


The article delineates best practices for ensuring quality assurance and compliance in clinical research, underscoring the critical necessity of systematic procedures, effective documentation, and regular audits. It elaborates on strategies such as:
Collectively, these strategies not only enhance the integrity and credibility of clinical trials but also prioritize the welfare of participants.
Quality assurance and compliance serve as the backbone of clinical research, ensuring that studies not only meet rigorous standards but also protect the rights and welfare of participants. As the landscape of medical research evolves, understanding and implementing best practices in these areas becomes increasingly critical for success. However, with the complexities of regulations and the potential consequences of non-compliance, research teams must navigate this intricate terrain effectively to achieve both ethical and operational excellence.
Quality assurance and compliance in medical research encompasses systematic procedures designed to ensure that studies adhere to established standards, regulations, and protocols. Quality assurance and compliance involve strict adherence to these regulations and guidelines set forth by oversight bodies such as the FDA and the International Council for Harmonisation (ICH). Together, quality assurance and compliance with regulatory standards are vital for ensuring that medical studies are not only effective but also ethical, safeguarding the rights and welfare of participants while preserving the integrity of the data collected.
As a leading contract research organization (CRO) in Latin America, bioaccess® excels at navigating the complex compliance landscape, providing tailored solutions for medtech startups. The organization’s comprehensive research study management services include:
This expertise is crucial for maintaining high standards in research trials, particularly in an environment where quality assurance and compliance demands can vary significantly. Notably, bioaccess® has achieved ACRP certification, underscoring its commitment to excellence in clinical research.
The significance of quality assurance and compliance is underscored by the fact that non-compliance can lead to severe repercussions, including costly delays and regulatory penalties. For example, a Phase III oncology study faced rejection from the FDA due to Good Clinical Practice (GCP) violations, leading to millions of dollars in additional costs for the sponsor. Furthermore, each data request in medical studies incurs an average expense of $150, illustrating the financial implications of inadequate QA procedures.
