


The article emphasizes the transformative impact of advanced imaging techniques in clinical research, underscoring their critical role in enhancing diagnostic capabilities and improving patient care. By exploring various innovative imaging technologies, including:
the article demonstrates how these advancements significantly enhance diagnostic accuracy. Furthermore, these technologies expedite medical studies, ultimately leading to improved health outcomes for patients. The relevance of these developments in the Medtech landscape cannot be overstated, as they address key challenges in clinical research, paving the way for future advancements.
The landscape of clinical research is experiencing a seismic shift, propelled by the rapid evolution of advanced imaging techniques that promise to enhance diagnostic precision and patient care. As healthcare professionals strive to keep pace with these innovations, the implications for medical studies are profound—ranging from accelerated trial timelines to improved treatment outcomes. However, significant challenges accompany these advancements: How can the medical community effectively integrate these cutting-edge technologies while ensuring safety and efficacy? This exploration delves into ten transformative imaging techniques that are not only redefining clinical research but also addressing the pressing questions of modern medicine.
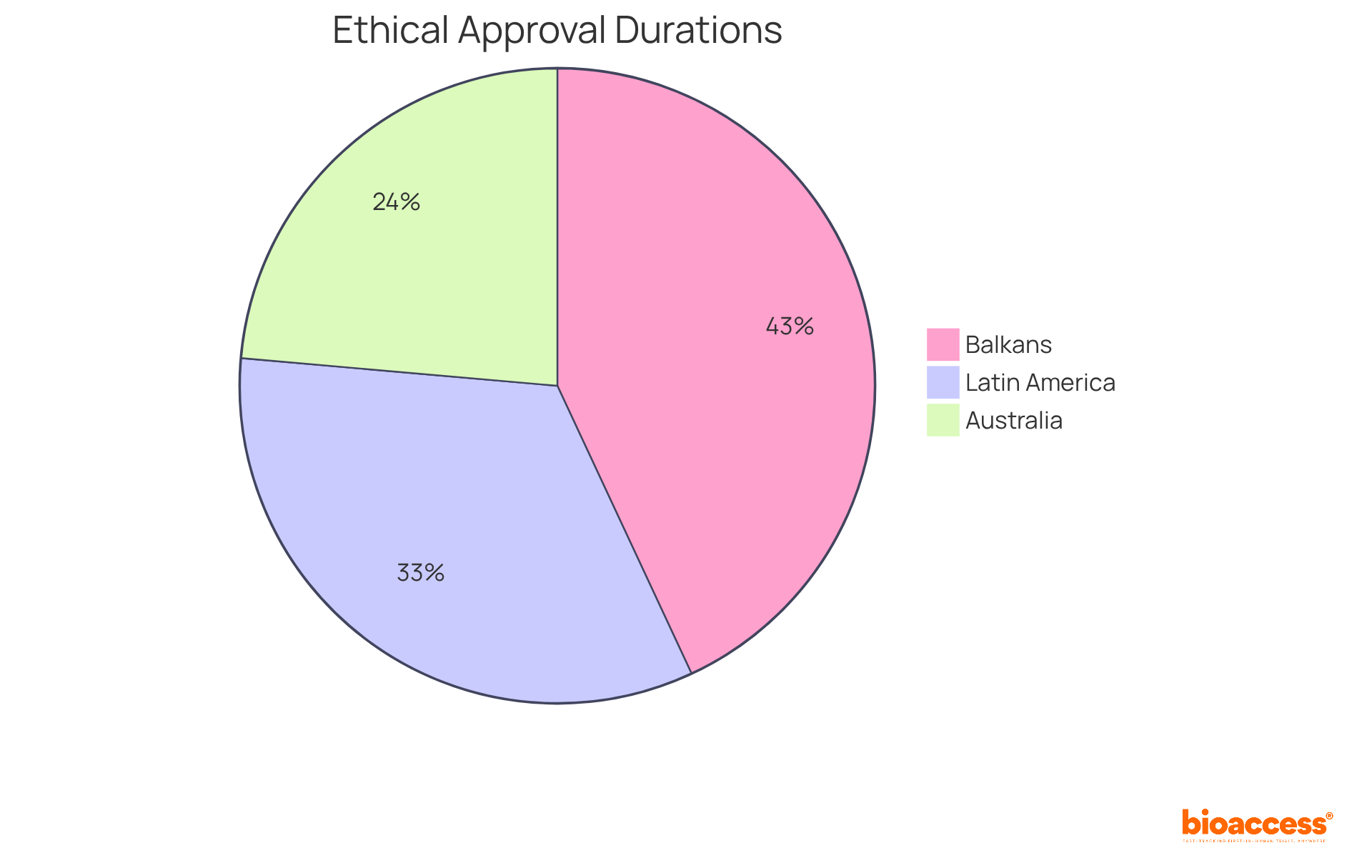
bioaccess® stands at the forefront of clinical research, particularly in advanced imaging techniques. By leveraging its strategic presence across Latin America, the Balkans, and Australia, bioaccess® accelerates the development and implementation of innovative visual technologies. The organization is committed to obtaining ethical approvals within an impressive timeframe of 4-6 weeks, significantly enhancing the pace of participant enrollment. This efficiency is crucial in a rapidly evolving field, where timely access to sophisticated imaging techniques can lead to substantial improvements in diagnostic capabilities and health outcomes.
In 2025, the average duration for ethical approvals varies by region, with Latin America showing a median of 48 days, underscoring the area's potential for swift advancements in healthcare. Medtech leaders emphasize that the utilization of imaging techniques not only expedites medical studies but also enhances the quality of data collected, ultimately benefiting patient care.
