


The article titled "10 New Treatments for CKD in 2024: Innovations You Need to Know" presents a compelling overview of the advancements in treatments for chronic kidney disease (CKD) anticipated to emerge in 2024. This exploration is crucial for clinical research, as it highlights innovative approaches such as sodium-glucose cotransporter-2 inhibitors and point-of-care testing. These advancements are poised to significantly enhance patient outcomes through improved management strategies and personalized care.
As we delve into the Medtech landscape, it becomes evident that these innovations address key challenges faced by healthcare providers. The integration of cutting-edge treatments not only improves patient care but also streamlines clinical processes, making it essential for professionals in the field to stay informed. How can these new strategies reshape your approach to CKD management?
In conclusion, the importance of collaboration among researchers, clinicians, and Medtech innovators cannot be overstated. By embracing these advancements, we can collectively improve the quality of care for CKD patients. The next steps involve actively engaging with these innovations and considering their implementation in clinical practice.
As the landscape of chronic kidney disease (CKD) management evolves, 2024 is set to unveil a range of innovative treatments that could redefine patient care. With advances spanning groundbreaking medications and cutting-edge diagnostic tools, these developments have the potential to significantly enhance patient outcomes and quality of life. Yet, amidst this wave of innovation, critical questions emerge:
This article delves into ten transformative treatments poised to make an impact in the coming year, offering insights into their mechanisms, benefits, and the future of CKD management.
bioaccess® stands out as a leading CRO in Latin America, dedicated to accelerating clinical research services for chronic renal disease (CKD) solutions. With a deep understanding of regulatory landscapes across Latin America, the Balkans, and Australia, bioaccess® achieves ethical approvals in an impressive 4-6 weeks and activates clinical research sites in under 8 weeks. This swift process not only reduces the time to market for the new treatment for CKD 2024 but also significantly improves patient access to groundbreaking therapies. Their commitment to early-phase studies guarantees that promising CKD interventions are assessed with efficiency and precision.
In addition to their rapid timelines, bioaccess® provides a comprehensive suite of services, including:
This holistic approach streamlines the clinical trial process, ensuring compliance and ultimately accelerating the path to commercialization. By addressing key challenges in the Medtech landscape, bioaccess® positions itself as a vital partner for those looking to navigate the complexities of clinical research.
Collaboration is essential in this field, and bioaccess® is poised to lead the way. As the demand for innovative CKD therapies increases, particularly with the anticipated new treatment for CKD 2024, the importance of partnering with a knowledgeable CRO cannot be overstated. Engage with bioaccess® today to explore how their expertise can enhance your clinical research efforts.

Sodium-glucose cotransporter-2 (SGLT2) inhibitors represent a groundbreaking advancement in the treatment of chronic renal disease (CKD). These medications work by preventing glucose reabsorption in the kidneys, which not only enhances glycemic control but also alleviates renal workload, ultimately leading to improved organ function. Recent clinical trials have shown that SGLT2 inhibitors significantly slow CKD progression, with one study revealing a remarkable 41% reduction in the risk of major adverse renal events (MAKEs) compared to RAAS blockade. Furthermore, these medications are associated with a 48% decreased risk of progressing to CKD stage 5, indicated by a hazard ratio of 0.52, underscoring their potential to enhance patient outcomes.
The protective effects of SGLT2 inhibitors extend beyond glycemic control; they also offer cardiovascular benefits and lower the incidence of acute kidney injury (AKI). However, it is crucial to remain vigilant regarding potential adverse effects, particularly urinary tract infections (UTIs), which are the most commonly reported side effects. As the evidence supporting the use of SGLT2 inhibitors continues to expand, they are solidifying their role as a cornerstone in CKD management, which may contribute to the new treatment for CKD 2024, providing renewed hope for both patients and healthcare providers. This growing body of research not only emphasizes the importance of these treatments but also encourages further exploration and collaboration in the field.

Cystatin C is emerging as a pivotal biomarker for evaluating glomerular filtration rate (GFR) in patients with chronic kidney disease (CKD). Unlike creatinine, cystatin C levels are less influenced by muscle mass, making it a more reliable indicator of renal function. This reliability allows for earlier detection of renal dysfunction and more accurate monitoring of CKD progression in clinical settings. As research continues to validate its effectiveness, cystatin C is poised to become a standard in CKD diagnostics, ultimately enhancing personalized care strategies.