Effective quality management plans (QMPs) are essential for maintaining quality assurance and compliance with high standards in clinical studies. A notable case involves a biotech firm that implemented risk-based monitoring (RBM) in a multi-site cardiovascular study, focusing on high-risk areas and reducing expenses by 30% while preserving data accuracy. This approach demonstrates how structured quality assurance and compliance can enhance procedural efficiency.
In conclusion, understanding the significance of quality assurance and compliance is crucial for all stakeholders involved in research, as these elements lay the foundation for effective management and execution. Additionally, the impact of medtech clinical research extends beyond individual studies, contributing to local economies through job creation, economic growth, and improved healthcare outcomes, further emphasizing the importance of rigorous quality assurance and compliance as well as regulatory practices.

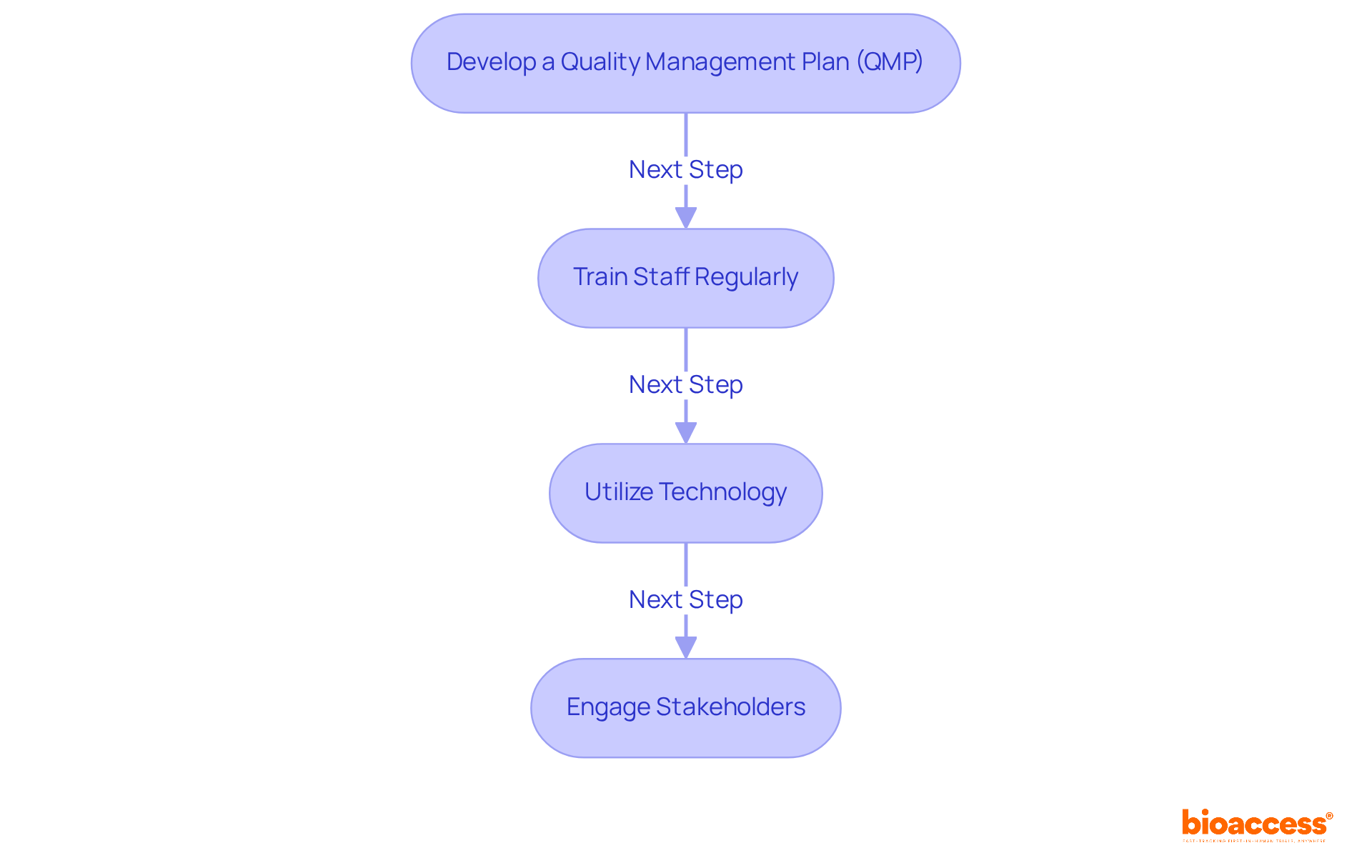
To implement effective quality assurance and compliance practices, research teams should consider the following strategies:
Develop a Quality Management Plan (QMP): A comprehensive QMP is crucial for outlining processes and procedures that ensure quality throughout the trial lifecycle. It should encompass risk management strategies, monitoring plans, and clearly defined roles and responsibilities. The establishment of a governance structure for quality metrics can facilitate continuous improvement and adaptation to evolving standards.
Train Staff Regularly: Ongoing education and training for all team members on compliance requirements and best practices are essential. Research indicates that regular training significantly enhances staff competency and confidence, with programs like the Mayo Clinic Clinical Research Orientation Program (MCCRO) demonstrating substantial knowledge gains among participants. Nearly 1300 professionals have completed this program, highlighting its effectiveness in improving operational efficiencies.
Utilize Technology: Leveraging electronic data capture (EDC) systems and other digital tools can streamline data collection and monitoring processes. These technologies not only improve data precision but also enable real-time regulatory checks. A study found that 65% of sites utilized centralized monitoring methods, indicating a trend towards technology-driven quality management.
Engage Stakeholders: Fostering open communication with all stakeholders, including sponsors, regulatory bodies, and ethics committees, is vital. Frequent updates and conversations can assist in recognizing possible regulatory issues early on. Engaging stakeholders in the quality assurance and compliance process ensures that everyone is aligned with the trial's objectives and standards, ultimately resulting in improved outcomes.
