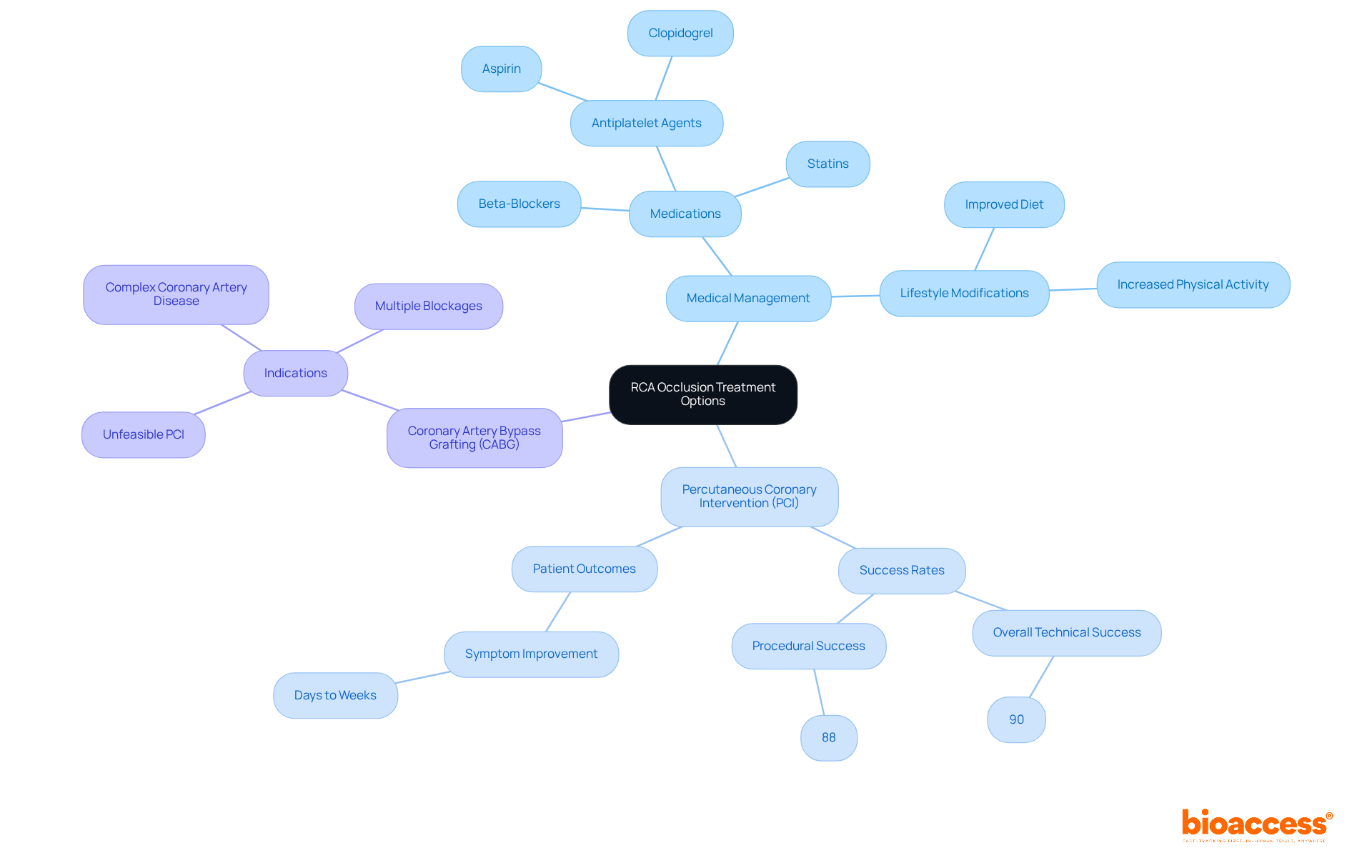
Treatment options for managing occluded RCA include medical management, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG).
Medical Management: This strategy typically encompasses medications such as antiplatelet agents (e.g., aspirin, clopidogrel), beta-blockers, and statins to alleviate symptoms and mitigate cardiovascular risks. Additionally, lifestyle modifications—such as improved diet and increased physical activity—are strongly encouraged to enhance overall heart health.