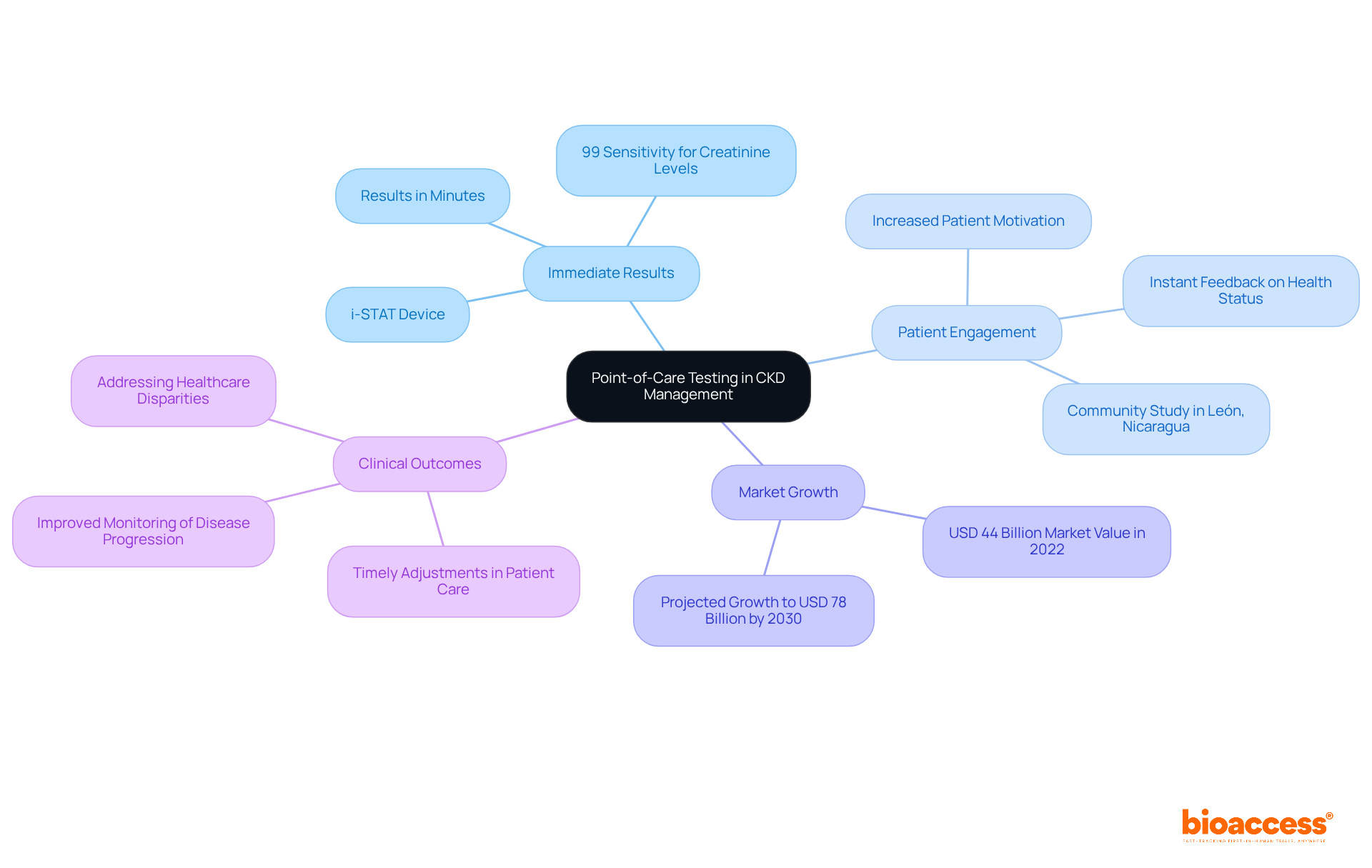
Point-of-care testing (POCT) is transforming the management of chronic kidney disease (CKD) by providing immediate results for essential biomarkers, such as creatinine and electrolytes. This rapid testing capability allows healthcare professionals to make timely adjustments, significantly enhancing outcomes for patients. For example, studies indicate that the i-STAT device can deliver results in just minutes, boasting a sensitivity of 99% for detecting creatinine levels of 1.5 mg/dL or higher. This enables clinicians to respond quickly to concerning clinical findings.
