


The article centers on the critical medical device types that clinical research directors must understand, underscoring their regulatory requirements and importance in clinical studies. It delineates various categories, including:
Grasping these device types and their compliance landscapes is essential for achieving successful clinical research outcomes and facilitating market entry. This understanding not only enhances the effectiveness of clinical studies but also ensures adherence to regulatory standards, which is paramount in the Medtech landscape.
Understanding the diverse landscape of medical devices is crucial for clinical research directors who aim to drive innovation in healthcare. A multitude of device types exists, ranging from low-risk bandages to high-risk implantable devices, each presenting unique regulatory challenges and opportunities. How can clinical research leaders effectively navigate this complex environment to ensure compliance while accelerating the path to market for groundbreaking medical solutions? This article delves into ten essential medical device types, illuminating their regulatory frameworks and the strategic insights necessary for successful clinical trials.
bioaccess® leads the way in advancing medical studies for healthcare tools by expertly navigating the complex compliance landscapes of Latin America, the Balkans, and Australia. With ethical approvals achieved in a mere 4-6 weeks and enrollment rates that outpace traditional markets by 50%, bioaccess® enables Medtech innovators to accelerate their market entry. This strategic approach not only enhances the effectiveness of medical studies but also ensures that groundbreaking health products reach patients in need more swiftly, ultimately contributing to improved health outcomes globally. The rapid governance in these regions significantly influences clinical research success rates, facilitating timely access to innovative solutions that can revolutionize patient care.

Class I medical device types are categorized as low-risk products, subject to minimal oversight. Common examples of medical device types are:
These medical device types primarily require basic controls to ensure their safety and effectiveness, including appropriate labeling and compliance with manufacturing practices. For clinical research directors, understanding the regulatory environment surrounding Class I items is crucial, particularly in Colombia, where INVIMA (Colombia National Food and Drug Surveillance Institute) oversees the marketing and production of health products. As a Level 4 health authority recognized by PAHO/WHO, INVIMA ensures that even low-risk products adhere to stringent safety standards. Recent advancements in safety regulations have further underscored the significance of