


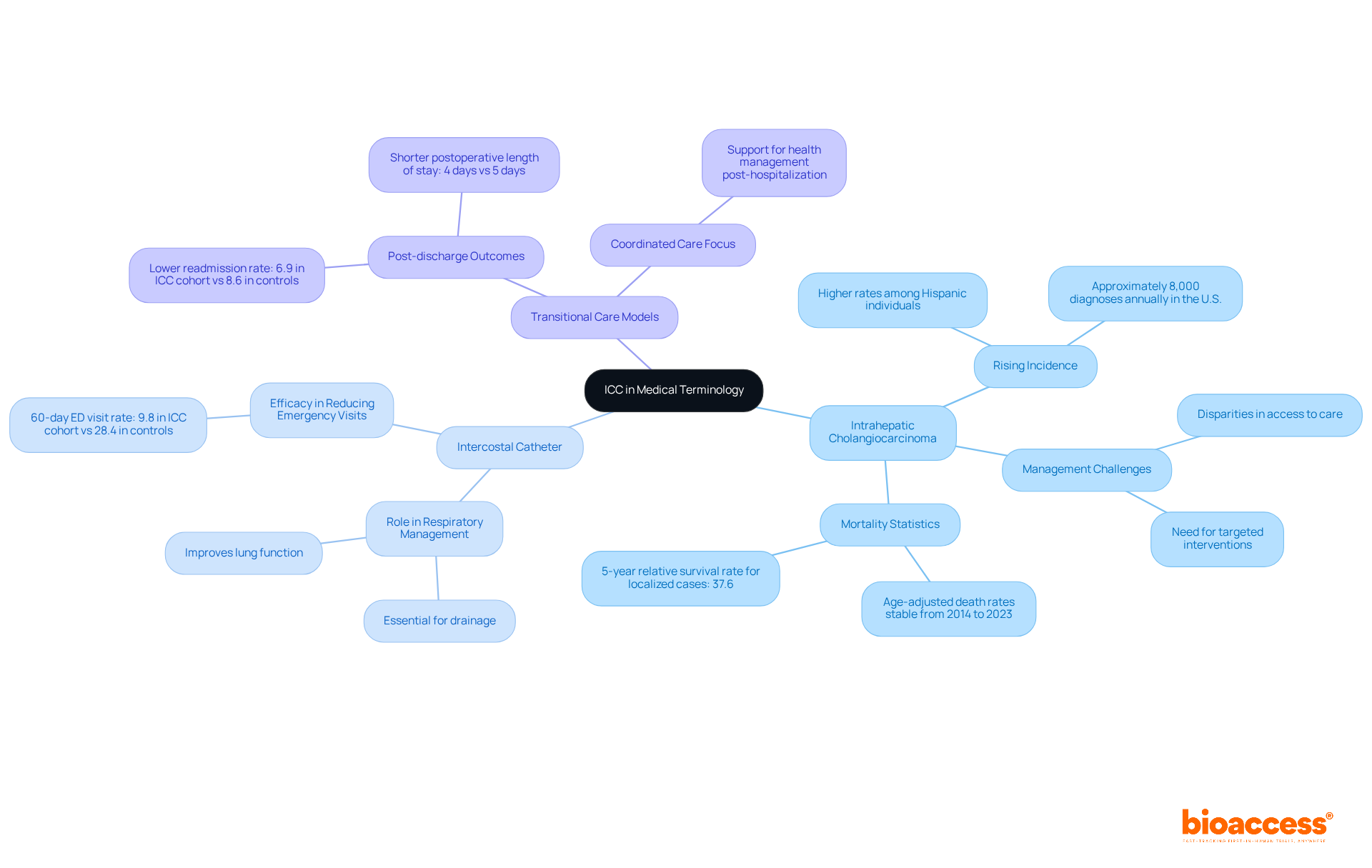
The ICC abbreviation in medical terminology primarily signifies Intercostal Catheter and Intrahepatic Cholangiocarcinoma, both of which hold considerable importance in healthcare. This article elucidates how Intercostal Catheters enhance postoperative recovery and pain management. Furthermore, it underscores the critical need for early detection and effective treatment strategies for Intrahepatic Cholangiocarcinoma, particularly in light of its rising incidence and poor survival rates. This highlights the necessity of comprehending these terms within clinical contexts.
