


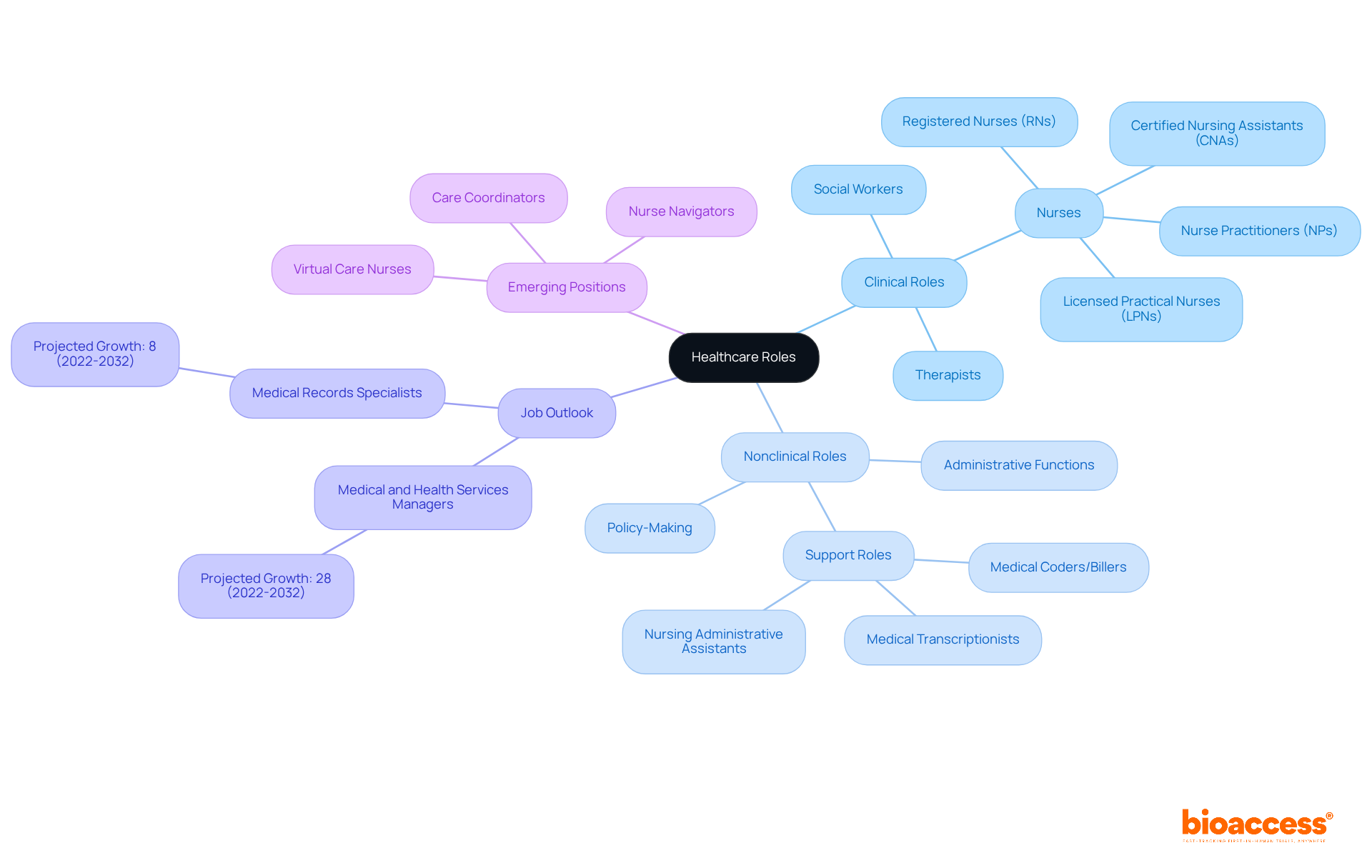
The article delineates the critical distinctions between clinical and nonclinical roles within healthcare. It asserts that clinical roles are primarily focused on direct patient care, whereas nonclinical roles are centered around administrative and support functions. This distinction is reinforced by illustrating the increasing demand for nonclinical positions, such as policy analysis and program management, alongside the indispensable responsibilities of clinical professionals. Such insights underscore the dynamic and evolving landscape of healthcare careers.
