


Understanding the complexities of clinical trials in the biopharmaceutical sector is crucial, especially in Australia, where innovation and patient safety take center stage. Risk-based monitoring (RBM) models stand out as essential frameworks that not only identify and mitigate potential risks but also enhance the overall quality of clinical studies. As the biopharma landscape evolves, professionals must consider:
This article explores the core principles, strategic approaches, and technological advancements that can transform risk-based monitoring practices, ultimately leading to improved patient safety and study efficiency.
Risk-based monitoring (RBM) stands as a pivotal framework designed to identify, assess, and mitigate risks throughout the clinical study lifecycle. For biopharma professionals aiming to enhance study outcomes and ensure patient safety, understanding risk-based monitoring models in Australian biopharma is essential.
Risk Identification and Assessment is the first step in this strategic approach. Before initiating any experiment, it’s vital to pinpoint potential hazards that could compromise data integrity and patient safety. This involves a thorough evaluation of the study design, patient demographics, and operational complexities. Recent studies suggest that effective risk assessments should ideally begin prior to protocol development, maximizing their overall value.
Next, we have the Prioritization of Monitoring Activities. Not every data point requires the same level of scrutiny. The focus of risk-based monitoring models in Australian biopharma is on critical data that directly influences patient safety and study outcomes. This targeted approach not only enhances resource allocation but can also significantly reduce clinical study costs, as frequent onsite visits can account for up to 30% of total expenses.
The third principle is Continuous Risk Evaluation. Ongoing assessment of identified risks is crucial throughout the study. This adaptive strategy allows teams to modify monitoring efforts based on real-time data and emerging challenges, ensuring that potential issues are swiftly addressed. The adoption of Risk-Based Quality Management (RBQM) components has surged, with 88% of studies incorporating at least one RBQM element by 2021.
Finally, Collaboration and Communication are key to effective RBM. Strong communication among all stakeholders-sponsors, research associates (CRAs), and site personnel-is essential. This collaboration fosters alignment on risk management strategies and facilitates rapid responses to any issues that may arise. A recent survey revealed that 81% of research sites utilizing RBQM statistical data oversight experienced improvements in quality, underscoring the importance of effective teamwork.
By grasping these fundamental principles, biopharma professionals can more effectively implement risk-based monitoring models in Australian biopharma, leading to enhanced study outcomes and improved patient safety.

To effectively implement risk-based monitoring models in Australian biopharma during clinical trials, adopting a strategic approach is crucial. Here are several key strategies that can enhance your oversight efforts:
Develop a Comprehensive Monitoring Plan: A robust monitoring plan should clearly outline identified risks, necessary monitoring activities, and the roles and responsibilities of team members. This plan serves as a roadmap for the entire process, ensuring all aspects are addressed.
Employ Key Risk Indicators (KRIs): Establish quantifiable KRIs that provide essential metrics throughout the study. These indicators are vital for assessing the study's health and identifying areas that may need closer scrutiny, transforming abstract risk concepts into actionable insights.
Incorporate Centralized Oversight: Utilize centralized oversight techniques to analyze data from multiple sites in real-time. This method aids in the swift recognition of trends and potential issues, allowing for proactive management and enhancing overall efficiency.
Foster a Culture of Compliance: It’s essential for all team members to understand the importance of adhering to oversight protocols. Regular training sessions and updates on regulatory requirements can help maintain high standards of practice and ensure compliance across the board.
Engage Stakeholders Early: Involve all relevant stakeholders, including regulatory bodies and ethics committees, early in the planning process. Their insights can significantly influence the oversight strategy and ensure alignment with regulatory expectations, ultimately leading to smoother execution of the study.
By implementing these strategies, biopharma companies can improve their risk-based monitoring models in Australian biopharma, leading to more effective studies and enhanced patient safety. The implementation of risk-oriented oversight has shown promising success rates, with a notable increase in the number of studies adopting these practices, indicating a shift towards more proactive and data-informed strategies in medical research.

Integrating technology and analytics into risk-based monitoring models in Australian biopharma is crucial for enhancing the efficiency of clinical studies. By leveraging these tools, organizations can significantly improve their oversight capabilities, leading to substantial cost reductions and enhanced operational effectiveness in research studies.
Implement Electronic Information Capture (EDC) Systems: EDC systems streamline information collection and management, providing real-time access to trial data. This capability enables faster decision-making and improves information accuracy, with organizations achieving error rates as low as 0.04% compared to conventional manual methods, which average around 1%. Such a significant improvement underscores the value of EDC systems in clinical research.
Utilize Advanced Analytics: Employing data analytics tools allows for the identification of trends and anomalies in experimental data. Predictive analytics can forecast potential risks, enabling proactive interventions before issues escalate. For instance, machine learning models can analyze large datasets to uncover hidden trends, optimizing trial design and improving overall efficiency.