Through its innovative approach, bioaccess® is not only advancing the development of cutting-edge visualization technologies but is also establishing a standard for clinical research efficiency and effectiveness.
Ultrasound Shear Wave Elastography (SWE) represents a groundbreaking non-invasive imaging technique that is one of the advanced imaging techniques used to quantify tissue stiffness, providing essential insights into a range of medical conditions. By accurately measuring the elasticity of tissues, SWE significantly enhances tumor and liver disease characterization through imaging techniques, leading to more precise diagnoses and informed treatment planning.
Notably, recent studies demonstrate that SWE, among various imaging techniques, can effectively distinguish between benign and malignant lesions, achieving a remarkable sensitivity of 97% in identifying malignant focal liver lesions. Furthermore, increased stiffness values, which can be evaluated using imaging techniques, are frequently linked to malignancy risk, as evidenced by a hazard ratio of 2.57 for mortality from cardiovascular disease in individuals exhibiting elevated liver stiffness. This capability proves particularly advantageous in research environments, where a deeper understanding of tissue characteristics enhances patient categorization and outcomes.
The integration of imaging techniques, including SWE, into medical trials not only aids in evaluating new therapies but also contributes to the advancement of medical knowledge by providing real-time, quantitative assessments of tissue attributes. Dr. Wei Dong Gao emphasizes this, stating, 'Ultrasound Shear Wave Elastography offers a non-invasive option for tracking liver stiffness, which relates to fibrosis stages,' underscoring its critical role in medical decision-making.
However, it is crucial to recognize that SWE encounters technical limitations, such as operator dependency and variability in measurements, which can impact its reproducibility. Despite these challenges, the capacity of SWE to deliver objective measurements positions it as an invaluable tool for enhancing diagnostic accuracy and guiding clinical decision-making in oncology and hepatology, particularly with the use of imaging techniques.