The healthcare industry is undergoing a profound transformation as the distinction between clinical and nonclinical roles becomes increasingly pronounced.
This article examines the key differences between clinical and nonclinical definitions, elucidating how each sector uniquely contributes to patient outcomes and healthcare efficiency.
As the demand for both types of professionals escalates, understanding these distinctions prompts a critical question: how can individuals effectively navigate their career paths in an evolving healthcare landscape?
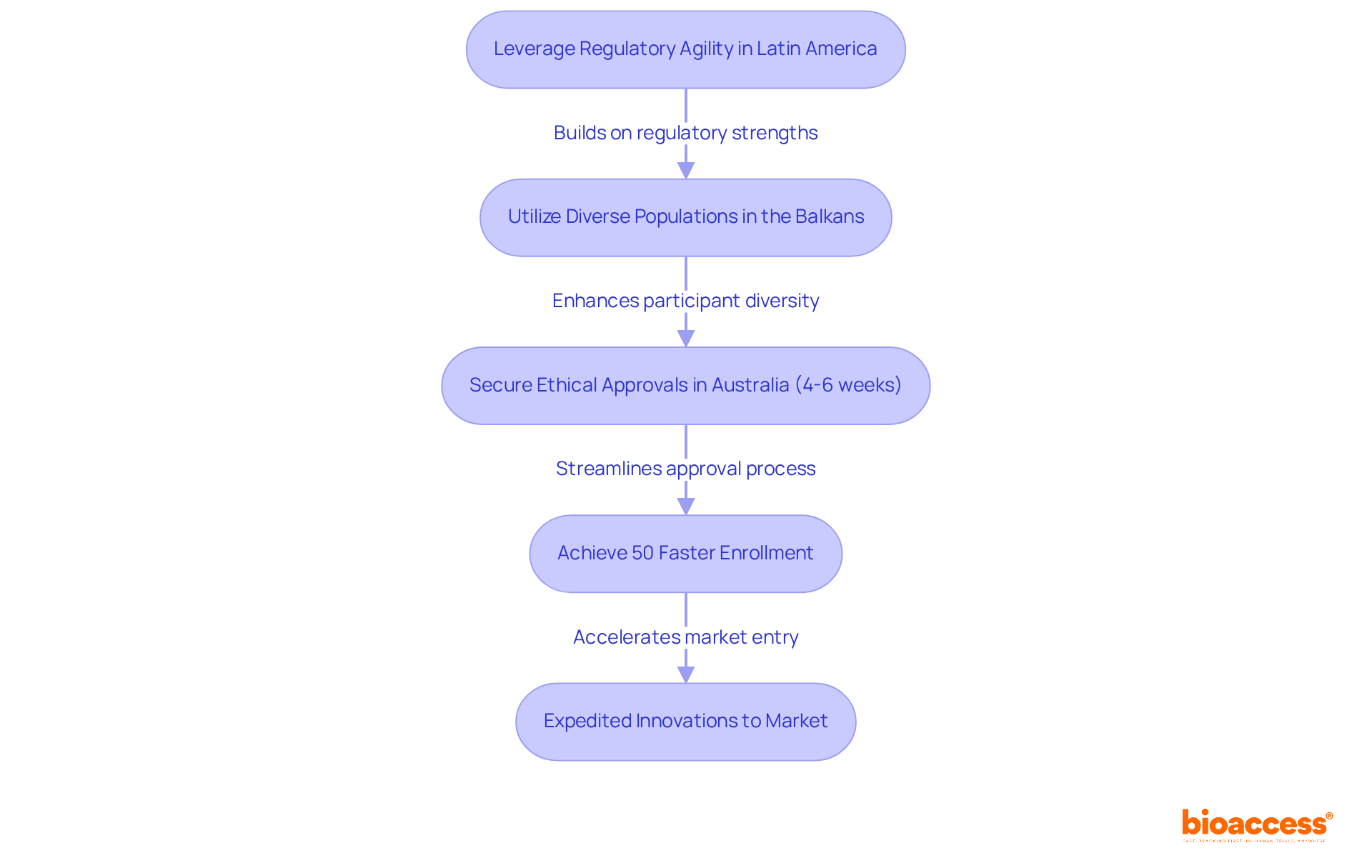
bioaccess® stands at the forefront of accelerating clinical research for Medtech innovations, leveraging the regulatory agility of Latin America, the diverse populations of the Balkans, and the efficient ethical approval processes in Australia. This strategic approach facilitates the securing of ethical approvals within a remarkable timeframe of just 4-6 weeks, achieving enrollment rates that are 50% faster than those in traditional markets. By concentrating on early-phase studies, bioaccess® empowers Medtech companies to expedite their innovations to market, ensuring that individuals gain access to groundbreaking technologies sooner than ever before.
