


Medical wearables are revolutionizing clinical research and care by facilitating continuous real-time monitoring, enabling early detection of health issues, and empowering patients to take an active role in managing their wellness. This article delineates how these devices enhance patient outcomes through:
Furthermore, it addresses the challenges associated with data privacy and user compliance, emphasizing the necessity for collaboration among stakeholders to overcome these hurdles.
Medical wearables are at the forefront of a healthcare revolution, seamlessly merging technology with patient care to enhance clinical research and outcomes. These devices are gaining traction, offering unprecedented opportunities for real-time monitoring, personalized treatment, and proactive health management, fundamentally altering the delivery of healthcare. However, as the adoption of this technology accelerates, significant challenges such as data privacy, user compliance, and integration within existing healthcare systems persist.
How can stakeholders navigate these complexities to fully harness the transformative potential of medical wearables?
bioaccess® leverages its extensive experience in early-phase clinical research to facilitate the rapid integration of medical devices into clinical trials. By capitalizing on Latin America's regulatory efficiency and diverse patient populations, particularly in Colombia, bioaccess® can secure ethical approvals in just 4-6 weeks. This significantly accelerates the timeline for technology studies, enabling innovators in Medtech, Biopharma, and Radiopharma to efficiently test and validate their medical wearables.
Moreover, Colombia offers a cost-saving advantage exceeding 30% compared to trials in North America or Western Europe, complemented by a robust medical system ranked among the best globally. These elements not only expedite market entry but also improve outcomes for individuals and invigorate local economies through job creation and advancements in medical services.

Medical wearables enable continuous real-time monitoring of individuals, empowering medical professionals to effortlessly track vital signs, activity levels, and other health metrics. This capability markedly enhances healthcare by enabling timely interventions and personalized treatment plans.
For example, devices that monitor heart rate and blood pressure can alert healthcare professionals to potential issues before they escalate, thereby improving safety and patient outcomes. Research indicates that Remote Health Monitoring (RPM) can reduce hospital readmissions by up to 76% and decrease the length of stay for chronic patients by 25%. Moreover, RPM programs can help providers save approximately $1,000 per individual annually, underscoring the financial benefits of these technologies.