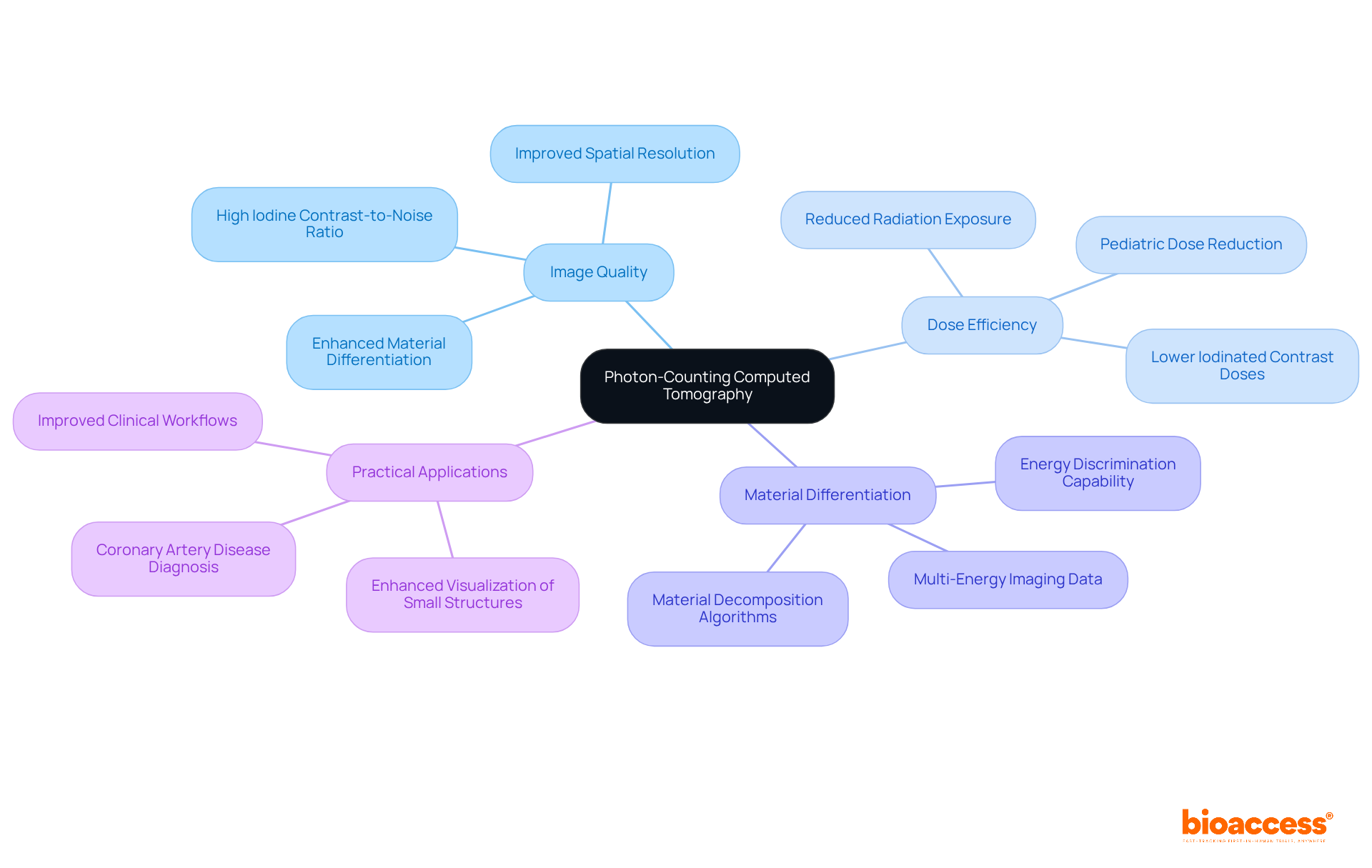
Photon-Counting Computed Tomography (PCCT) represents a pivotal advancement in imaging techniques, delivering superior image quality while significantly reducing radiation exposure. Unlike conventional CT systems that rely on energy-integrating detectors, PCCT employs imaging techniques to count individual photons, resulting in enhanced spatial resolution and improved material differentiation. This capability enhances diagnostic precision and emphasizes safety by reducing radiation exposure, with reductions of 20%-30% achievable in young individuals without compromising image quality, as demonstrated in recent studies.
Radiologists have noted that PCCT's high iodine contrast-to-noise ratio allows for lower doses of iodinated contrast, further enhancing safety for patients with renal dysfunction. In medical research, imaging techniques such as PCCT facilitate more accurate evaluations of disease progression and treatment responses, showcasing its essential value in developing groundbreaking healthcare solutions.