Understanding medical abbreviations can indeed pose a challenge, particularly when a single term encompasses multiple critical meanings. The abbreviation "ICC" in healthcare is especially multifaceted, representing essential concepts such as:
Each of these interpretations plays a significant role in improving patient outcomes and advancing clinical practices. Yet, what occurs when the complexities of these terms intersect with the urgent need for effective treatment and care coordination? Exploring the implications of ICC not only underscores its importance in medical terminology but also highlights the pressing challenges faced in today’s healthcare landscape.
The ICC abbreviation medical encompasses several significant healthcare terms, including Intercostal Catheter, Intrahepatic Cholangiocarcinoma, and Integrated Comprehensive Care.
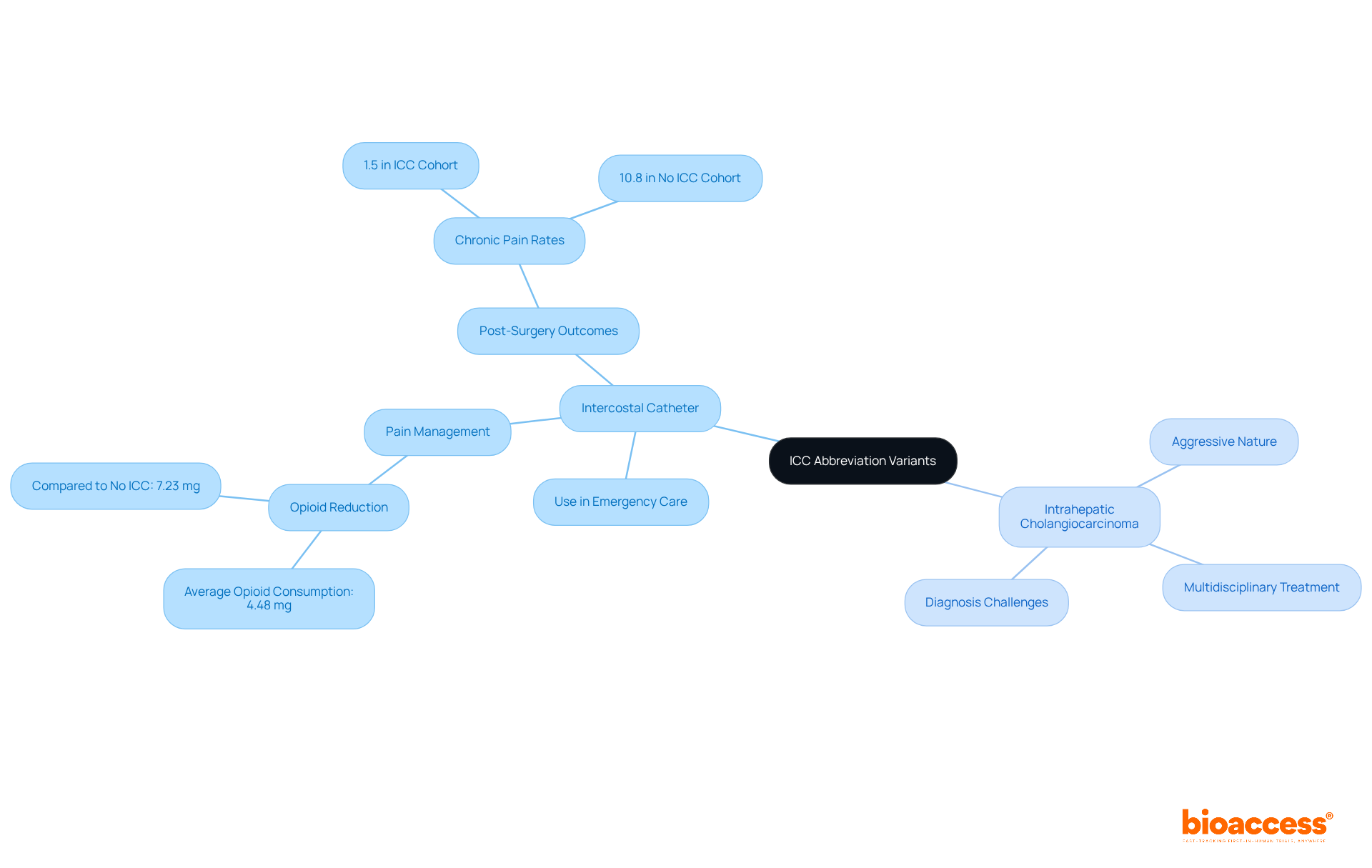
Intercostal Catheter (ICC) serves as a crucial medical device designed to drain fluid or air from the pleural space within the thoracic cavity, greatly facilitating postoperative recovery. Recent studies reveal that individuals utilizing intercostal catheters experience a substantial reduction in opioid consumption, averaging 4.48 mg compared to 7.23 mg in those without catheters. Furthermore, one year post-surgery, only 1.5% of individuals with ICC reported significant pain, in contrast to 10.8% in those lacking this intervention, as indicated by a study analyzing the effectiveness of intercostal catheters combined with a single shot intraoperative intercostal nerve block (SSINB). This advancement in pain management is particularly pertinent as the healthcare community strives to discover effective strategies that enhance recovery outcomes.