Adopt Remote Monitoring Technologies: Remote monitoring solutions minimize the need for frequent site visits, allowing for a more efficient use of resources. Technologies like telemedicine and mobile health applications enhance patient involvement and information gathering, enabling treatment-naive cardiology or neurology groups to be enrolled 50% quicker than conventional sites, as demonstrated by bioaccess®. This acceleration not only enhances patient recruitment but also contributes to significant cost savings of up to $25K per patient with FDA-ready data.
Integrate Risk-Based Oversight Software: Specialized software designed for risk-based oversight can automate risk assessments and oversight activities. This software helps track Key Risk Indicators (KRIs) and generates reports that inform decision-making, ensuring that monitoring efforts are focused on high-risk areas.
Enhance Information Visualization: Utilizing visualization tools presents intricate information in a readily understandable format. Visual dashboards assist stakeholders in swiftly grasping progress and pinpointing areas requiring attention, ultimately resulting in enhanced data quality and outcomes.
By adopting these technologies, biopharma firms can significantly enhance their oversight capabilities through risk-based monitoring models in Australian biopharma. Additionally, bioaccess® offers comprehensive clinical trial management services, including Early-Feasibility, First-In-Human, Pilot, Pivotal, and Post-Market Follow-Up Studies, ensuring successful outcomes for your clinical research initiatives.

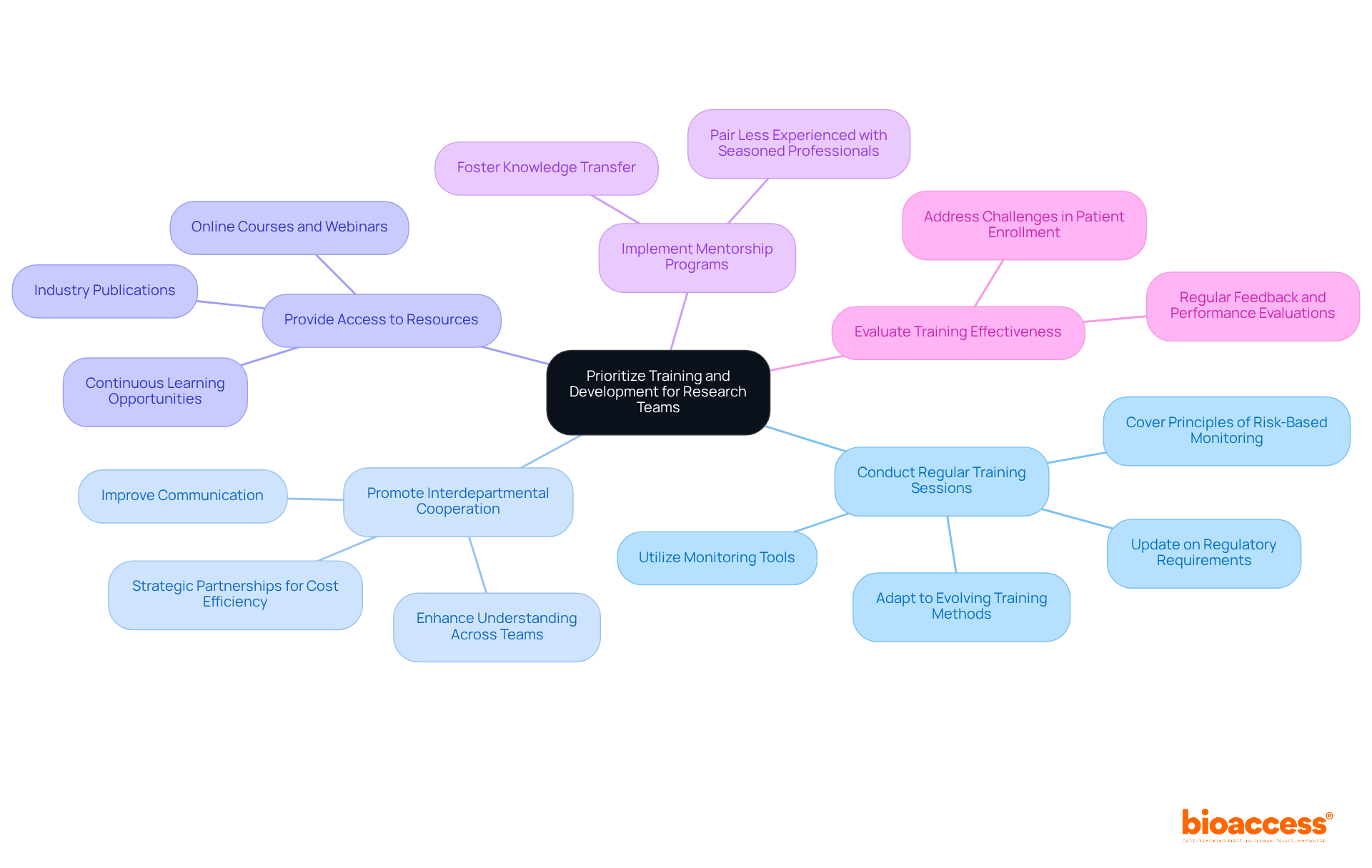
To ensure the successful execution of risk-based oversight, prioritizing training and development for research teams is essential. This focus not only enhances team capabilities but also aligns with the evolving demands of clinical research. Consider the following approaches:
Conduct Regular Training Sessions: Organize training sessions that cover the principles of risk-based monitoring, regulatory requirements, and the use of monitoring tools. This ensures that all team members are up-to-date with the latest practices and can adapt to the evolving nature of training delivery methods, including online platforms and blended learning.