Successful implementations of PCCT, such as the Naeotom Alpha class, have proven effective in minimizing radiation exposure while maintaining high image quality, solidifying its role as a transformative tool in modern diagnostics through the use of advanced imaging techniques.
As Philipp Fischer, Head of Computed Tomography at Siemens Healthineers, stated, 'We observe how photon-counting CT influences medical decision-making, and we are convinced that this technology shapes the future of CT scanning.
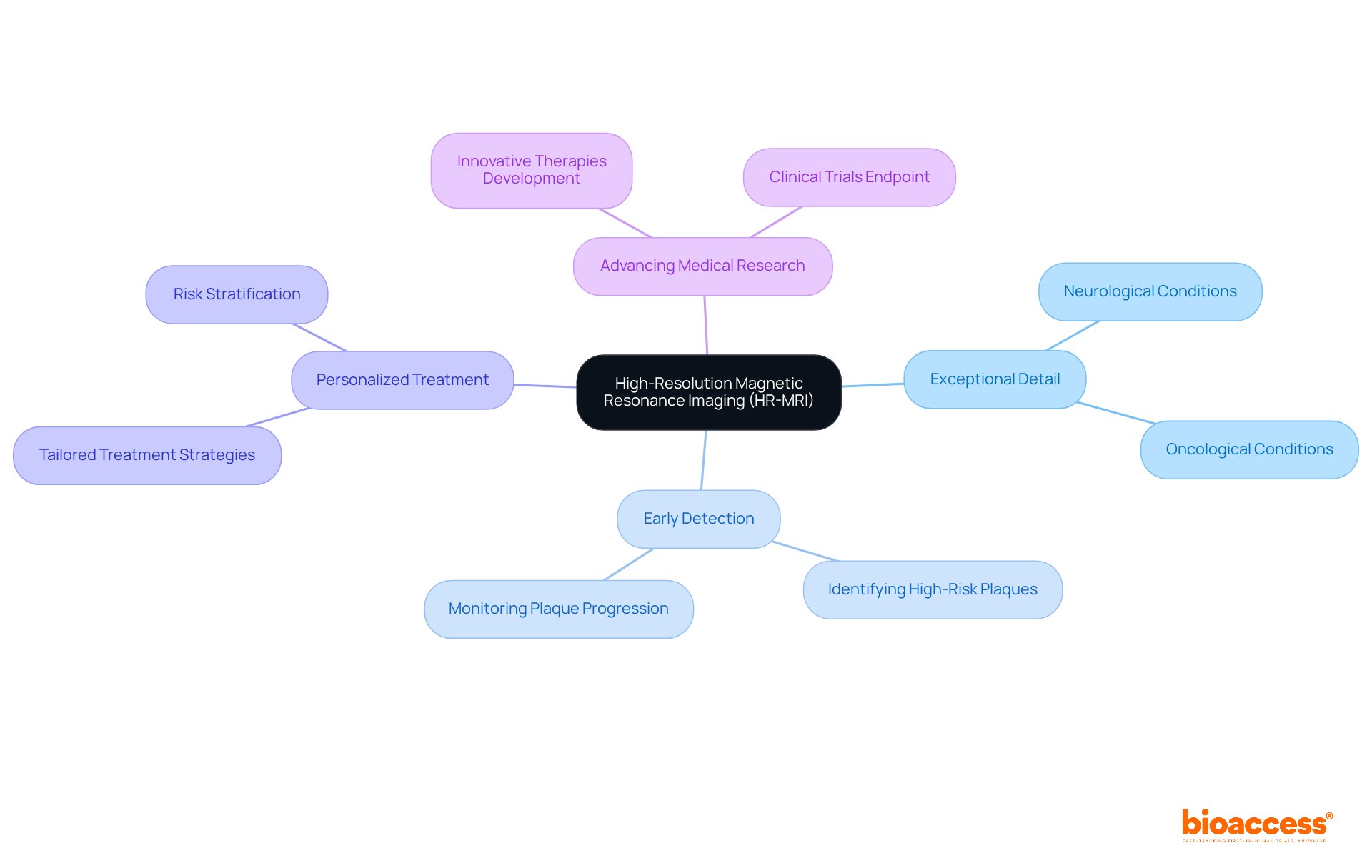
High-Resolution Magnetic Resonance Imaging (HR-MRI) has revolutionized imaging techniques by delivering exceptional detail in soft tissue visualization. This advancement is particularly advantageous in evaluating neurological and oncological conditions. In clinical studies, HR-MRI enables scientists to detect subtle changes in disease states, thereby fostering early intervention and personalized treatment strategies. The capacity to visualize anatomical structures with remarkable precision using imaging techniques not only enhances diagnostic accuracy but also facilitates the development of innovative therapies. Consequently, HR-MRI stands as an indispensable tool in propelling medical research forward.