The integration of these devices into clinical workflows ensures that healthcare professionals have immediate access to critical information, fostering a proactive approach to health management. Continuous monitoring of health metrics not only empowers individuals but also enhances adherence to treatment plans, with studies showing that RPM can increase engagement by as much as 80%.
As the adoption of medical wearables expands, their transformative potential for patient care and safety becomes increasingly clear. Nonetheless, addressing ethical and privacy concerns surrounding data use in predictive analytics is essential, as these issues could affect the widespread acceptance of monitoring devices in healthcare.
As Viviana Gradinaru emphasizes, 'There is significant value for well individuals to have these regular measurements, to have a time course and, based on that timeline, to intervene with actionable, beneficial behaviors to prolong their lifespan.
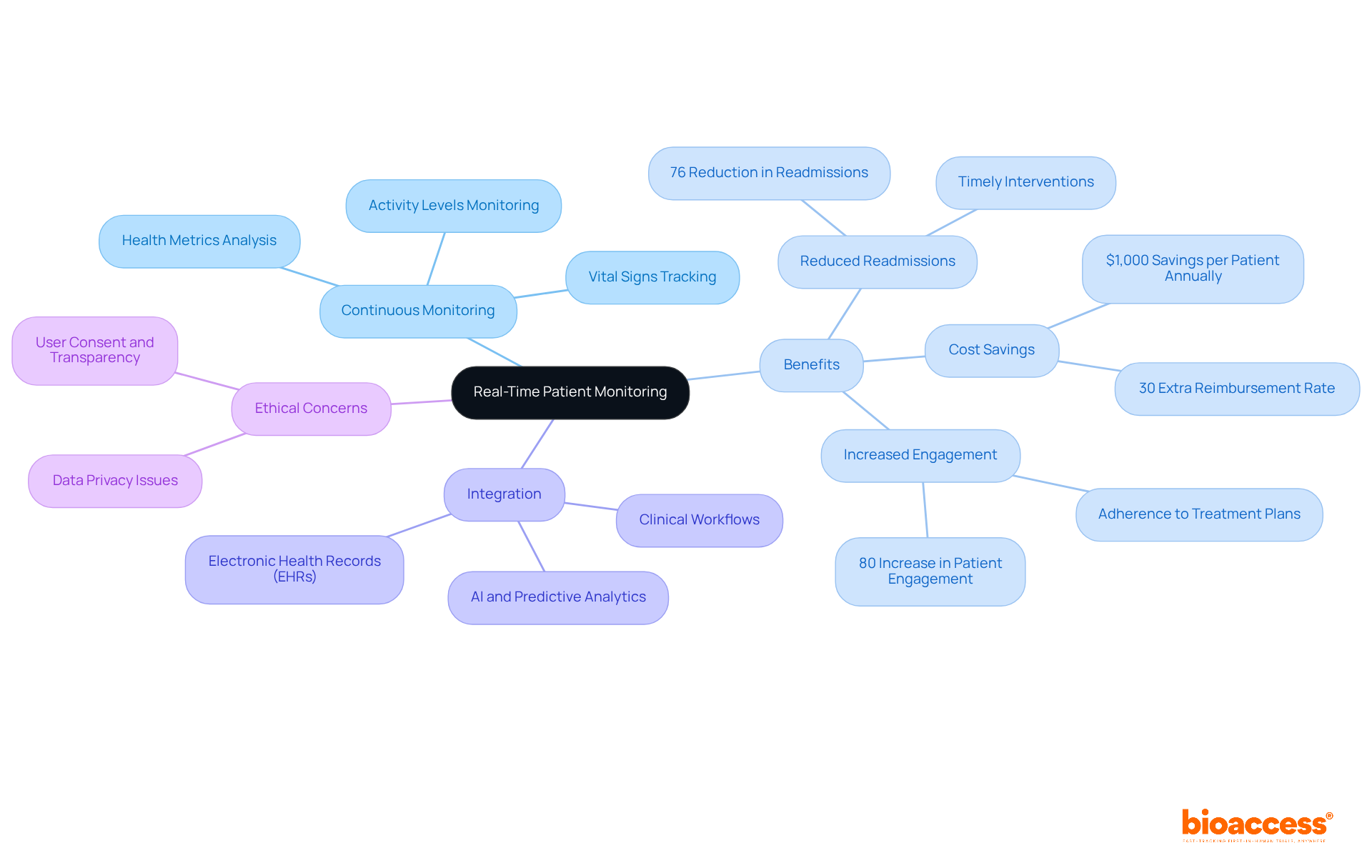
Incorporating portable technology into medical systems significantly enhances individual management by ensuring that information gathered from devices is seamlessly integrated into electronic medical records (EMRs). This integration enables medical providers to access extensive individual data, which facilitates improved decision-making and coordinated care.
For instance, portable devices can automatically transfer wellness metrics to electronic medical records, thereby decreasing the administrative load on medical personnel and allowing them to concentrate more on providing care for individuals.
Furthermore, interoperability between wearables and healthcare systems boosts the overall efficiency of individual management, resulting in better wellness outcomes.

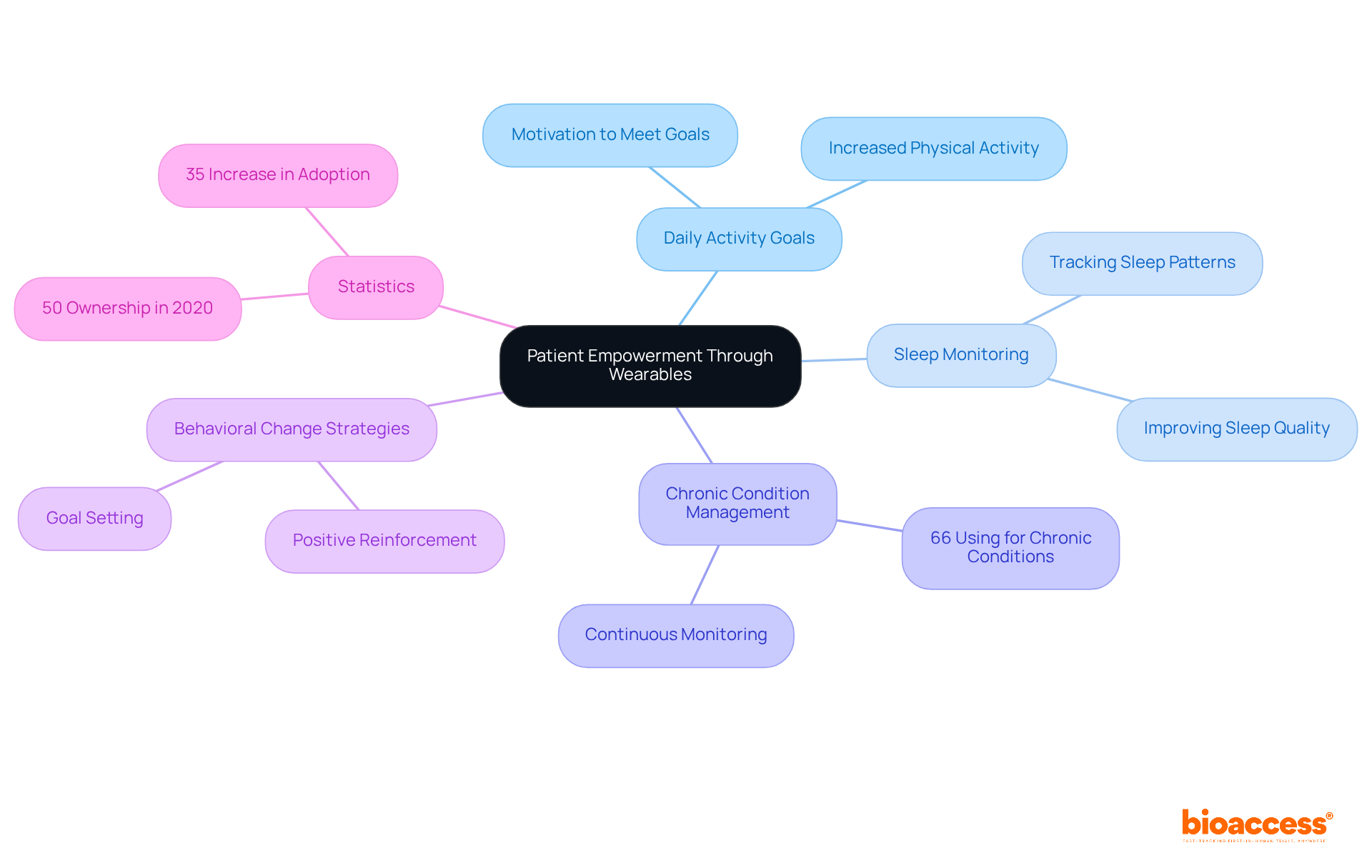
Medical wearables empower individuals by providing real-time insights on wellness metrics, motivating them to take an active role in managing their well-being. For instance, medical wearables such as fitness trackers and smartwatches inspire users to:
This self-monitoring capability fosters a sense of responsibility for one's health, leading to improved adherence to treatment plans and healthier lifestyle choices. By enabling patients to track their progress and set personal wellness objectives, medical wearables significantly enhance patient engagement and satisfaction.