compliance, ensuring that these tools are both reliable and effective. Successful trials for Class I instruments not only demonstrate their safety but also highlight the necessity for coordinators to stay informed about evolving regulations and best practices in the field. Furthermore, collaborating with specialists such as bioaccess® can streamline trial processes, providing Medtech, Biopharma, and Radiopharma startups with essential support to navigate the complexities of compliance approval and site activation for trials.

Class II medical device types, such as infusion pumps and surgical drapes, necessitate a 510(k) clearance, which demonstrates substantial equivalence to a legally marketed item. This procedure involves a rigorous assessment of the product's safety and efficacy. Therefore, it is crucial for clinical research leaders to grasp the intricacies of this compliance pathway. Mastering the 510(k) process can significantly affect both the timeline and the success of bringing a medical product to market.

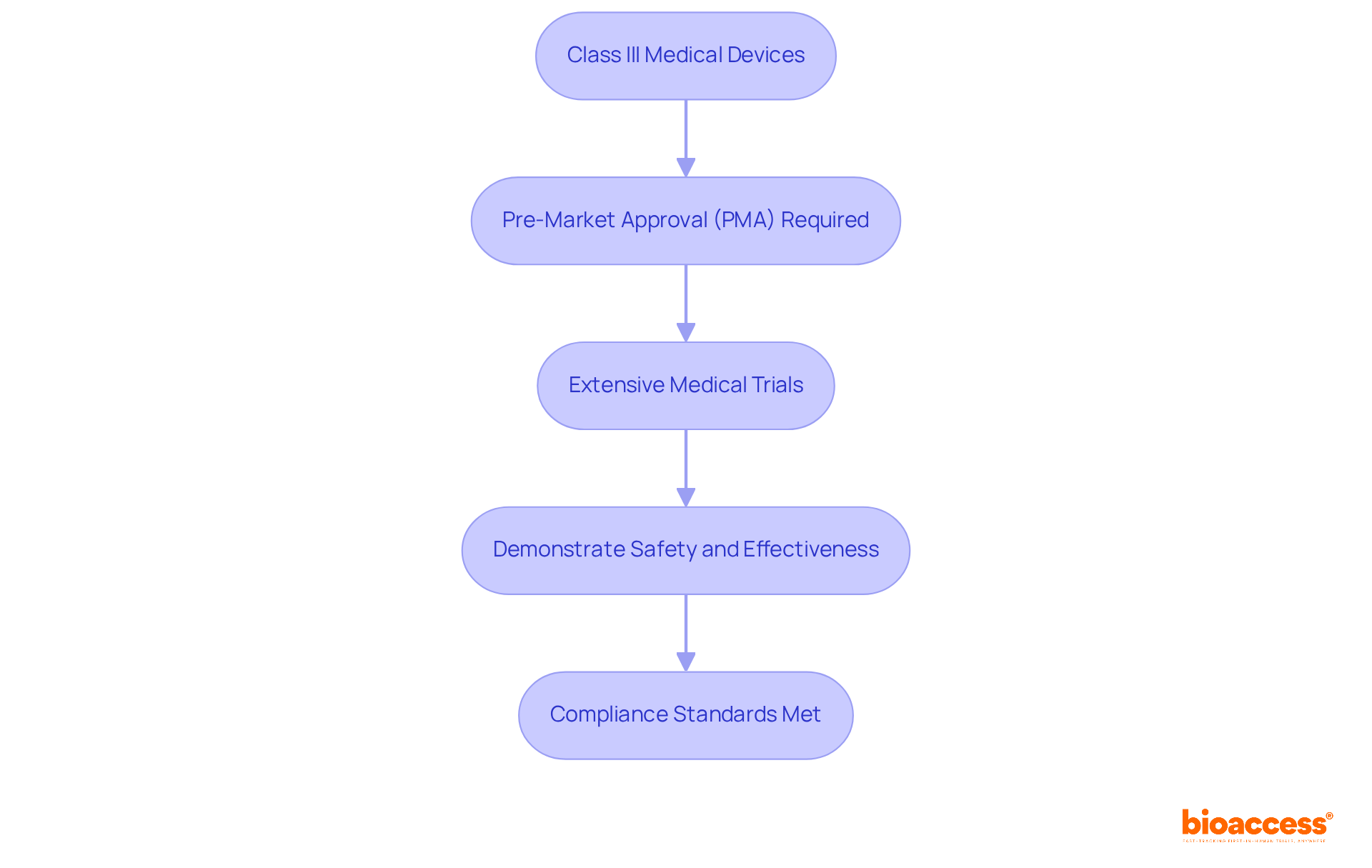
Class III medical instruments, including pacemakers and implantable defibrillators, are classified as high-risk devices that require pre-market approval (PMA) from regulatory authorities. This rigorous process involves extensive medical trials designed to demonstrate the safety and effectiveness of these devices.
For trial supervisors, understanding the PMA process is crucial; it dictates the planning and execution of studies, ensuring that all compliance standards are met before a product can be marketed. The implications of this regulatory framework underscore the importance of meticulous oversight in clinical research.
Software as a Medical Device (SaMD) is a category of software among different medical device types, specifically created for medical purposes and distinct from hardware medical devices. This category includes various medical device types, such as mobile health applications and diagnostic software.
The regulatory landscape governing SaMD is evolving, which compels directors of medical studies to stay informed about the guidelines and standards that dictate software development and validation. Grasping these regulations is essential for guaranteeing the safety and effectiveness of SaMD products for patient use.

In Vitro Diagnostic Devices (IVDs) play a crucial role in the detection of diseases and the monitoring of health conditions. Devices such as blood glucose meters and pregnancy tests exemplify their importance. IVDs are governed by specific oversight requirements that guarantee their accuracy and reliability.
For research directors in healthcare, grasping the regulatory landscape surrounding IVDs is vital, as it significantly impacts study design and the validation of diagnostic claims.