Contrast-Enhanced Ultrasound (CEUS) represents a groundbreaking advancement in imaging techniques, significantly enhancing the visualization of vascular structures and blood flow dynamics. By utilizing microbubble contrast agents, CEUS facilitates real-time imaging that enhances the assessment of various medical conditions, including:
Recent medical trials have confirmed the efficacy of CEUS in evaluating therapeutic responses, offering critical insights into vascular changes following treatment. Its non-invasive nature, coupled with rapid acquisition times, establishes CEUS as an essential tool in medical studies, particularly for tumor evaluation and the exploration of new treatment methods using imaging techniques.
Vascular experts have noted that imaging techniques, such as CEUS, not only improve diagnostic accuracy but also enhance the management of patients by delivering detailed insights into vascular responses, thereby transforming the landscape of vascular visualization in clinical research.

Ultrafast Ultrasound represents a revolutionary advancement in imaging techniques, allowing for real-time observation at frame rates reaching up to 2000 frames per second. This rapid imaging techniques capability is crucial in emergency and critical care environments, where swift diagnosis using imaging techniques can significantly affect patient outcomes. By delivering immediate insights into anatomical structures and physiological processes, imaging techniques such as ultrafast ultrasound empower clinicians to make informed decisions quickly, thereby enhancing management strategies.
In practical applications, this technology proves indispensable for evaluating acute conditions, such as trauma or cardiac events, facilitating real-time assessment of interventions. Critical care physicians have noted that the ability to observe changes in a patient's condition instantaneously leads to more effective treatment strategies and improved clinical outcomes. For example, the incorporation of ultrafast ultrasound in emergency medicine has been demonstrated to support timely interventions, ultimately advancing both medical knowledge and patient care.
Current data indicates that ultrafast ultrasound, as one of the advanced imaging techniques, not only enhances diagnostic accuracy but also reduces the time required for visualization, establishing it as a vital tool in modern healthcare. As the global ultrasound market is projected to surpass USD 10.9 billion by 2030, driven by the growing demand for non-invasive diagnostic solutions, the significance of ultrafast ultrasound in clinical research and practice is poised for substantial expansion.

The incorporation of Artificial Intelligence (AI) in visual analysis is fundamentally transforming the field, significantly enhancing diagnostic precision and operational efficiency. AI algorithms possess the capability to analyze extensive volumes of data produced by imaging techniques, adeptly identifying patterns and anomalies that may elude human detection. This advanced analytical capability not only enhances diagnostic precision—demonstrated by an overall accuracy of 52.1% for generative AI models—but also optimizes workflows within medical settings.
In medical studies, AI facilitates the development of predictive models and assists in individual categorization, paving the way for more tailored treatment strategies. As Jean Jose, a prominent figure in radiology, aptly observes, "AI is something that is impacting every aspect of our lives in medicine."
Current studies highlight that AI's role in visualization is not merely supplementary; it is becoming crucial for advancing medical research and enhancing patient care outcomes. Furthermore, ethical considerations surrounding AI's implementation must be addressed to ensure responsible use in clinical settings. As AI technology continues to progress, its applications in imaging techniques will increasingly influence the future of healthcare diagnostics.