As noted by Harjeevan Singh Kang, the ability of these devices to employ various behavior modification strategies to promote positive behavior change presents a substantial opportunity for individuals willing to take greater responsibility for their health and care. Additionally, financial incentives, such as reduced insurance costs for using these devices, can further motivate individuals to engage with this technology, ultimately transforming their wellness management experience.
Notably, ownership of medical wearables surged to 50% in 2020, with 66% of new users employing medical wearables for chronic condition management. However, privacy concerns have also emerged, underscoring the necessity for comprehensive evaluation of data security as these devices become increasingly integrated into wellness management systems.
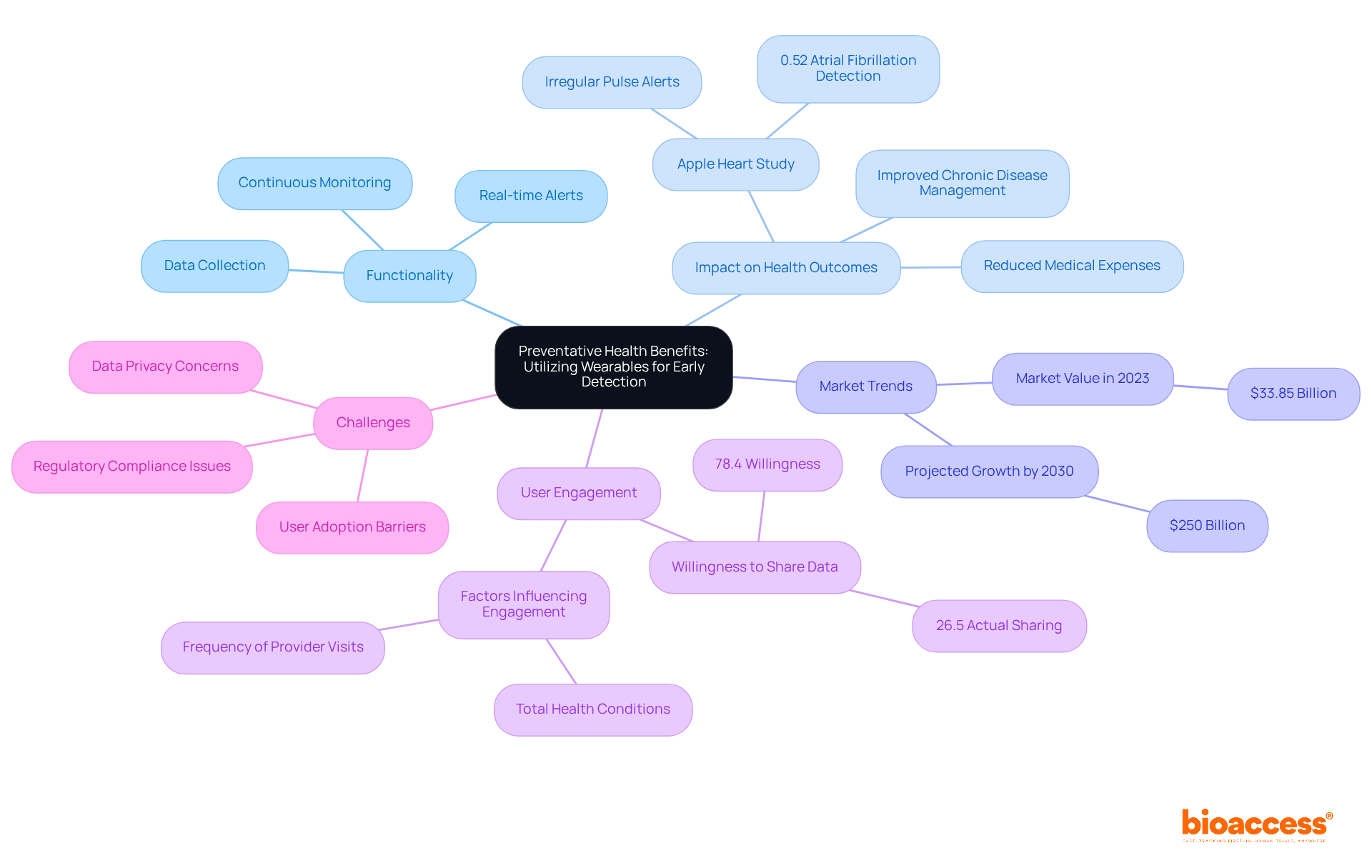
Medical wearables are revolutionizing preventative wellness by enabling the early identification of potential medical concerns. Medical wearables equipped with advanced sensors continuously monitor vital signs and physiological parameters, alerting users and healthcare providers to abnormalities that may indicate underlying health issues.