This efficiency not only enhances outcomes for individuals but also significantly reduces expenses, with potential savings of $25K per individual when utilizing FDA-ready data. As the landscape of research trials evolves, the emphasis on regulatory speed and participant engagement becomes increasingly critical, underscoring bioaccess®'s pivotal role in transforming the Medtech sector. The importance of collaboration and strategic partnerships cannot be overstated, as they are essential for navigating the complexities of clinical research and delivering innovative solutions that meet the needs of patients and healthcare providers alike.
Healthcare roles encompass direct individual care and treatment, typically necessitating specific licensure and training, exemplified by social workers who offer therapy and counseling. In contrast, the clinical and nonclinical definition indicates that nonclinical roles prioritize administrative, policy-making, or support functions devoid of direct patient interaction.
As of 2025, a considerable segment of healthcare professionals operates in nonclinical capacities, highlighting a burgeoning trend toward administrative and support roles within the industry. Notably, the job outlook for medical and health services managers is projected to grow by 28% between 2022 and 2032, underscoring the escalating importance and demand for nonclinical roles in healthcare.
Emerging positions such as virtual care nurses, care coordinators, and nurse navigators illustrate the evolving landscape of both medical and nonmedical roles. Understanding the clinical and nonclinical definition of these distinctions is crucial for professionals in the field to effectively align their skills and career aspirations.