Percutaneous Coronary Intervention (PCI): PCI is a minimally invasive technique that employs catheters to reopen blocked arteries, often followed by stent placement to maintain arterial patency. Recent advancements in PCI technology have yielded success levels nearing 90% for procedures addressing occluded RCA CTO, with an overall technical success level of 90% and a procedural success level of 88%. Notably, patients who undergo CTO PCI frequently experience symptom improvement within days to weeks, making this option increasingly viable. Furthermore, RCA-CTO has been significantly associated with target lesion revascularization (TLR) and target vessel revascularization (TVR), underscoring the implications of occluded RCA and treatment outcomes.
Coronary Artery Bypass Grafting (CABG): When PCI is deemed unfeasible or unsuccessful, CABG may be indicated. This surgical procedure establishes an alternative route for blood flow to the heart by grafting a vessel from another body part. CABG is generally reserved for patients with complex coronary artery disease or multiple blockages, ensuring that those with the most severe conditions receive appropriate care.
Each treatment modality presents distinct indications, benefits, and risks, necessitating a tailored approach that considers the individual patient's clinical status and preferences.
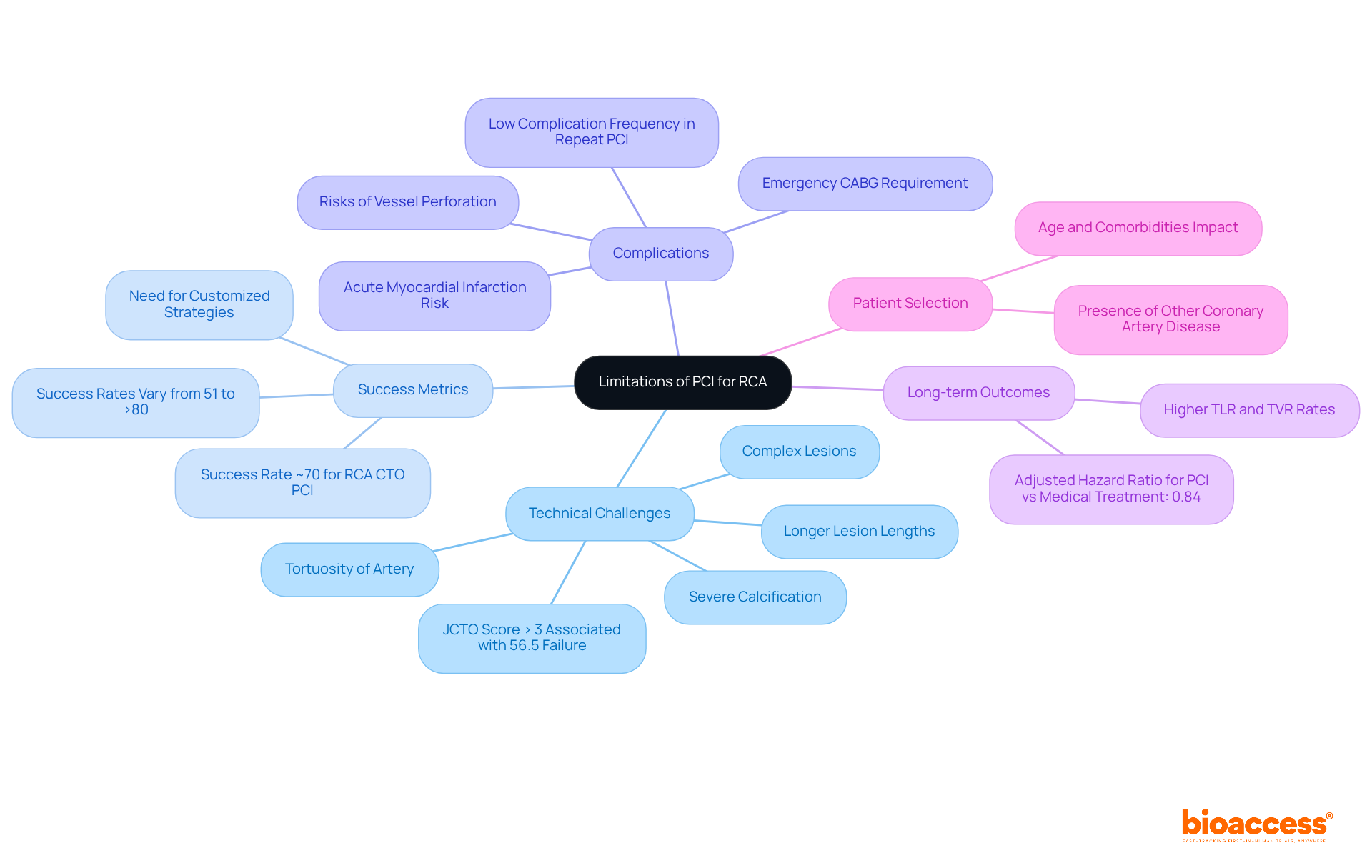
While PCI is a widely utilized treatment for occluded RCA, it has its limitations.