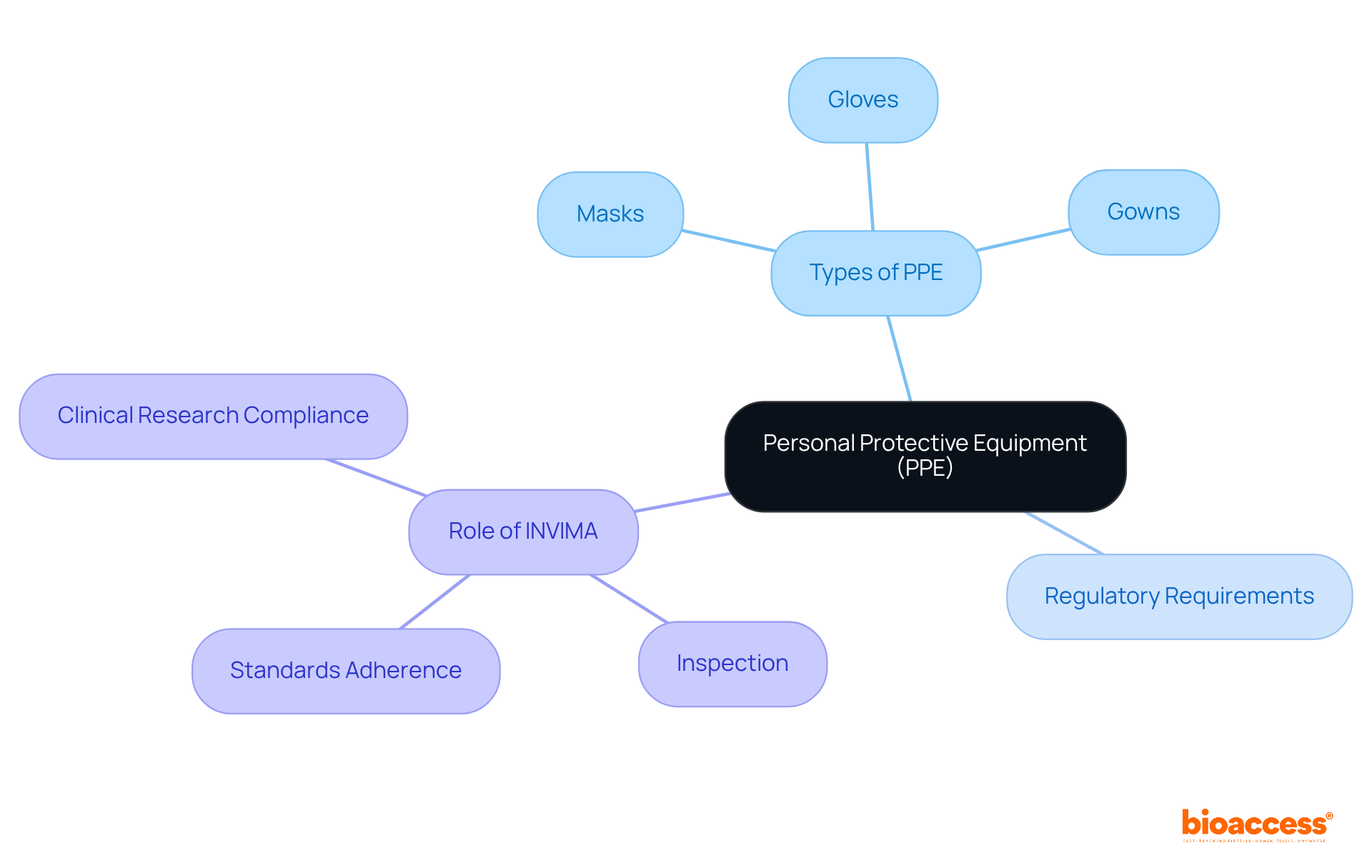
Personal Protective Equipment (PPE), including masks, gloves, and gowns, is essential for maintaining health safety, particularly in healthcare environments. Regulatory requirements for PPE are designed to ensure that these products meet safety standards, safeguarding both healthcare workers and patients.
In Colombia, the National Food and Drug Surveillance Institute (INVIMA) plays a pivotal role in this oversight. Established in 1992 under the Ministry of Health and Social Protection, INVIMA is tasked with inspecting and supervising the marketing and manufacturing of health products, including PPE. It rigorously assesses adherence to health standards and implements best practices, ensuring that various medical device types, including PPE, are both safe and effective.
Recognized as a Level 4 health authority by the Pan American Health Organization/World Health Organization, INVIMA's stringent regulatory framework is vital for guaranteeing the quality and safety of medical device types used in clinical studies. Clinical research directors must remain cognizant of these regulations to ensure compliance and safety in their studies, especially in light of recent global health challenges.