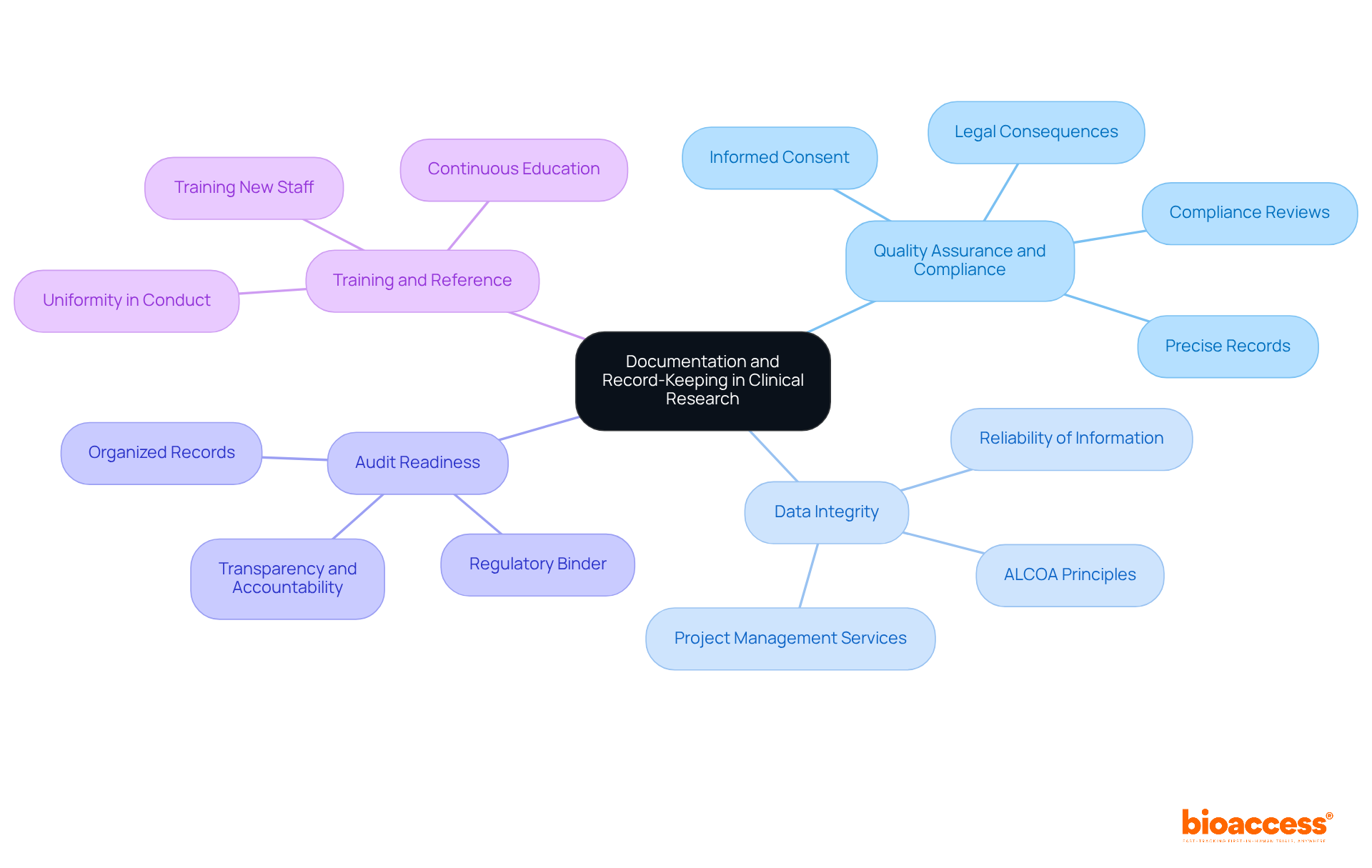
Effective documentation and record-keeping are essential in clinical research for several key reasons:
Quality assurance and compliance require keeping precise records, which is crucial for demonstrating conformity to legal requirements. This includes meticulous documentation of all trial-related materials, such as protocols, informed consent forms, and case report forms, which are vital during audits and inspections. Regulatory agencies stress that incomplete documentation can result in considerable legal consequences, including fines and approval revocation. Furthermore, acquiring informed consent from participants is a vital element of adherence to regulations, safeguarding their rights and privacy. Services such as those provided by bioaccess, including compliance reviews, feasibility studies, and setup for testing, ensure quality assurance and compliance by meeting country-specific documentation requirements and further enhancing regulatory adherence.
Data Integrity: Proper documentation protects the reliability of information gathered during tests, ensuring it can be verified and trusted. This integrity is essential for the credibility of research outcomes, as precise records enable the reconstruction of event occurrences and support informed decision-making. Adhering to the ALCOA principles (Attributable, Legible, Contemporaneous, Original, Accurate) and the ALCOA+ enhancements (Complete, Consistent, Enduring, Available) is essential for ensuring data integrity. bioaccess’s project management services assist in upholding these standards throughout the testing process.
Audit Readiness: Organized and thorough records equip research teams for audits by oversight bodies. A properly cared for regulatory binder not only aids in a smoother audit process but also improves transparency and accountability, which are essential for preserving the integrity of research studies. Regular audits and monitoring are vital for ensuring quality assurance and compliance by identifying and rectifying non-compliance issues, thereby meeting ethical considerations. Clear filing systems and document control procedures, as emphasized in bioaccess’s study project management, are necessary for facilitating audits effectively.