Transitioning from clinical to nonclinical roles is generally straightforward due to existing knowledge of administrative systems, which can facilitate career mobility. This expertise not only supports personal career development but also enhances the overall efficiency of healthcare delivery by ensuring that individuals are positioned in roles that best suit their expertise and interests.
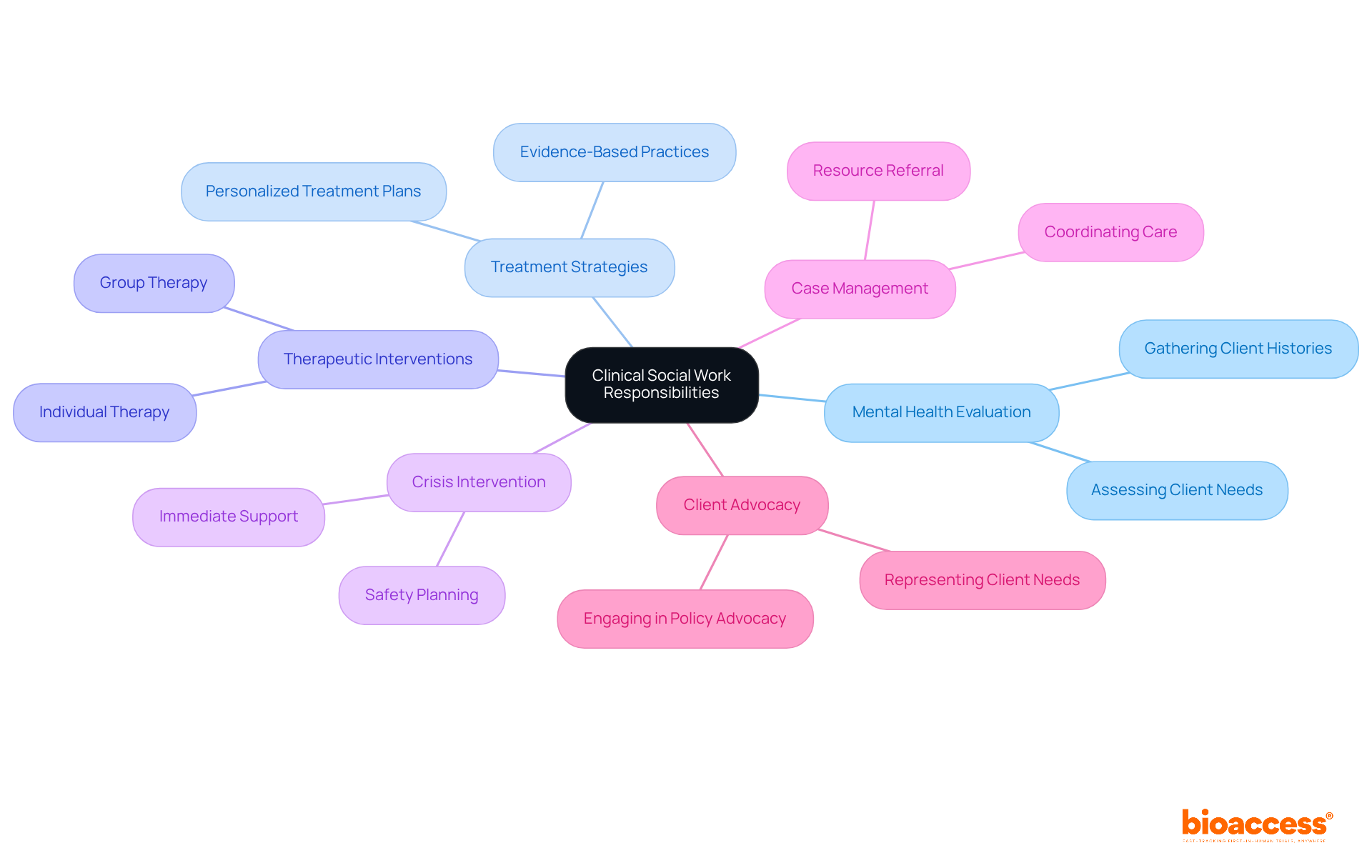
Clinical counselors are pivotal in the healthcare landscape, tasked with evaluating individuals' mental health needs, formulating tailored treatment strategies, and delivering therapeutic interventions. Operating across a spectrum of environments, including hospitals, clinics, and private practices, they work in close collaboration with other healthcare professionals to ensure comprehensive care. Their role encompasses not only therapy but also crisis intervention, case management, and client advocacy, highlighting their essential function within the healthcare team.
As we look towards 2025, healthcare professionals are expected to adeptly manage complex patient situations, employing evidence-based practices to enhance treatment outcomes. Effective treatment plans typically integrate thorough assessments of clients' histories, strengths, and cultural contexts, ensuring that interventions are both personalized and pertinent.
As one expert aptly stated, 'There is no 'one size fits all' plan for therapy — no two treatment plans or clients are the same.' This adaptability is vital in meeting the unique challenges faced by individuals, ultimately promoting improved mental health and well-being.
Furthermore, the National Association of Social Workers underscores the necessity of cultural competence during assessments, which is critical for delivering effective care. With a median salary of $62,940 in 2023, therapists find themselves in a profession that demands high ethical standards while also offering a rewarding career path.