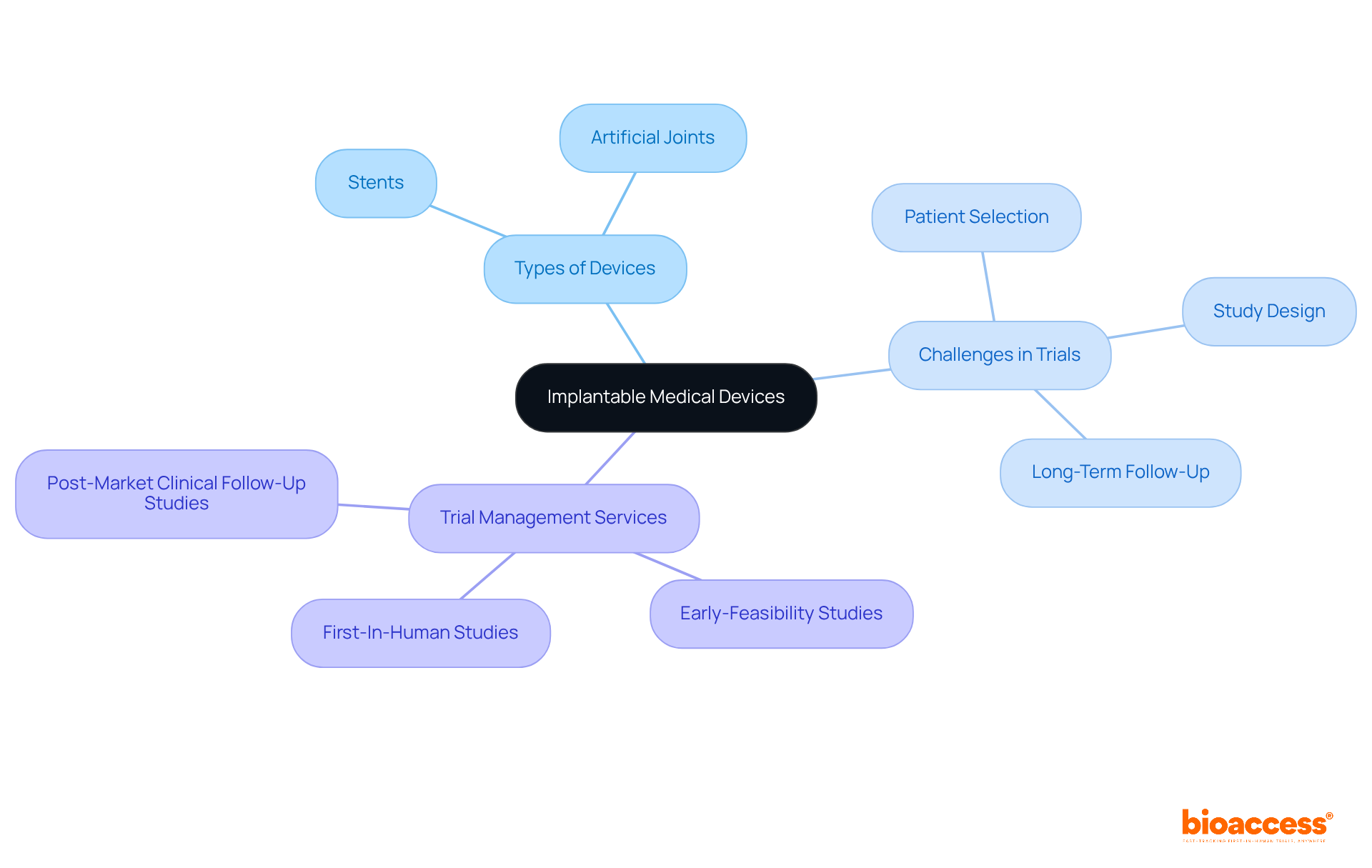
Implantable medical instruments, including stents and artificial joints, are designed for long-term integration within the body. These instruments require comprehensive medical trials to ensure their safety and efficacy over time. For research directors in healthcare, understanding the unique challenges associated with different medical device types, including implantable devices, is essential, as it influences study design, patient selection, and the requirements for long-term follow-up.