Technical Challenges: RCA CTOs often present unique technical difficulties due to the complexity of the lesions, including longer lesion lengths, severe calcification, and tortuosity of the artery. These factors can complicate the procedure and increase the risk of failure. Notably, a JCTO score greater than 3 has been associated with failure in 56.5% of cases involving occluded RCA, underscoring the necessity for experienced operators and advanced techniques.
Success Metrics: Although advancements in technology have improved PCI success metrics, studies indicate that the success level for RCA CTO PCI, particularly in cases of occluded RCA, can be lower compared to other coronary arteries. For instance, a recent study reported a success percentage of approximately 70% for procedures involving occluded RCA CTO, which is lower than that for non-CTO interventions. The success percentages for CTO PCI can vary from 51% to more than 80%, highlighting the variability and the necessity for customized strategies in these situations.
Complications: The procedure carries risks of complications such as vessel perforation, acute myocardial infarction, and the need for emergency CABG. The overall complication frequency for repeat PCI was low, with only two periprocedural myocardial infarctions reported, indicating that while risks are present, they can be managed effectively. These risks are heightened in patients with complex lesions involving an occluded RCA.
Long-term Outcomes: Patients who undergo PCI for occluded RCA CTO may experience higher rates of target lesion revascularization (TLR) and target vessel revascularization (TVR) compared to those treated for non-CTO lesions. The adjusted hazard ratio for successful PCI compared to medical treatment is 0.84, suggesting that while PCI can provide immediate relief, the long-term durability of the intervention may be less favorable.
Patient Selection: Not all patients are suitable candidates for PCI. Factors such as age, comorbidities, and the presence of other coronary artery disease can influence the decision to proceed with PCI versus alternative treatments.
Understanding these limitations is essential for healthcare providers to make informed decisions and manage patient expectations effectively.
Chronic Total Occlusion (CTO) of the Right Coronary Artery (RCA) represents a significant cardiovascular challenge, characterized by a complete blockage that can lead to serious health complications. Understanding the nature of this condition is essential for effective management and treatment, as timely intervention can dramatically improve patient outcomes. This article highlights various treatment options, including:
Each with its unique benefits and limitations.
Key insights reveal that while PCI offers a minimally invasive approach with high success rates, it is not without challenges. Technical difficulties, variability in success rates, potential complications, and the importance of patient selection underscore the need for careful consideration when determining the most appropriate treatment path. A tailored approach is vital for optimizing outcomes in patients with RCA CTO.
In light of these findings, healthcare providers are encouraged to remain informed about the latest advancements and limitations in the treatment of RCA occlusions. This knowledge not only aids in making informed clinical decisions but also empowers patients to engage in discussions about their treatment options. As the landscape of cardiology evolves, continuous education and adaptation to emerging therapies will be crucial for improving patient care and outcomes for those affected by chronic total occlusion of the right coronary artery.
What is Chronic Total Occlusion (CTO) of the Right Coronary Artery (RCA)?
Chronic Total Occlusion of the RCA is a complete blockage of the artery that lasts three months or longer, typically caused by atherosclerosis, which leads to a 100% occlusion and impaired blood flow to the heart muscle.
What are the symptoms of a Chronic Total Occlusion of the RCA?
Symptoms may include chest pain, shortness of breath, and fatigue due to the impaired blood flow to the heart muscle.
How is Chronic Total Occlusion of the RCA diagnosed?
CTOs are often identified through coronary angiography, a procedure that uses contrast dye to visualize blood flow in the arteries.
What is the significance of recognizing Chronic Total Occlusion of the RCA?
Recognizing CTO is crucial for understanding the urgency and potential complications associated with the condition, as timely intervention can significantly influence patient outcomes.
What are the treatment options for Chronic Total Occlusion of the RCA?
Effective management often involves percutaneous coronary intervention (PCI), which has a reported success rate of up to 86%.
What is the mortality rate for patients undergoing PCI for Chronic Total Occlusion?
The 1-month mortality rate for patients undergoing PCI for CTO is approximately 1.3%.
Are there any complications associated with PCI for Chronic Total Occlusion?
Yes, CTO PCI procedures exhibit higher complication rates compared to non-CTO PCI, highlighting the need for careful treatment planning.