Intrahepatic Cholangiocarcinoma (ICC) represents a rare form of liver cancer that originates in the bile ducts within the liver. Projections for 2025 estimate approximately 42,240 new cases of liver and intrahepatic bile duct cancer in the U.S., underscoring the critical need for early detection and treatment strategies. The 5-year relative survival rate for liver and intrahepatic bile duct cancer stands at a mere 22.0%, highlighting the necessity for timely intervention.
The ICC abbreviation medical stands for Integrated Comprehensive Care, which refers to a holistic model that integrates hospital and community services, ensuring extensive support for individuals. Understanding these definitions is essential for healthcare professionals and patients alike, as they navigate the complexities of terminology and its implications for treatment and assistance.

The icc abbreviation medical carries substantial significance in medical terminology, representing critical concepts that enhance individual well-being and advance clinical research. Intrahepatic Cholangiocarcinoma (ICC) is increasingly recognized due to its rising incidence, which underscores the urgent need for effective treatment strategies. This cancer type, affecting the bile ducts within the liver, presents unique management challenges, particularly as disparities in access to care remain prevalent among different populations. Notably, the occurrence rate of intrahepatic cholangiocarcinoma is disproportionately higher among Hispanic individuals, highlighting the imperative for targeted interventions.
Furthermore, the Intercostal Catheter plays a pivotal role in managing respiratory conditions by providing essential drainage and facilitating improved lung function. Case studies demonstrate its efficacy, with the group identified by the ICC abbreviation medical exhibiting a significantly reduced rate of 60-day emergency department visits at 9.8% compared to 28.4% in controls, thereby decreasing complications and enhancing recovery times for individuals with pleural effusions and other respiratory issues.
Moreover, models referred to by the ICC abbreviation medical are crucial for optimizing transitions from hospital to home, significantly improving post-discharge outcomes. These models focus on coordinated care, ensuring that individuals receive the necessary support and resources to effectively manage their health after leaving the hospital. For instance, the ICC cohort experienced a lower readmission rate of 6.9% compared to 8.6% in controls, along with a reduced postoperative length of stay of 4 days versus 5 days.
Collectively, these applications of the ICC abbreviation medical underscore its vital role in advancing healthcare delivery and enhancing patient outcomes across various healthcare domains.
The origins of the term ICC abbreviation medical can be traced back to the mid-20th century, particularly with the identification of Intrahepatic Cholangiocarcinoma as a distinct clinical entity. This marked a pivotal moment in medical research, as the understanding of this cancer type evolved, leading to improved diagnostic and treatment protocols. Concurrently, the application of Intercostal Catheters became more widespread, reflecting advancements in thoracic surgery and intensive treatment. Furthermore, the concept of Integrated Comprehensive Support has gained traction in recent decades, highlighting a shift towards patient-centered models that emphasize continuity and coordination across healthcare environments. This historical perspective underscores the dynamic nature of healthcare terminology, such as the icc abbreviation medical, and its adaptation to meet the needs of evolving practices.