The integration of POCT into clinical practice not only facilitates better monitoring of disease progression but also promotes greater patient engagement, as individuals receive instant feedback on their health status. Furthermore, the convenience and efficiency of POCT represent a substantial advancement in managing chronic conditions. Evidence suggests that timely results lead to more informed care decisions and improved overall support for those with CKD. As Salvatore Viscomi, M.D., pointed out, the ongoing development of these technologies is vital for addressing healthcare disparities and ensuring early detection and intervention for CKD.
The POCT market was valued at approximately USD 44 billion in 2022 and is projected to reach USD 78 billion by 2030, highlighting the increasing importance of this technology in healthcare. With the rising prevalence of CKD, the introduction of a new treatment for CKD in 2024 highlights the ever-increasing critical role of POCT in enhancing care and optimizing management strategies. A community study in León, Nicaragua, underscores the importance of validating POC devices in community settings, demonstrating their effectiveness in improving outcomes for individuals.
Personal risk evaluation is essential in managing chronic kidney disease (CKD), enabling healthcare professionals to customize care based on each individual's unique profile. Factors such as age, comorbidities, and genetic predispositions play a significant role in influencing treatment outcomes. By employing advanced risk assessment tools like the Kidney Klinrisk Algorithm, clinicians can identify high-risk individuals and implement targeted interventions, leading to better management of CKD and improved outcomes.
As Maria Madak, an IgA Nephropathy patient and transplant recipient, aptly states, "For anyone who has kidney disease... have hope. Be alert, eat right, take your medications, and be persistent with your lab and doctor visits." This personalized approach is increasingly vital in modern medicine, aligning care strategies with the distinct needs of individuals and fostering a more effective healthcare experience.
Moreover, the success stories of individuals like Melissa Bensouda, who has thrived for over twenty years post-diagnosis, highlight the transformative potential of personalized therapies. By integrating community support and resources, healthcare providers can develop a comprehensive care model that not only addresses medical needs but also empowers individuals to lead fulfilling lives.

Postponing the advancement of chronic renal disease (CKD) is crucial for improving patient outcomes. Effective management plans typically include several key strategies:
For instance, keeping blood pressure below 130/80 mmHg is vital, as hypertension significantly contributes to CKD progression. Additionally, dietary changes, like reducing sodium intake to less than 2.3 g/day, can effectively lower blood pressure and decrease proteinuria, thereby slowing disease advancement. The World Health Organization endorses this sodium limit as a cost-effective public health measure.
Medications such as ACE inhibitors and SGLT2 inhibitors have proven effective in delaying CKD progression. These therapies not only help manage blood pressure but also provide renal protective benefits, making them essential components of a comprehensive management strategy. Regular monitoring of renal function, including estimated glomerular filtration rate (eGFR) and albuminuria levels, is critical for assessing treatment effectiveness and adjusting strategies as needed.
Patient education is pivotal in management, empowering individuals to embrace healthier lifestyles. Research shows that lifestyle modifications, including increased physical activity and weight management, can significantly enhance quality of life and lower the risk of CKD progression. As Akihiro Kuma noted, "Lifestyle interventions seem to positively affect some risk factors for progression of CKD and quality of life." For example, a systematic review revealed that lifestyle interventions led to significant improvements in key health markers, including creatinine levels and blood pressure.
By focusing on these multifaceted strategies, healthcare providers can enhance the quality of life for individuals with CKD and alleviate the burden of the disease, ultimately leading to better long-term outcomes. Notably, chronic renal disease affects 10% of adults globally, with its prevalence rising by 88% from 1990 to 2016, underscoring the urgent need for effective management strategies.

Hyperuricemia, characterized by elevated uric acid levels, is a prevalent complication in individuals with chronic renal disease (CKD). This condition not only exacerbates renal damage but also heightens cardiovascular risk. Effective management strategies are essential, including:
Research shows that allopurinol can significantly lower serum uric acid levels, achieving therapeutic effectiveness in about 45.4% of those treated. Furthermore, individuals with mean serum uric acid levels above 8.0 mg/dL face a greater likelihood of treatment failure compared to those with levels below 6.0 mg/dL. This underscores the critical need for consistent monitoring of uric acid concentrations. By addressing hyperuricemia, healthcare providers can enhance renal health and improve overall well-being, emphasizing the importance of a comprehensive approach to CKD management with the new treatment for CKD 2024.