Tissue Doppler Imaging (TDI) represents a groundbreaking echocardiographic technique that employs imaging techniques to provide critical insights into cardiac function by quantifying the velocity of myocardial motion. This advanced technology utilizes imaging techniques that significantly enhance the assessment of diastolic function and can identify early indicators of heart disease, establishing itself as an essential tool in cardiac diagnostics. Recent studies have demonstrated that TDI can predict negative outcomes in individuals with heart failure and preserved ejection fraction, with specific velocity thresholds indicating an increased mortality risk. For instance, reduced S' and E' velocities are associated with more than a two-fold increase in the risk of death, heart failure, or new myocardial infarction in patients with ST-elevation myocardial infarction.
In clinical research, imaging techniques like TDI are pivotal in evaluating the efficacy of new cardiac therapies and interventions. Its capacity to measure both systolic and diastolic velocities facilitates a nuanced understanding of how these therapies influence heart function. By incorporating imaging techniques such as TDI into research protocols, clinicians can achieve more accurate diagnoses and formulate tailored treatment strategies, ultimately enhancing patient outcomes. Ugo Giulio Sisto highlights that TDI, as one of the essential imaging techniques, serves as an indispensable diagnostic and prognostic tool for acute coronary syndromes, aiding in the assessment of systolic or diastolic dysfunction and contributing to the etiological diagnosis of acute heart failure.
The real-world applications of TDI as one of the imaging techniques extend to assessing left ventricular filling pressures in acute heart failure, where traditional echocardiography may miss subtle dysfunction. Furthermore, TDI is one of the imaging techniques that has proven invaluable in distinguishing between cardiogenic and non-cardiogenic pulmonary edema, thereby improving diagnostic accuracy in critical care settings. Its ability to detect organ damage in hypertensive emergencies further underscores TDI's diagnostic capabilities. As the field of cardiology evolves, TDI emerges as a powerful adjunct to conventional echocardiography, providing detailed, real-time quantitative insights through advanced imaging techniques that are essential for effective cardiac care.

Advanced imaging techniques are essential for monitoring respiratory muscle function, significantly influencing the management of chronic obstructive pulmonary disease (COPD) and neuromuscular disorders. Imaging techniques, including ultrasound and MRI, provide comprehensive assessments of diaphragm and intercostal muscle function, enabling clinicians to detect dysfunction early and tailor interventions accordingly. For instance, diaphragm thickening fractions exceeding 29% correlate with a high probability of successful weaning from mechanical ventilation, while diaphragm thickening fractions during deep breathing range from 150% to 200%. This underscores the importance of precise visualization in clinical decision-making.
In clinical research, these imaging techniques are instrumental in evaluating novel treatments aimed at enhancing respiratory function. Advanced ultrasound imaging techniques, such as tissue Doppler visualization and shear wave elastography, enhance the capabilities of traditional assessments by providing insights into muscle stiffness and contractility. This progression in visual technology, especially through the use of imaging techniques, not only aids in diagnosing conditions but also plays a pivotal role in monitoring treatment effectiveness, ultimately leading to improved patient outcomes and a better quality of life.
Pulmonologists emphasize the transformative impact of diagnostic techniques in managing COPD. As one specialist noted, integrating advanced visualization techniques into routine practice can significantly deepen our understanding of respiratory muscle dynamics, facilitating more effective therapeutic strategies. Moreover, the potential of PET-MRI for evaluating respiratory muscles showcases the evolving landscape of imaging techniques in respiratory care. Ongoing research into these modalities continues to reveal their promise in optimizing care for individuals facing respiratory challenges. Emerging portable scanning technologies could further enhance continuous monitoring in ICU settings, thereby improving the care provided to critically ill patients.

