


This article delineates the critical distinctions between accuracy and precision in clinical research, underscoring their paramount importance for reliable data and patient safety.
In the realm of clinical research, accuracy and precision are not merely academic terms; they are the foundational elements upon which successful medical trials are constructed.
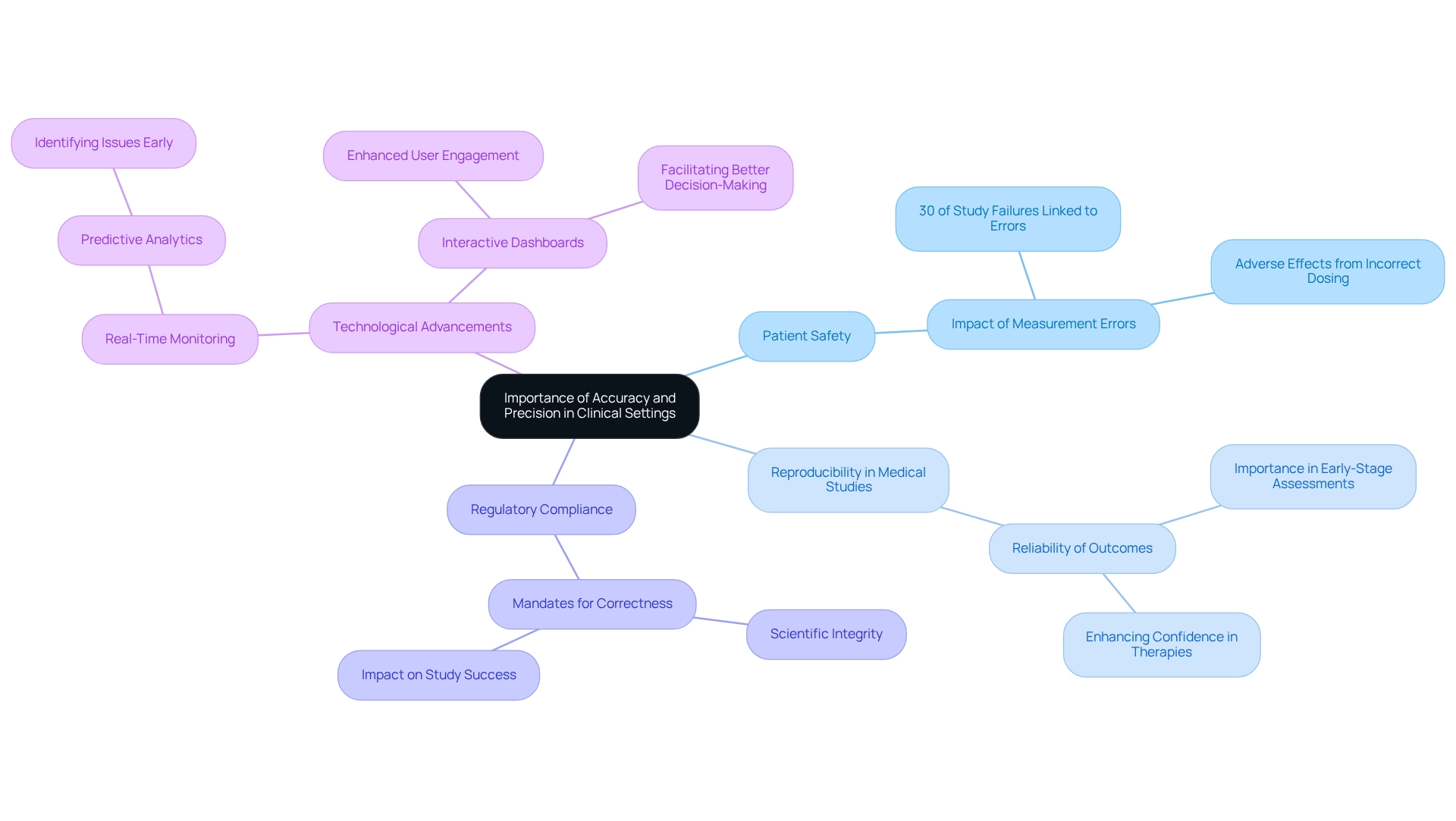
This article delves into the significance of accuracy and precision in clinical settings, explores strategies to enhance these attributes, and highlights the role of technology in achieving superior outcomes in research.
In clinical research, the distinction of precise versus accurate is defined as the degree to which a measured value aligns with the true value or actual parameter being assessed. For instance, if a blood pressure monitor consistently displays 120/80 mmHg while the true blood pressure is 130/85 mmHg, it is deemed accurate if the average of its readings approaches the true value. This underscores the significance of calibration; adjusting a scale can greatly enhance its accuracy.
Conversely, exactness pertains to the consistency of measurements, regardless of their proximity to the actual value. For example, if the same blood pressure monitor reliably shows 130/85 mmHg, it indicates exactness but lacks correctness if the actual value varies.
Essentially, correctness refers to being right, while consistency pertains to reliability. Both components are crucial for producing dependable results in medical research. Understanding the distinctions of precise versus accurate is vital for researchers striving to produce valid and reproducible results. A case study illustrating this concept involved the creation of a shared database, where the optimal outcome was achieved when the database maintained both accuracy and precision, thereby enhancing collaboration across multiple projects. This highlights the essential function that accurate and precise measurements serve in the success of medical studies.
With more than 20 years of experience in medical research, bioaccess® emphasizes the significance of these concepts in ensuring successful studies. Their extensive trial management services, including Early-Feasibility Studies, First-In-Human Studies, feasibility studies, site selection, compliance reviews, trial setup, import permits, project management, and reporting, are designed to uphold the highest standards of correctness and exactness. Moreover, the utilization of sophisticated instruments such as business intelligence dashboards for exact data visualization and trend analysis is increasingly crucial in sustaining correctness and exactness in medical research.