Leveraging the expertise of specialized trial management services, such as those offered by bioaccess®, which has a robust presence in Latin America, can markedly enhance the efficiency of these studies. With over 20 years of experience in Medtech, bioaccess® delivers a wide array of services, encompassing:
This ensures that trials are executed with precision and regulatory compliance. Their expedited approval process facilitates a rapid 6-8 week timeline for submissions, allowing for quicker patient enrollment, particularly within cardiology and neurology groups. This approach not only addresses common recruitment challenges but also integrates targeted strategies to enhance site participation and patient eligibility, streamlining the pathway to successful trial outcomes.
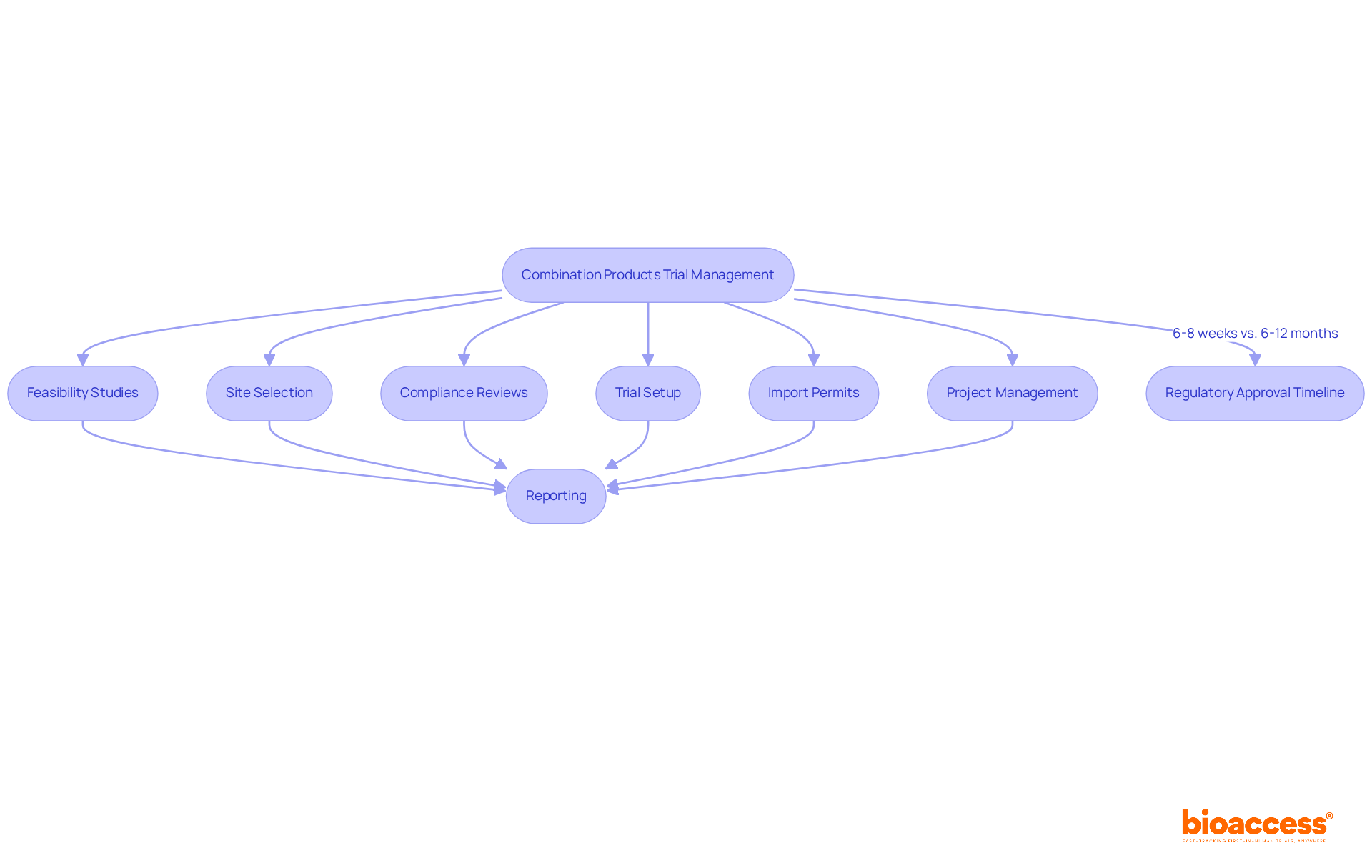
Combination products, which integrate drugs and devices, such as drug-eluting stents, present unique oversight challenges that necessitate a nuanced understanding of both drug and device approval processes. These products must meet the stringent criteria established for each category, requiring research leaders to navigate a complicated oversight environment efficiently.