Statins are frequently recommended for individuals with chronic kidney disease (CKD) to effectively manage dyslipidemia and mitigate cardiovascular risk. Research indicates that statin therapy can significantly reduce the occurrence of cardiovascular events in this population, which is crucial given the heightened risk of heart disease among those with CKD. For instance, studies reveal that statin therapy is associated with a 23% decrease in all-cause mortality among hyperlipidemic individuals undergoing dialysis who have a history of myocardial infarction or percutaneous coronary intervention, underscoring its potential benefits.
However, initiating statin therapy requires careful customization based on individual factors, including kidney function and the risk of side effects such as muscle cramping, tenderness, and weakness, as well as liver enzyme elevation. Current guidelines advocate for statins in individuals with CKD over 50 years old who are not on dialysis, while younger individuals aged 18-49 may be considered if they exhibit specific risk factors. Furthermore, the KDIGO guidelines emphasize a 'fire and forget' approach when starting statin therapy in individuals with CKD.
Ongoing research continues to investigate the long-term cardiovascular benefits of statins in CKD management, making this a vital area for healthcare providers to monitor and address. It is essential for healthcare providers to engage in discussions about the risks and benefits of statin therapy with their patients, ensuring informed decision-making.

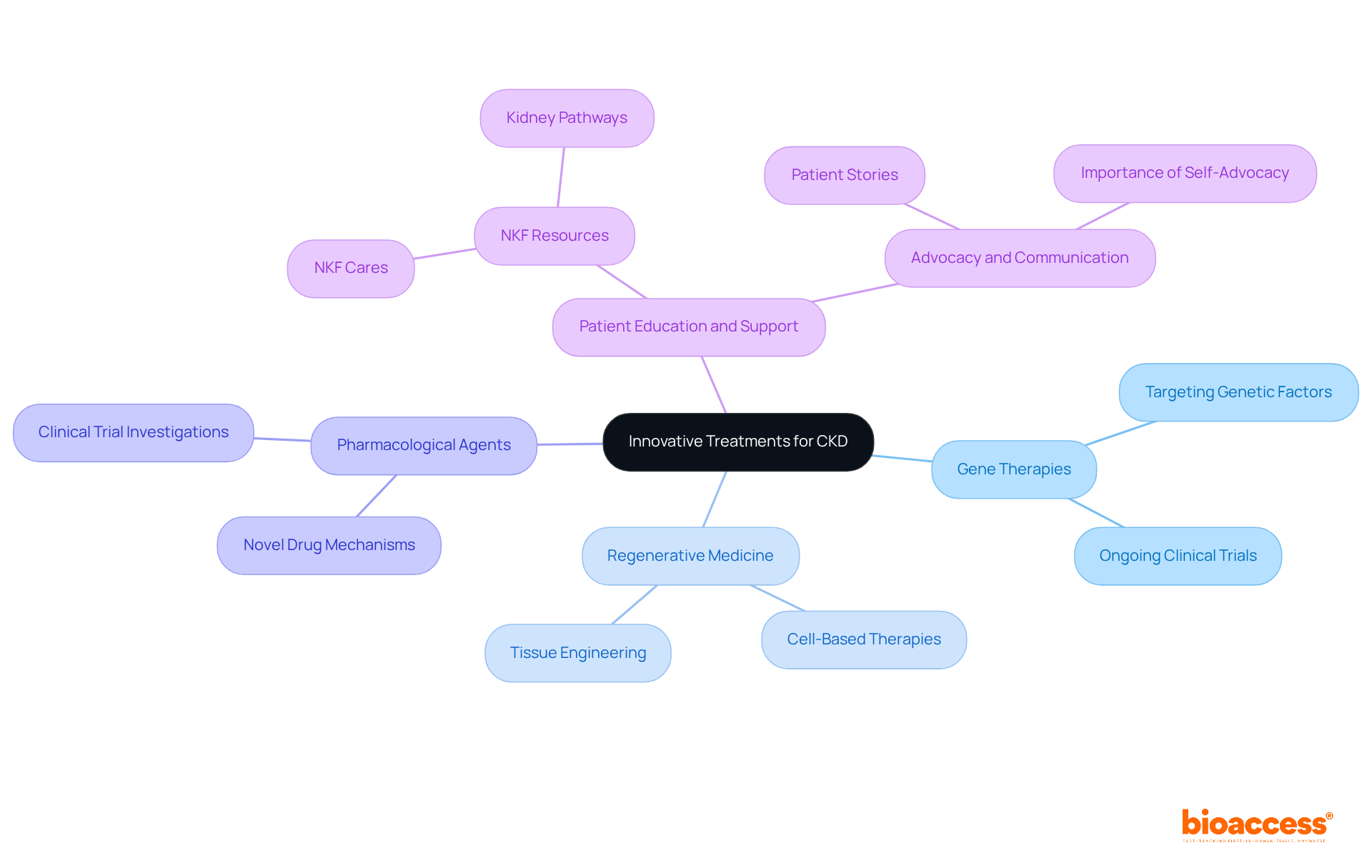
Innovative experimental treatments are emerging for chronic kidney disease (CKD), including a new treatment for CKD 2024, driven by extensive research into gene therapies, regenerative medicine, and novel pharmacological agents that specifically target pathways of kidney damage. Ongoing clinical trials are investigating these therapies as a new treatment for CKD 2024, which hold the potential to transform CKD management and instill renewed optimism in affected individuals.