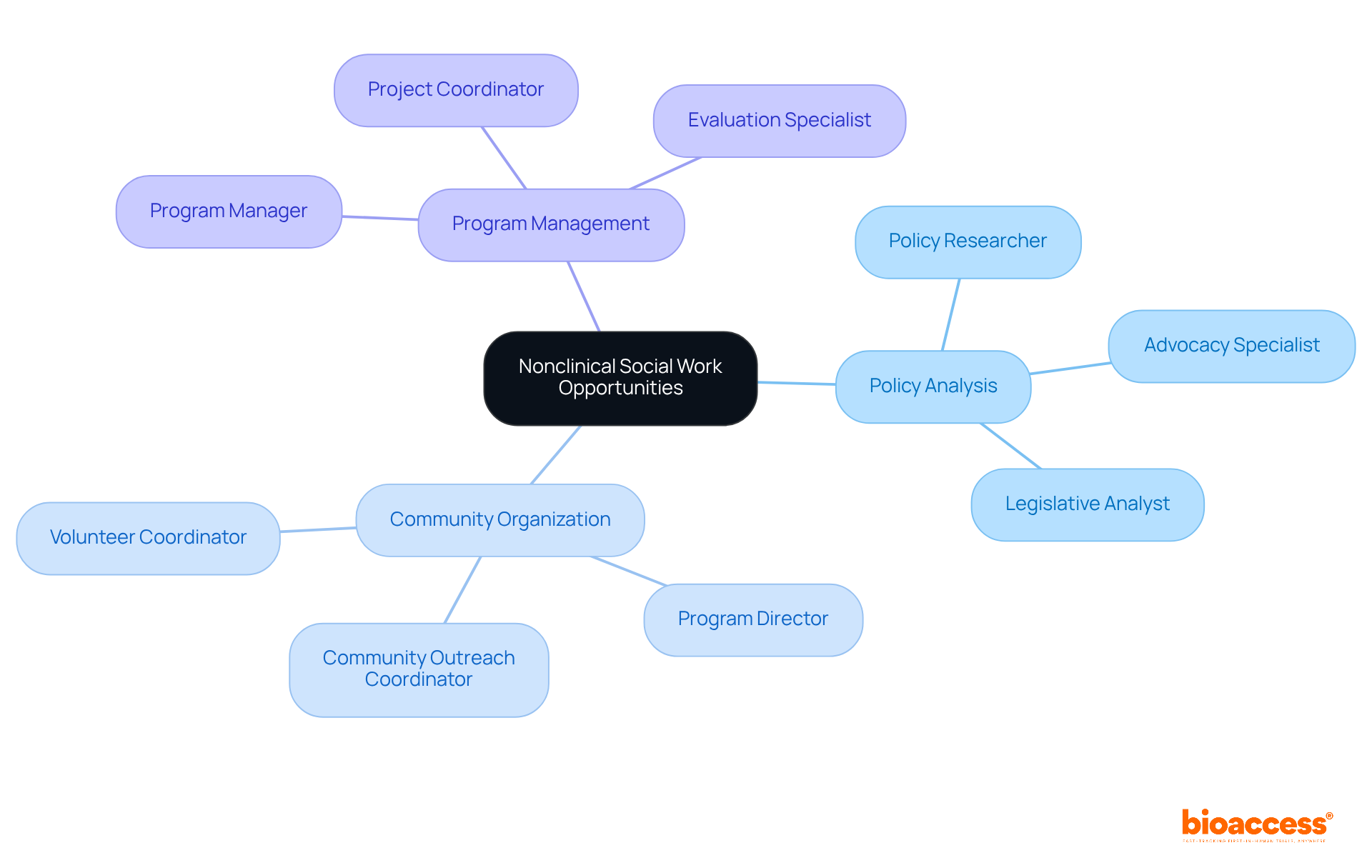
Nonclinical professionals assume pivotal roles that underscore policy development, program management, and community outreach. Operating within government agencies, non-profit organizations, or educational institutions, they tackle systemic issues such as poverty, housing, and access to healthcare. Their contributions are essential for fostering supportive environments that enhance community well-being, thereby reinforcing the importance of their work in the broader context of public health.