At bioaccess®, we offer extensive trial management services that encompass:
This ensures meticulous handling of all trial process elements. Our accelerated regulatory approval process allows for approvals in just 6-8 weeks, significantly faster than the typical 6-12 months seen in the US and EU. This efficiency enables us to enroll treatment-naive cardiology or neurology cohorts 50% faster than Western sites.
As the combination of medications and instruments continues to progress, clinical study directors must ensure adherence and safety throughout the development process, utilizing their expertise to manage the unique demands of these innovative therapies.
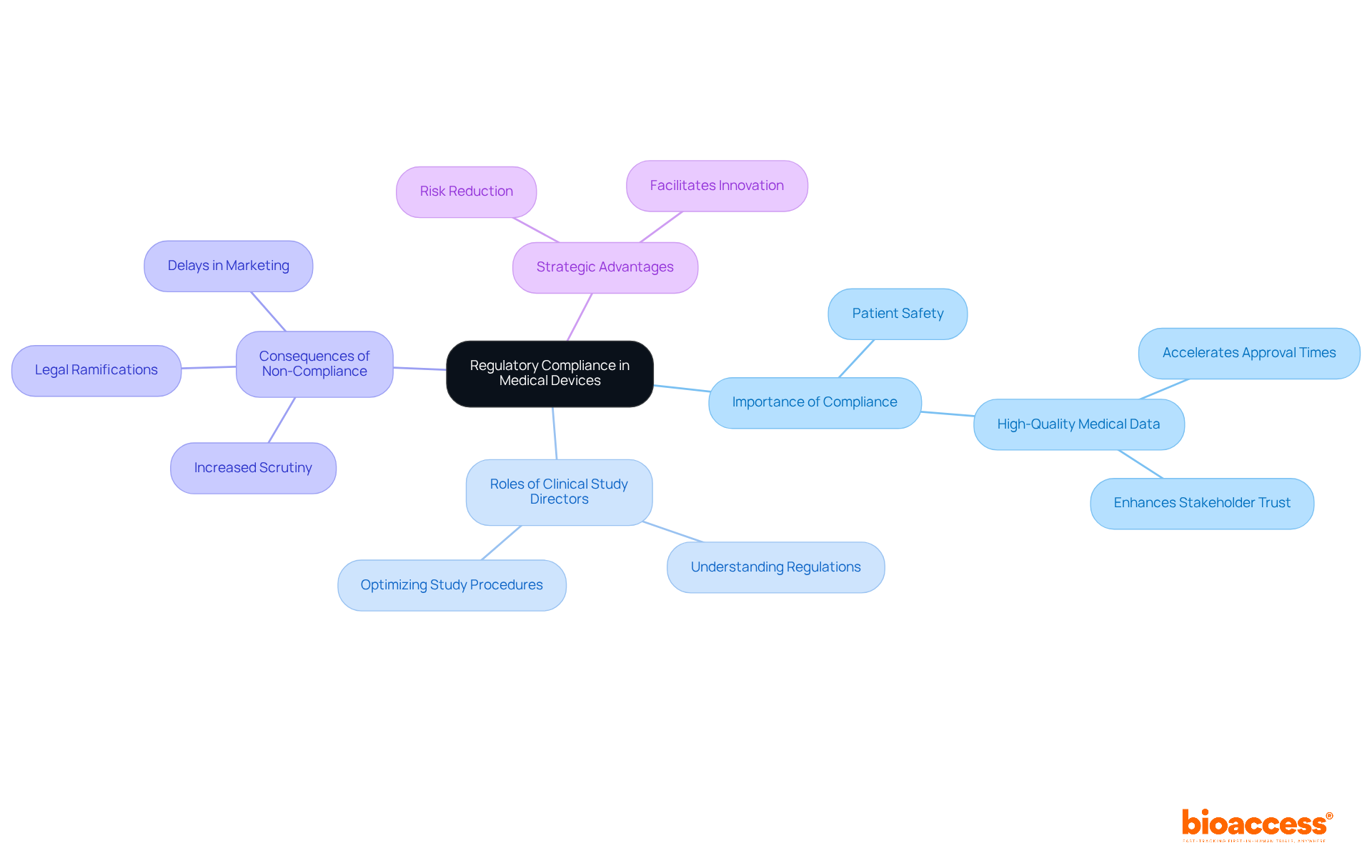
Regulatory compliance is essential for ensuring the safety and effectiveness of medical equipment. Clinical study directors must possess a thorough understanding of the regulations specific to the various medical device types, as non-compliance can result in significant delays and jeopardize patient safety. High-quality medical data is vital; it not only accelerates approval and clearance times but also enhances stakeholder trust in the development process.