For instance, gene therapies are currently being tested in clinical trials, aiming to tackle the underlying genetic factors that contribute to CKD progression. As these advancements unfold, it is essential for healthcare providers to stay updated on the latest research and innovations, particularly the new treatment for CKD 2024, ensuring they can deliver the most effective care to those grappling with this challenging condition.
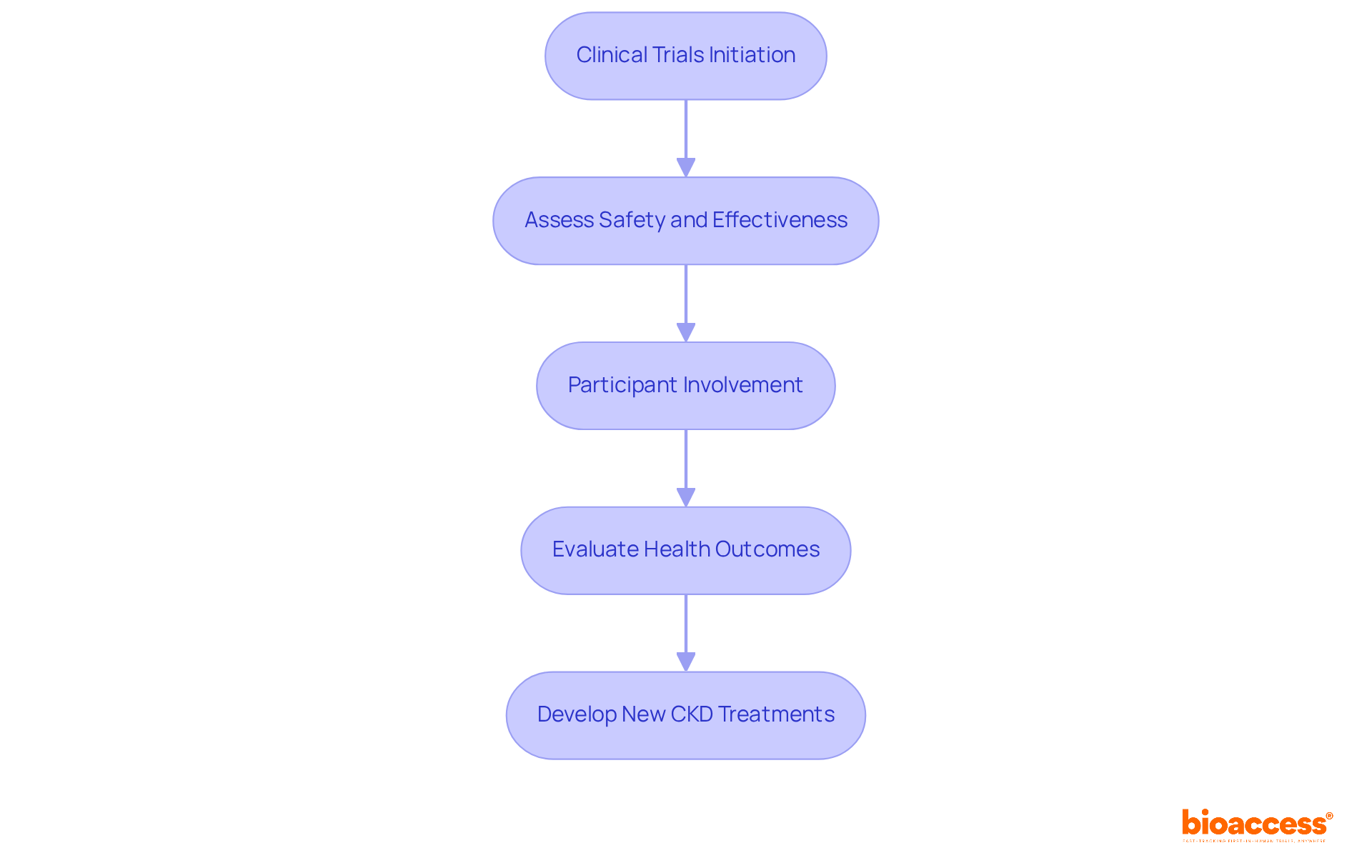
Clinical trials serve as the cornerstone for developing a new treatment for CKD 2024, providing a systematic approach to assess safety and effectiveness. These studies not only enhance scientific understanding but also grant individuals access to pioneering therapies. For example, recent trials have shown that participation can lead to better health outcomes, with some reporting a 25% reduction in cardiovascular and renal complications among participants. By engaging in clinical trials, individuals play a crucial role in CKD research while potentially accessing a new treatment for CKD 2024 that may not yet be available commercially.