In medical environments, understanding the difference between precise versus accurate is paramount. The distinction between precise versus accurate measurements forms the foundation for ensuring that treatments are based on reliable data, which is vital for patient safety. For instance, incorrect dosing of medication can lead to adverse effects or treatment failures, underscoring the necessity for precision in medical applications.
Equally vital is understanding the differences between precise versus accurate measurements for reproducibility in medical studies. Unreliable outcomes hinder the ability to reach sound conclusions or replicate studies, particularly in early-stage assessments where establishing a dependable safety profile is crucial. Regulatory agencies mandate proof of both correctness and the concept of precise versus accurate in medical research, making compliance with these standards not only a matter of scientific integrity but also a regulatory necessity that can significantly impact the success of studies and the approval of healthcare products.
With over 20 years of experience in the field, bioaccess® recognizes that inaccuracies in measurements can lead to substantial challenges in healthcare environments. Research indicates that up to 30% of medical study failures are linked to measurement errors, highlighting the critical distinction between precise versus accurate measurements. Furthermore, understanding the difference between precise versus accurate measurements in research reproducibility is essential, as reproducible outcomes enhance the reliability of discoveries and foster confidence in novel therapies.
Bioaccess® specializes in managing a diverse array of medical studies in Latin America, including Early-Feasibility Studies (EFS), First-In-Human Studies (FIH), Pilot Studies, Pivotal Studies, and Post-Market Medical Follow-Up Studies (PMCF). This comprehensive approach ensures that all management elements are executed with a focus on correctness and exactness, ultimately facilitating the advancement of medical devices and biopharmaceuticals.
Advancements in real-time monitoring are paving the way for safer and more reliable treatments for patients globally. As Meri Beckwith, Co-Founder of bioaccess®, articulates, "The integration of advanced technologies such as artificial intelligence and machine learning into real-time monitoring systems allows for predictive analytics, which can identify potential issues before they escalate." This underscores the significance of technology in achieving precise versus accurate outcomes in medical research.
Case studies, such as the implementation of interactive dashboards in medical research, illustrate how enhanced data visualization can elevate user engagement and enable better decision-making. At bioaccess®, these technologies contribute to outcomes in research that emphasize the difference between precise versus accurate, ultimately supporting the progression of medical devices and biopharmaceuticals.
To enhance accuracy and precision in clinical research, it is essential to implement the following strategies:
By incorporating these strategies into research practices, researchers can significantly enhance data quality, resulting in more dependable and influential outcomes. For instance, continuous monitoring has been shown to enhance trial effectiveness, paving the way for safer and more reliable treatments for patients worldwide. As Junichi Ishigami, MD, MPH, noted, the approval of studies by institutional review boards is crucial for maintaining the integrity of clinical research.

The significance of accuracy and precision in clinical research is paramount. These foundational elements guarantee that measurements align closely with true values while ensuring consistent reproducibility, which is essential for generating reliable outcomes. Inaccuracies can lead to detrimental effects, such as adverse patient outcomes or failed treatments, highlighting the necessity for adherence to high standards in data collection and analysis.
Implementing strategies such as standardizing protocols, regular training, and continuous monitoring significantly enhances both accuracy and precision in clinical trials. By prioritizing these practices, researchers can minimize variability and bolster the credibility of their findings. The integration of advanced technologies, including real-time monitoring systems and artificial intelligence, further supports these efforts, enabling timely identification of issues and fostering trust in new medical treatments.
Ultimately, the pursuit of accuracy and precision in clinical research transcends scientific integrity; it is crucial for patient safety and the successful advancement of medical therapies. As the landscape of clinical research continues to evolve, a steadfast commitment to these principles will ensure that innovative treatments are both effective and safe, paving the way for improved patient care and outcomes.
What is the difference between accuracy and precision in clinical research?
Accuracy refers to the degree to which a measured value aligns with the true value or actual parameter being assessed, while precision pertains to the consistency of measurements, regardless of their proximity to the actual value.
Can you provide an example to illustrate accuracy and precision?
For instance, if a blood pressure monitor consistently displays 120/80 mmHg while the true blood pressure is 130/85 mmHg, it is deemed accurate if the average of its readings approaches the true value. If the monitor reliably shows 130/85 mmHg, it indicates precision but lacks accuracy if the actual value varies.
Why is calibration important in measurements?
Calibration is significant because adjusting a scale can greatly enhance its accuracy, ensuring that measured values are closer to the true values.
What do correctness and consistency mean in the context of medical research?
Correctness refers to being right, while consistency pertains to reliability. Both are crucial for producing dependable results in medical research.
Why is understanding the distinction between precise and accurate measurements vital for researchers?
Understanding these distinctions is essential for researchers striving to produce valid and reproducible results in their studies.
How does a shared database relate to accuracy and precision in medical studies?
A case study showed that the optimal outcome was achieved when a shared database maintained both accuracy and precision, enhancing collaboration across multiple projects.
What role does bioaccess® play in ensuring accuracy and precision in medical research?
Bioaccess® emphasizes the significance of accuracy and precision in ensuring successful studies and offers extensive trial management services designed to uphold high standards of correctness and exactness.
What tools does bioaccess® use to maintain correctness and exactness in research?
Bioaccess® utilizes sophisticated instruments such as business intelligence dashboards for exact data visualization and trend analysis, which are crucial for sustaining correctness and exactness in medical research.