For instance, devices that track heart rate variability can detect irregularities, potentially preventing cardiovascular incidents. A significant study, the Apple Heart Study, demonstrated that irregular pulse alerts from medical wearables, such as smartwatches, effectively identified atrial fibrillation in 0.52% of participants, underscoring the capability of consumer-grade devices in early disease detection.
By enabling prompt interventions, these devices not only enhance health outcomes but also contribute to reducing medical expenses, emphasizing the critical role of preventative care in modern healthcare systems. As the global market for medical devices was valued at $33.85 billion in 2023 and is projected to reach $250 billion by 2030, the focus on their integration into clinical practice is increasingly pertinent.
Moreover, while 78.4% of device users expressed a willingness to share information with medical providers, only 26.5% actually did so, highlighting a significant gap in user engagement. Additionally, factors such as the frequency of medical provider appointments and the total number of health conditions serve as important indicators of device usage, which are vital for understanding their acceptance in clinical settings.
However, challenges related to data privacy and regulatory compliance continue to pose substantial barriers to the widespread adoption of wearable technology. As Ranganathan Chandrasekaran notes, medical wearables have the potential to transform medical service delivery by enabling real-time, continuous monitoring that fosters early disease detection, personalized treatments, and increased patient engagement.
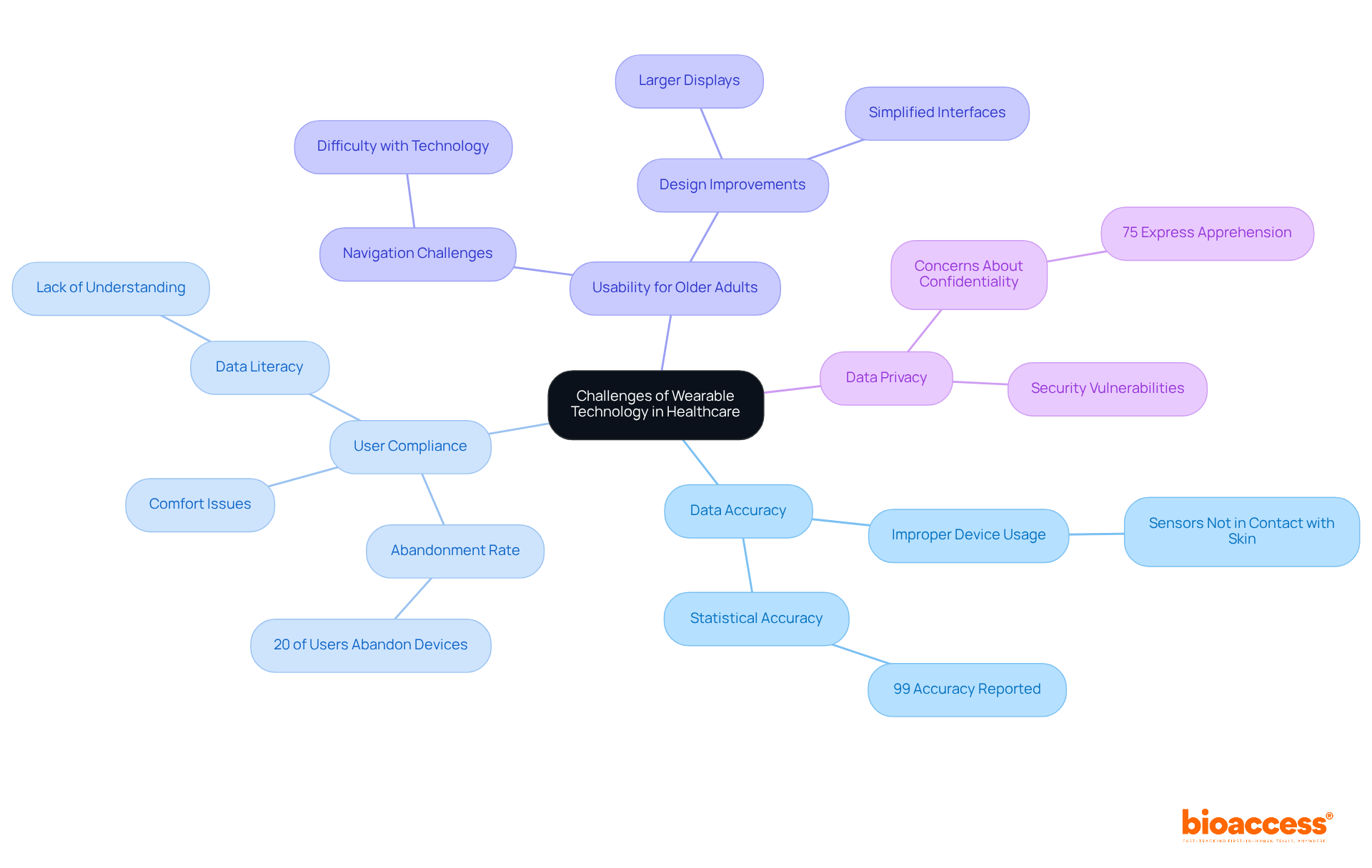
Despite the numerous advantages of medical wearables, several obstacles impede their widespread acceptance in medical settings. Data accuracy is a paramount concern, with the precision of personal devices typically reaching 99%, as reported by the National Library of Medicine. However, discrepancies in data collection may occur due to improper device usage, particularly when sensors are not in direct contact with the skin. User compliance with medical wearables presents another significant barrier; studies reveal that 20% of users abandon their medical wearables, often due to comfort issues or a lack of data literacy, which can adversely impact healthcare outcomes.
Usability is particularly critical for older adults, who may struggle with navigating technology. Enhancing the design and functionality of medical wearables for this demographic is essential. For instance, incorporating larger displays and simplified interfaces, as suggested in various studies, can markedly enhance user experience. Furthermore, addressing concerns about data privacy and security is vital, as 75% of individuals express apprehension regarding the confidentiality of their health information, a statistic highlighted in recent surveys.
To address these challenges, collaboration among technology creators, medical providers, and patients is crucial. Specific steps stakeholders can undertake include:
By focusing on these areas, stakeholders can significantly enhance the adoption and effectiveness of medical wearables as personal technology in healthcare.