The rigorous methodologies employed in these trials ensure that the new treatment for CKD 2024 meets the highest standards of safety and effectiveness, ultimately leading to improved care for patients. As the prevalence of CKD continues to escalate, driven by factors such as an aging population and rising rates of type 2 diabetes, the necessity for robust clinical trials becomes increasingly urgent. Recent initiatives, including the MoreTrials campaign, aim to streamline trial participation while prioritizing participant safety and reliable outcomes, thereby encouraging greater patient involvement in this essential area of research.
The advancements in chronic kidney disease (CKD) treatments highlighted in this article mark a pivotal shift towards more effective management strategies and innovative therapies for 2024. Collaborations with organizations like bioaccess®, the role of SGLT2 inhibitors, and the emergence of biomarkers such as cystatin C illustrate the rapidly evolving landscape of CKD care. These innovations promise not only to enhance patient outcomes but also signify a collective effort to tackle the complexities of CKD management.
Key insights reveal that strategies such as point-of-care testing, personalized risk assessments, and comprehensive lifestyle modifications are essential in delaying CKD progression. The exploration of new experimental treatments and the ongoing commitment to clinical trials further demonstrate a proactive approach in the fight against this prevalent condition. Each of these elements contributes to a nuanced understanding of CKD, enabling healthcare providers to tailor interventions that align with individual patient needs.
The significance of these developments cannot be overstated. As the prevalence of CKD continues to rise, it is crucial for healthcare professionals, patients, and stakeholders to stay informed and engaged with the latest advancements. Embracing these innovations fosters improved health outcomes and empowers individuals living with CKD to take charge of their health journey. The path forward is bright, and the commitment to research and collaboration will undoubtedly lead to a future where CKD management is more effective and accessible for all.
What is bioaccess and what services does it provide for CKD treatments?
Bioaccess is a leading Contract Research Organization (CRO) in Latin America that specializes in accelerating clinical research services for chronic renal disease (CKD) treatments. It offers a comprehensive suite of services, including subject recruitment and trial data management, aimed at streamlining the clinical trial process and ensuring compliance.
How quickly can bioaccess achieve ethical approvals and activate clinical research sites?
Bioaccess can achieve ethical approvals in an impressive 4-6 weeks and activate clinical research sites in under 8 weeks.
What are Sodium-Glucose Cotransporter-2 (SGLT2) inhibitors, and how do they help in CKD management?
SGLT2 inhibitors are medications that prevent glucose reabsorption in the kidneys, enhancing glycemic control and alleviating renal workload. They have been shown to significantly slow CKD progression and reduce the risk of major adverse renal events and progression to CKD stage 5.
What are the benefits of SGLT2 inhibitors beyond glycemic control?
In addition to improving glycemic control, SGLT2 inhibitors offer cardiovascular benefits and lower the incidence of acute kidney injury (AKI).
What is Cystatin C, and why is it important in assessing renal function in CKD patients?
Cystatin C is a biomarker that is used to evaluate glomerular filtration rate (GFR) in CKD patients. It is less influenced by muscle mass compared to creatinine, making it a more reliable indicator of renal function, which allows for earlier detection of renal dysfunction and more accurate monitoring of CKD progression.
How is Cystatin C expected to impact CKD diagnostics?
As research continues to validate its effectiveness, Cystatin C is poised to become a standard in CKD diagnostics, enhancing personalized care strategies for patients.