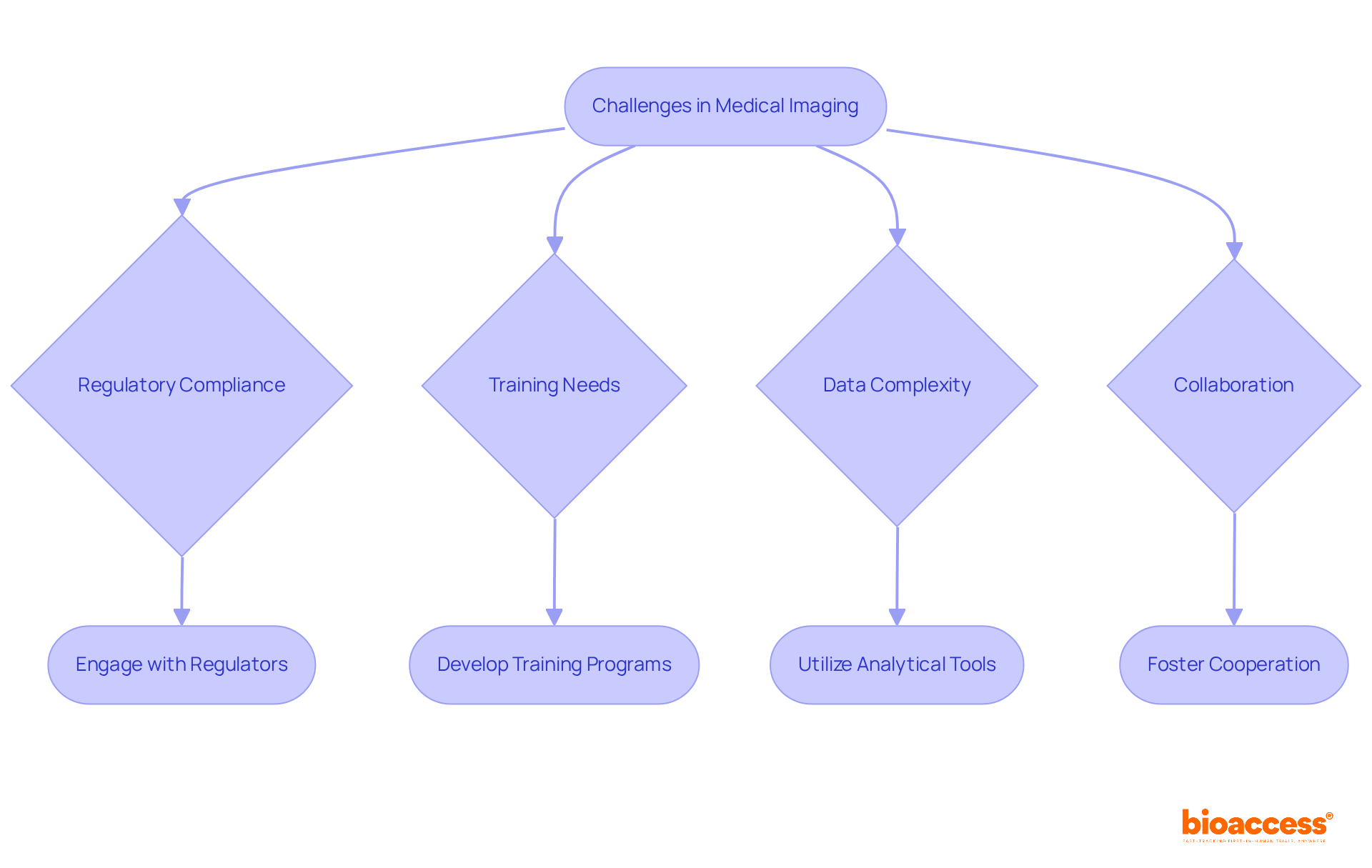
The rapid evolution of medical visualization technology presents numerous challenges that researchers and clinicians must adeptly navigate. A primary concern is the necessity for strict adherence to regulatory standards, which is essential for ensuring patient safety and the effectiveness of new diagnostic techniques. As advanced visualization methods are integrated into existing workflows, healthcare professionals face the dual challenge of adapting to these innovations while also addressing their training needs. Furthermore, the increasing complexity of visual data underscores the critical need for robust analytical tools and methods capable of deriving significant insights. By proactively addressing these challenges, the medical community can fully harness advanced diagnostic methods to enhance patient care and propel research efforts forward.