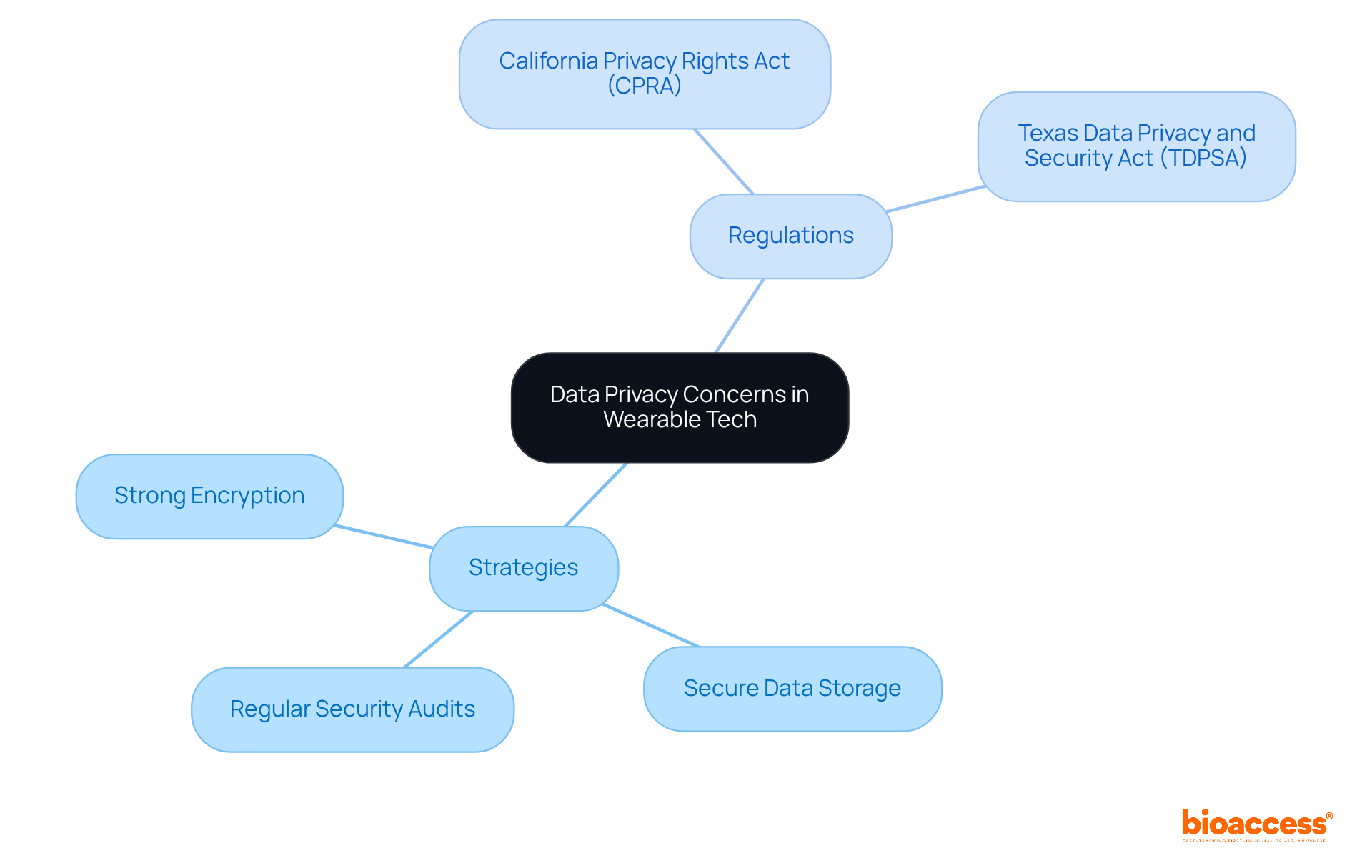
Data privacy stands as a pivotal concern in the realm of portable technology, given that these devices gather sensitive health information from users. To uphold patient trust and comply with regulations such as HIPAA, it is imperative to implement robust data protection measures. Key strategies encompass:
Moreover, clear privacy policies that explicitly outline data usage and sharing practices are vital for fostering user trust in medical wearables. For example, organizations can adopt a zero-trust model, ensuring that only authorized personnel have access to sensitive data, thus minimizing the risk of breaches.
Current regulations, including the California Privacy Rights Act (CPRA) and the Texas Data Privacy and Security Act (TDPSA), mandate stringent compliance regarding the handling of biometric data and personal health information. These laws necessitate entities to provide opt-out rights and adhere to principles of data minimization and purpose limitation. By emphasizing data privacy and adhering to these guidelines, stakeholders can enhance the acceptance and utilization of medical wearables in medical environments, ultimately leading to improved patient outcomes and increased confidence in innovative health technologies.
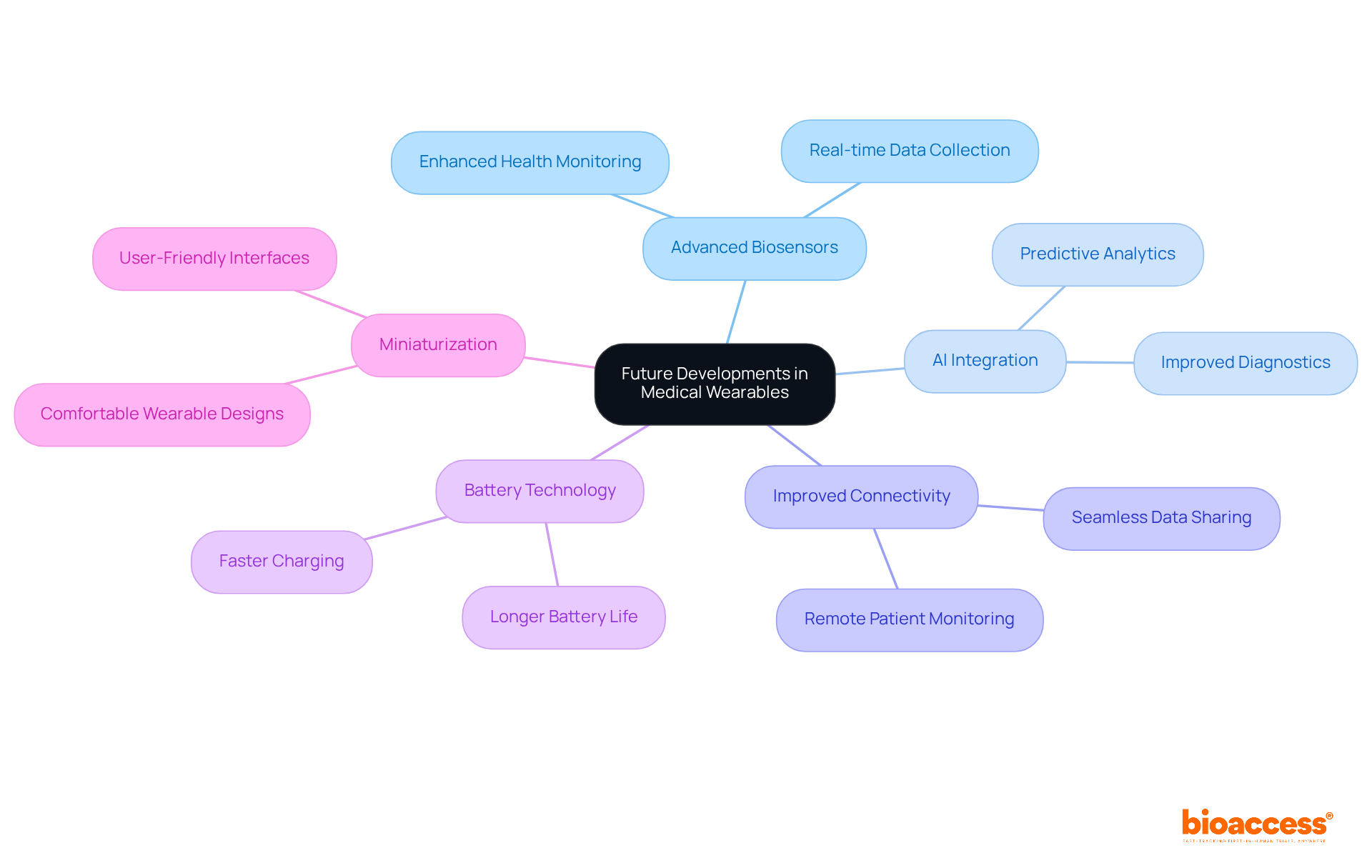
The future of medical wearables in portable technology within healthcare is undeniably promising. Innovations such as advanced biosensors, AI integration, and improved connectivity are on the horizon. These advancements are set to enhance device functionalities, enabling more precise wellness tracking and tailored support.