By emphasizing compliance with regulations, clinical research leaders can optimize study procedures, reduce risks, and ultimately facilitate the successful marketing of innovative medical products. The consequences of non-compliance can be severe, leading to increased scrutiny from oversight agencies and potential legal ramifications, underscoring the need for robust compliance strategies.
Staying updated on the latest medical device types and their safety regulations is crucial, as these guidelines evolve to address emerging challenges in the industry. In this dynamic landscape, effective compliance management is not merely a regulatory obligation but a strategic advantage that can significantly impact clinical trial timelines and outcomes.
Understanding the essential types of medical devices is crucial for clinical research directors who aim to navigate the complex landscape of medical product development. This article highlights ten key categories, ranging from low-risk Class I devices to high-risk Class III instruments, each accompanied by distinct regulatory requirements that significantly impact the speed and efficacy of bringing innovative healthcare solutions to market.
The discussion encompasses various device types, including:
It emphasizes the paramount importance of regulatory compliance at every stage. Insights into the specific requirements for each category, such as the 510(k) clearance for Class II devices and pre-market approval for Class III devices, illustrate the critical role that understanding these regulations plays in successful clinical trials and product launches.
In conclusion, the landscape of medical devices is ever-evolving. Staying informed about the latest regulations and device types is imperative for clinical research directors. By prioritizing compliance and leveraging the expertise of specialized services, such as those offered by bioaccess®, stakeholders can enhance the efficiency of their trials and ultimately improve patient outcomes. Embracing this knowledge not only facilitates timely access to innovative solutions but also reinforces the commitment to safety and efficacy in medical device development.
What is bioaccess® and what role does it play in clinical research for medical devices?
bioaccess® is a company that accelerates clinical research for medical devices by navigating the complex compliance landscapes of regions such as Latin America, the Balkans, and Australia. They achieve ethical approvals in 4-6 weeks and have enrollment rates that exceed traditional markets by 50%, enabling faster market entry for Medtech innovators.
How does bioaccess® impact the effectiveness of medical studies?
bioaccess® enhances the effectiveness of medical studies by ensuring that innovative health products reach patients more swiftly, which contributes to improved health outcomes globally. Their strategic approach facilitates timely access to innovative solutions that can revolutionize patient care.
What are Class I medical devices and what regulatory controls apply to them?
Class I medical devices are categorized as low-risk products and are subject to minimal regulatory oversight. Examples include bandages, examination gloves, and handheld surgical instruments. These devices primarily require basic controls for safety and effectiveness, including appropriate labeling and compliance with manufacturing practices.
What is the role of INVIMA in regulating Class I medical devices in Colombia?
INVIMA (Colombia National Food and Drug Surveillance Institute) oversees the marketing and production of health products in Colombia. As a Level 4 health authority recognized by PAHO/WHO, INVIMA ensures that even low-risk Class I products adhere to stringent safety standards.
Why is it important for clinical research directors to understand the regulatory environment for Class I medical devices?
It is crucial for clinical research directors to understand the regulatory environment surrounding Class I items to ensure compliance with safety regulations and to successfully navigate the complexities of trial processes. This knowledge helps in demonstrating the safety and effectiveness of these devices.
What are Class II medical devices and what is required for their clearance?
Class II medical devices, such as infusion pumps and surgical drapes, are considered moderate-risk products that require a 510(k) clearance. This clearance demonstrates substantial equivalence to a legally marketed item and involves a rigorous assessment of the product's safety and efficacy.
How does mastering the 510(k) process affect medical product development?
Mastering the 510(k) process is crucial for clinical research leaders, as it significantly impacts both the timeline and success of bringing a medical product to market. Understanding this compliance pathway can streamline the development and approval process.