Promote Interdepartmental Cooperation: Cultivating collaboration among various divisions, such as operational activities, data management, and regulatory affairs, is crucial. This interdisciplinary approach enhances understanding and improves communication across teams. Strategic partnerships can also improve cost efficiency and accelerate the research process, further enhancing collaboration.
Provide Access to Resources: Offering access to online courses, webinars, and industry publications that focus on risk-based monitoring and study management is vital. Continuous learning opportunities are essential, as evidenced by the statistic that 51% of U.S. workers reported taking a class or receiving additional training within 12 months as of December 2024. This helps team members stay informed about industry trends and best practices.
Implement Mentorship Programs: Pairing less experienced team members with seasoned professionals who can provide guidance and support fosters knowledge transfer. Mentorship helps build a strong foundation for future leaders in clinical research.
Evaluate Training Effectiveness: Regularly assessing the effectiveness of training programs through feedback and performance evaluations allows for continuous improvement. Given that 85% of studies struggle to enroll enough patients on time, effective training and collaboration are critical for enhancing study outcomes.
By prioritizing training and development, biopharma companies can cultivate a skilled workforce capable of effectively implementing risk-based monitoring strategies. This ultimately leads to better trial outcomes.
Mastering risk-based monitoring models is crucial for biopharma professionals in Australia. These frameworks significantly enhance study outcomes and ensure patient safety. By effectively implementing these models, organizations can navigate the complexities of clinical trials, minimizing risks while optimizing resources.
The article outlines four core principles of risk-based monitoring:
Each principle acts as a building block for a robust risk-based monitoring strategy, allowing biopharma companies to focus on critical data and adapt to emerging challenges throughout the clinical study lifecycle.
In conclusion, integrating technology, data analytics, and comprehensive training programs is vital for successfully implementing risk-based monitoring in Australian biopharma. By fostering a culture of compliance and collaboration, organizations can significantly enhance their oversight capabilities. This ultimately leads to more effective studies and improved patient safety. Embracing these strategies not only prepares biopharma teams for the evolving landscape of clinical research but also positions them to achieve better trial outcomes in the competitive biopharmaceutical industry.
What is risk-based monitoring (RBM)?
Risk-based monitoring (RBM) is a framework designed to identify, assess, and mitigate risks throughout the clinical study lifecycle, particularly in biopharma.
Why is understanding RBM important for biopharma professionals?
Understanding RBM is essential for enhancing study outcomes and ensuring patient safety in clinical trials.
What is the first step in risk-based monitoring?
The first step is Risk Identification and Assessment, which involves pinpointing potential hazards that could compromise data integrity and patient safety before initiating any experiment.
When should risk assessments ideally begin?
Effective risk assessments should ideally begin prior to protocol development to maximize their overall value.
How does prioritization of monitoring activities work in RBM?
Not every data point requires the same level of scrutiny; RBM focuses on critical data that directly influences patient safety and study outcomes, enhancing resource allocation and reducing clinical study costs.
What percentage of total expenses can frequent onsite visits account for in clinical studies?
Frequent onsite visits can account for up to 30% of total expenses in clinical studies.
What is the importance of continuous risk evaluation in RBM?
Continuous risk evaluation involves ongoing assessment of identified risks throughout the study, allowing teams to adapt monitoring efforts based on real-time data and emerging challenges.
What is the trend regarding Risk-Based Quality Management (RBQM) in studies?
By 2021, 88% of studies incorporated at least one RBQM element, indicating a surge in its adoption.
Why are collaboration and communication important in RBM?
Strong communication among stakeholders, including sponsors, research associates, and site personnel, is essential for aligning on risk management strategies and facilitating rapid responses to issues.
What improvement was noted in research sites utilizing RBQM statistical data oversight?
A survey revealed that 81% of research sites utilizing RBQM experienced improvements in quality, highlighting the importance of effective teamwork in risk management.