For instance, the incorporation of AI facilitates predictive analytics, empowering devices to provide users with insights into potential health risks derived from their data. Furthermore, breakthroughs in battery technology and miniaturization will yield devices that are not only more comfortable but also user-friendly.
As these innovations emerge, they will significantly reshape the landscape of medical care and individual health management through the use of medical wearables.
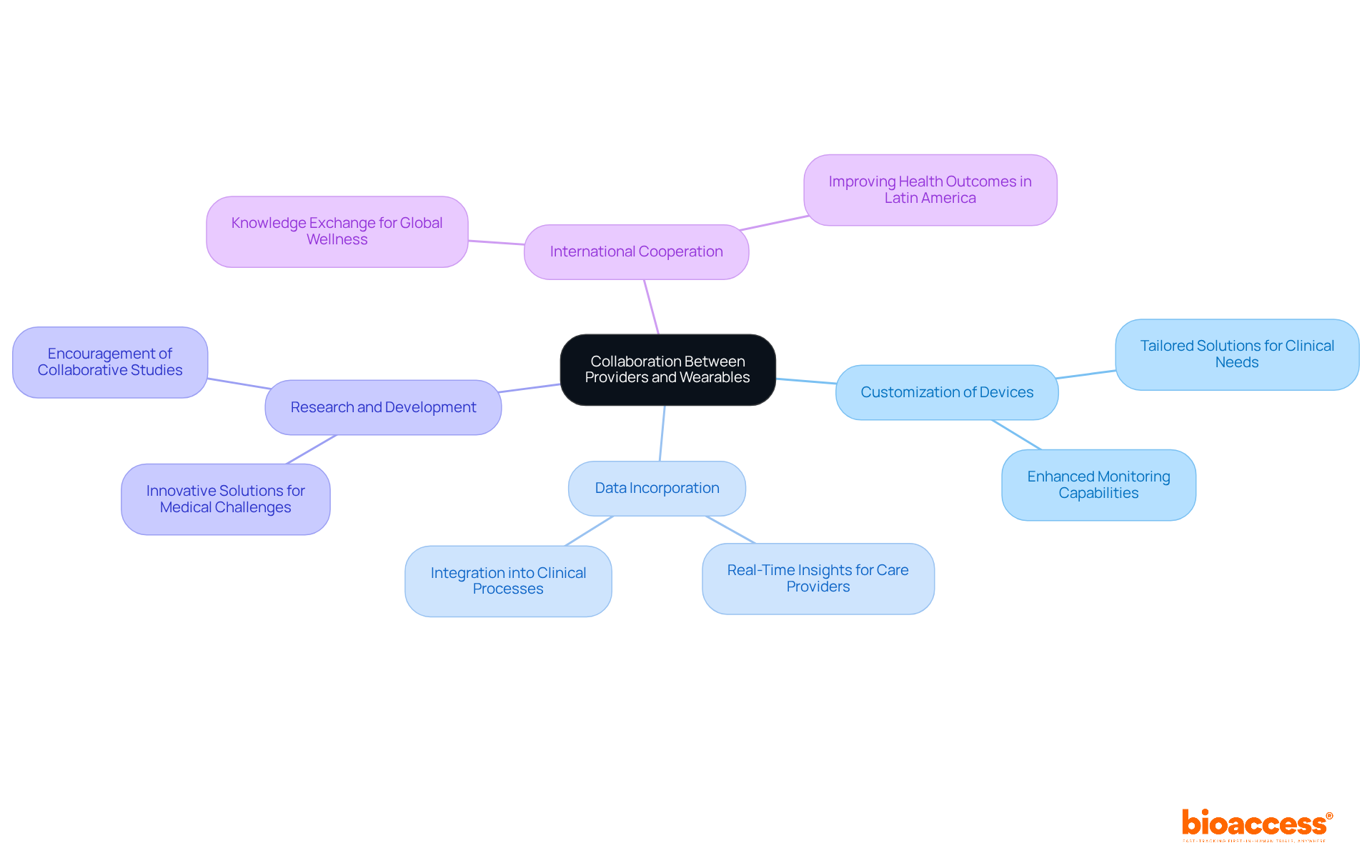
Cooperation among medical practitioners and device creators is essential for enhancing outcomes for individuals. By coordinating their efforts, these stakeholders can ensure that monitoring devices are customized to address clinical needs, resulting in more effective solutions for managing and monitoring individuals.