Training and Reference: Documentation serves as a valuable resource for training new staff and providing reference material for ongoing studies. It guarantees uniformity in conduct and adherence to protocols, emphasizing the significance of comprehensive training on documentation practices. Continuous training and education for research staff are essential to guarantee adherence to changing regulations, as the area of medical investigation keeps progressing. bioaccess’s comprehensive services include training support, ensuring that all personnel are well-versed in documentation practices and regulatory requirements.
By prioritizing these aspects of documentation and record-keeping, research organizations can improve their adherence efforts, ultimately contributing to the advancement of medical knowledge and the safety of trial participants.
Conducting regular audits and inspections is essential for enhancing quality assurance and compliance in clinical research. To ensure effective oversight, consider the following key steps:
Establish an Audit Schedule: Develop a systematic schedule for internal audits to evaluate adherence to protocols and regulatory standards. This should encompass both announced and unannounced audits, ensuring comprehensive assessments.
Utilize Checklists: Create detailed audit checklists that cover all critical aspects of the study, including documentation, data management, and participant safety. This approach guarantees that every vital area is systematically reviewed.
Engage Independent Auditors: Employ third-party auditors to provide an impartial assessment of adherence. Independent assessments can reveal issues that internal teams might overlook, thereby enhancing the overall quality of the audit process.
Implement Corrective Actions: After audits, swiftly address any identified issues through corrective action plans. This not only demonstrates a commitment to continuous improvement but also fosters a culture of accountability within the research team.
Regular audits are vital for quality assurance and compliance, ensuring not only adherence to standards but also contributing to the integrity and credibility of clinical trials. Ultimately, they safeguard participant safety and enhance data quality.

Quality assurance and compliance serve as foundational pillars in clinical research, ensuring that studies adhere to established standards and regulations. By systematically implementing best practices, research teams not only enhance the integrity of their findings but also safeguard the rights and welfare of participants involved in clinical trials. This commitment to quality assurance and compliance transcends mere regulatory obligation; it embodies a pledge to uphold the highest ethical standards in the pursuit of medical advancements.
The article delineates several key strategies for achieving effective quality assurance and compliance, such as:
Furthermore, it underscores the critical importance of meticulous documentation and record-keeping in maintaining compliance and ensuring data integrity. Regular audits and inspections reinforce these practices, fostering a culture of accountability and continuous improvement within research teams.
Ultimately, the significance of quality assurance and compliance extends beyond individual studies; it contributes to the broader landscape of medical research, driving innovation and enhancing healthcare outcomes. As the field evolves, embracing these best practices becomes essential for researchers, stakeholders, and organizations alike. By prioritizing quality assurance and compliance, the clinical research community can ensure that the pursuit of knowledge is conducted with integrity, ultimately benefiting society as a whole.
What is quality assurance and compliance in clinical research?
Quality assurance and compliance in clinical research refer to systematic procedures that ensure studies adhere to established standards, regulations, and protocols set by oversight bodies like the FDA and ICH.
Why are quality assurance and compliance important in medical studies?
They are vital for ensuring that medical studies are effective and ethical, safeguarding the rights and welfare of participants while preserving the integrity of the data collected.
What services does bioaccess® provide related to quality assurance and compliance?
Bioaccess® offers services such as feasibility assessments, site selection, compliance evaluations, study setup, import permits, project oversight, and reporting.
What certification has bioaccess® achieved to demonstrate its commitment to clinical research?
Bioaccess® has achieved ACRP certification, highlighting its dedication to excellence in clinical research.
What can happen if there is non-compliance in clinical research?
Non-compliance can lead to severe repercussions, including costly delays and regulatory penalties, such as the rejection of studies by the FDA due to Good Clinical Practice violations.
How do inadequate quality assurance procedures impact costs in medical studies?
Each data request in medical studies incurs an average expense of $150, illustrating the financial implications of inadequate quality assurance procedures.
What is a quality management plan (QMP) and why is it important?
A quality management plan (QMP) is essential for maintaining high standards of quality assurance and compliance in clinical studies, helping to manage risks and enhance procedural efficiency.
Can you provide an example of effective quality assurance in clinical research?
A biotech firm implemented risk-based monitoring (RBM) in a multi-site cardiovascular study, focusing on high-risk areas and reducing expenses by 30% while preserving data accuracy.
How does quality assurance and compliance impact local economies?
The impact of medtech clinical research extends beyond individual studies, contributing to local economies through job creation, economic growth, and improved healthcare outcomes.