The Intercostal Catheter (ICC), often referred to by the icc abbreviation medical, serves as an essential instrument within medical practice, particularly in emergency and critical care environments. Its innovative design facilitates the effective drainage of pleural effusions and pneumothorax, both of which are crucial for patient recovery. Research indicates that patients utilizing ICCs experience a marked reduction in opioid consumption, averaging 4.48 mg compared to 7.23 mg in those without ICCs. This underscores its pivotal role in pain management and recovery. Furthermore, the positioning of ICCs correlates with reduced rates of chronic post-surgery pain (CPSP), with only 1.5% of individuals in the ICC cohort reporting pain one year post-surgery, in stark contrast to 10.8% in the non-ICC group. Such findings highlight the critical importance of ICCs in enhancing health outcomes.
Conversely, Intrahepatic Cholangiocarcinoma (ICC) introduces a distinct array of challenges, characterized by its aggressive nature and the complexities surrounding diagnosis and treatment. Patients diagnosed with ICC frequently necessitate multidisciplinary approaches to effectively navigate their treatment. The seamless integration of services and transitions of support are imperative in addressing the needs of these individuals, emphasizing the necessity of comprehensive support strategies.
In summary, grasping the varied applications and functionalities of the ICC abbreviation medical—whether relating to Intercostal Catheters or Intrahepatic Cholangiocarcinoma—is vital for healthcare professionals. Each variant significantly contributes to the enhancement of patient care and outcomes, reinforcing the need for precision in medical terminology.
Understanding the ICC abbreviation in medical terminology reveals its multifaceted nature, encompassing vital concepts essential for enhancing patient care and clinical outcomes. The significance of terms like Intercostal Catheter, Intrahepatic Cholangiocarcinoma, and Integrated Comprehensive Care cannot be overstated; each contributes uniquely to the healthcare landscape, addressing critical needs in pain management, cancer treatment, and coordinated care.
Throughout this article, we have explored key insights, including the effectiveness of Intercostal Catheters in reducing postoperative pain and complications, the urgent need for early detection and treatment strategies for Intrahepatic Cholangiocarcinoma, and the importance of Integrated Comprehensive Care models in ensuring seamless transitions from hospital to home. These elements underscore the necessity for healthcare professionals to engage with and understand the implications of the ICC abbreviation in their practice.
Ultimately, recognizing the diverse applications of the ICC abbreviation is crucial for improving healthcare delivery. As the medical community continues to evolve, embracing precise terminology and fostering effective communication will play a pivotal role in advancing patient outcomes. Engaging with these concepts not only enhances understanding but also emphasizes the importance of coordinated care strategies in addressing the complexities of modern healthcare challenges.
What does the abbreviation ICC stand for in medical terms?
ICC can refer to several significant healthcare terms, including Intercostal Catheter, Intrahepatic Cholangiocarcinoma, and Integrated Comprehensive Care.
What is an Intercostal Catheter (ICC)?
An Intercostal Catheter is a medical device designed to drain fluid or air from the pleural space within the thoracic cavity, which aids in postoperative recovery.
How does the use of Intercostal Catheters affect opioid consumption?
Individuals using intercostal catheters experience a substantial reduction in opioid consumption, averaging 4.48 mg compared to 7.23 mg in those without catheters.
What are the pain management outcomes for patients with Intercostal Catheters after surgery?
One year post-surgery, only 1.5% of individuals with Intercostal Catheters reported significant pain, compared to 10.8% in those lacking this intervention.
What is Intrahepatic Cholangiocarcinoma (ICC)?
Intrahepatic Cholangiocarcinoma is a rare form of liver cancer that originates in the bile ducts within the liver.
What are the projections for liver and intrahepatic bile duct cancer cases in the U.S. for 2025?
It is estimated that there will be approximately 42,240 new cases of liver and intrahepatic bile duct cancer in the U.S. by 2025.
What is the 5-year relative survival rate for liver and intrahepatic bile duct cancer?
The 5-year relative survival rate for liver and intrahepatic bile duct cancer is only 22.0%.
What does Integrated Comprehensive Care (ICC) refer to?
Integrated Comprehensive Care refers to a holistic model that integrates hospital and community services, providing extensive support for individuals.