Collaborations can facilitate the smooth incorporation of device data into clinical processes, enabling care providers to make knowledgeable choices based on real-time insights from individuals. Furthermore, joint efforts can encourage research and development, promoting innovative solutions that address particular medical challenges.
This synergy is crucial for unlocking the full potential of wearables in enhancing healthcare delivery and care for individuals. By fostering international cooperation and knowledge exchange, as bioaccess seeks to achieve, we can improve global wellness results and transform lives, particularly in regions such as Latin America.
Medical wearables are fundamentally transforming care for individuals by enabling continuous monitoring of well-being, facilitating early detection of medical issues, and empowering people to take charge of their wellness. This integration significantly enhances medical providers' ability to deliver individualized care, improving client outcomes.
For instance, smartwatches equipped with heart rate monitors can detect irregularities such as atrial fibrillation, allowing for timely interventions. As technology progresses, its impact on medical services will continue to grow, promoting a proactive and patient-focused strategy for wellness management.
Notably, 88% of doctors favor individuals tracking wellness metrics at home, highlighting the increasing acceptance of devices in clinical practice. By embracing portable technology, medical systems can enhance their capabilities, effectively meeting the needs of patients in a digital environment.
The global market for medical wearables, which was valued at $33.85 billion in 2023, is projected to reach $250 billion by 2030, indicating a significant transition towards digital wellness solutions. This trend is further supported by the COVID-19 pandemic, which accelerated the adoption of medical wearables for health monitoring and managing chronic conditions, demonstrating their vital role in modern healthcare delivery.
![]()
Medical wearables are fundamentally transforming clinical research and patient care by delivering innovative solutions that enhance monitoring, empower individuals, and streamline healthcare processes. Their integration into medical systems significantly boosts patient engagement and facilitates timely interventions and personalized treatment plans, ultimately leading to improved health outcomes.
Key insights have emerged regarding the multifaceted benefits of wearable technology:
The importance of medical wearables in contemporary healthcare is immense. As the market continues to expand, embracing these technologies is crucial for enhancing patient care and outcomes. Stakeholders must foster innovation, prioritize data security, and focus on user-friendly designs to ensure the transformative potential of wearables is fully realized. By taking these steps, the future of healthcare can evolve into a more connected, proactive, and patient-centered system.
What is bioaccess® and how does it facilitate clinical research for medical wearables?
bioaccess® is a company that leverages its extensive experience in early-phase clinical research to facilitate the rapid integration of medical devices into clinical trials. It capitalizes on Latin America's regulatory efficiency and diverse patient populations, particularly in Colombia, to secure ethical approvals in just 4-6 weeks, significantly accelerating the timeline for technology studies.
What advantages does Colombia offer for clinical trials of medical wearables?
Colombia offers a cost-saving advantage exceeding 30% compared to trials in North America or Western Europe, along with a robust medical system ranked among the best globally. This not only expedites market entry for medical wearables but also improves outcomes for individuals and invigorates local economies through job creation and advancements in medical services.
How do medical wearables enhance real-time patient monitoring?
Medical wearables enable continuous real-time monitoring of individuals, allowing medical professionals to track vital signs, activity levels, and other health metrics. This capability enhances healthcare by enabling timely interventions and personalized treatment plans, ultimately improving safety and patient outcomes.
What impact does Remote Health Monitoring (RPM) have on healthcare costs and patient outcomes?
Research indicates that RPM can reduce hospital readmissions by up to 76% and decrease the length of stay for chronic patients by 25%. Additionally, RPM programs can help providers save approximately $1,000 per individual annually, highlighting the financial benefits of these technologies.
How does the integration of medical wearables into clinical workflows benefit healthcare professionals?
The integration of medical wearables into clinical workflows ensures that healthcare professionals have immediate access to critical information, fostering a proactive approach to health management. Continuous monitoring empowers individuals and enhances adherence to treatment plans, with studies showing RPM can increase engagement by as much as 80%.
What ethical and privacy concerns are associated with medical wearables?
Ethical and privacy concerns surrounding data use in predictive analytics are essential to address, as these issues could affect the widespread acceptance of monitoring devices in healthcare.
How do portable devices improve patient management within healthcare systems?
Portable devices enhance individual management by ensuring that information gathered is seamlessly integrated into electronic medical records (EMRs). This integration allows medical providers to access extensive individual data, facilitating improved decision-making and coordinated care.
What is the role of interoperability between wearables and healthcare systems?
Interoperability between wearables and healthcare systems boosts the overall efficiency of individual management, resulting in better wellness outcomes and reducing the administrative load on medical personnel, allowing them to focus more on patient care.