Industry leaders emphasize that a clearly outlined healthcare and regulatory strategy is crucial for optimizing the development process. Cooperation among practitioners, researchers, and regulators is essential for effective medical device translation. Current trends indicate that adherence to evolving regulatory frameworks is vital, particularly as new imaging techniques emerge, which necessitate thorough validation to meet safety and effectiveness criteria. To navigate these advancements effectively, early engagement with regulators is paramount.
bioaccess offers comprehensive clinical trial management services, including:
These services can significantly aid in overcoming the challenges posed by the evolving landscape of imaging techniques in medicine. Engaging with bioaccess provides the necessary support to ensure a smooth transition into this dynamic field, ultimately enhancing the capabilities of clinical research.
The landscape of clinical research is undergoing a significant transformation through advanced imaging techniques, which are crucial in enhancing diagnostic accuracy and improving patient outcomes. These innovations not only expedite the research process but also offer deeper insights into various medical conditions, revolutionizing how healthcare professionals approach diagnosis and treatment. The incorporation of technologies such as Ultrasound Shear Wave Elastography, Photon-Counting Computed Tomography, and Artificial Intelligence in imaging represents a substantial leap toward more precise and efficient medical care.
Key arguments presented illustrate the multifaceted benefits of these imaging techniques. For instance, advancements like High-Resolution Magnetic Resonance Imaging and Contrast-Enhanced Ultrasound have proven invaluable in assessing complex medical conditions, while Ultrafast Ultrasound and Tissue Doppler Imaging enhance real-time decision-making in critical care settings. The commitment of organizations like bioaccess® to streamline clinical research processes ensures that these technologies can be rapidly implemented, ultimately benefiting patient care through improved diagnostic capabilities.
As the field of medical imaging continues to evolve, it is imperative for healthcare professionals to embrace these advancements and tackle the accompanying challenges, such as regulatory compliance and data complexity. The future of clinical research relies on the successful integration of these innovative imaging techniques, which promise to enhance diagnostic precision and optimize patient management strategies. Engaging with advanced imaging solutions is not merely a step forward in medical research; it is a commitment to improving health outcomes and advancing the quality of care provided to patients.
What is bioaccess® and what role does it play in clinical research?
bioaccess® is an organization at the forefront of clinical research, particularly focusing on advanced imaging techniques. It accelerates the development and implementation of innovative visual technologies, obtaining ethical approvals within a timeframe of 4-6 weeks to enhance participant enrollment.
How does bioaccess®'s approach impact healthcare advancements?
By ensuring quick ethical approvals and efficient participant enrollment, bioaccess® significantly improves the pace of research in imaging techniques, leading to advancements in diagnostic capabilities and health outcomes.
What is Ultrasound Shear Wave Elastography (SWE) and its significance?
SWE is a non-invasive imaging technique that quantifies tissue stiffness, providing critical insights into medical conditions. It enhances tumor and liver disease characterization, leading to more accurate diagnoses and better treatment planning.
How effective is SWE in distinguishing between benign and malignant lesions?
SWE has shown a remarkable sensitivity of 97% in identifying malignant focal liver lesions, making it a valuable tool in medical diagnostics.
What are the implications of increased liver stiffness values measured by SWE?
Increased stiffness values are linked to a higher risk of malignancy, with a hazard ratio of 2.57 for mortality from cardiovascular disease in individuals with elevated liver stiffness.
What are the technical limitations of SWE?
SWE faces challenges such as operator dependency and variability in measurements, which can affect its reproducibility.
What is Photon-Counting Computed Tomography (PCCT) and how does it differ from conventional CT?
PCCT is an advanced imaging technique that counts individual photons to deliver superior image quality and reduce radiation exposure, unlike conventional CT systems that use energy-integrating detectors.
What are the safety benefits of using PCCT?
PCCT can reduce radiation exposure by 20%-30% in young individuals without compromising image quality. It also allows for lower doses of iodinated contrast, enhancing safety for patients with renal dysfunction.
How does PCCT contribute to medical research?
PCCT facilitates more accurate evaluations of disease progression and treatment responses, showcasing its essential value in developing innovative healthcare solutions.
What is the future outlook for imaging techniques like PCCT?
Technologies like PCCT are expected to shape the future of CT scanning, influencing medical decision-making and improving diagnostic precision.