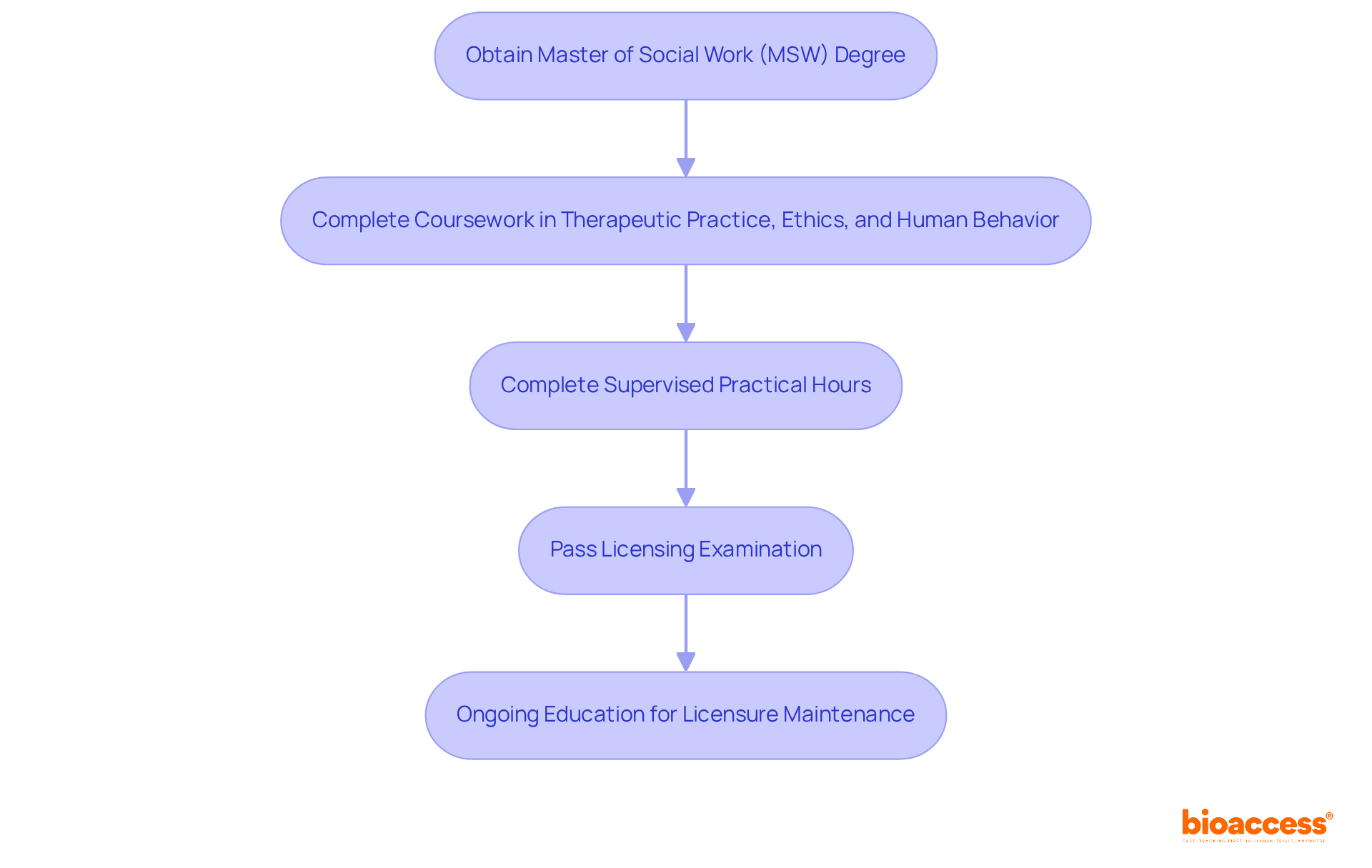
Pursuing a profession as a healthcare practitioner in support services typically necessitates obtaining a Master of Social Work (MSW) degree. This degree encompasses essential coursework in therapeutic practice, ethics, and human behavior. As of 2025, the average duration to complete an MSW program is around two years, though this timeline may fluctuate depending on the institution and whether the student opts for full-time or part-time enrollment. Upon earning their degree, candidates are required to complete a specified number of supervised practical hours, providing invaluable real-world experience in the field. Subsequently, they must successfully pass a licensing examination to practice as a therapist.
Ongoing education is vital for maintaining licensure and ensuring practitioners remain informed about evolving best practices and regulatory changes. Academic leaders emphasize the significance of MSW programs in equipping graduates to tackle the challenges of practice, asserting that these programs furnish students with the critical skills necessary to effectively address diverse client needs. The journey to becoming a clinical counselor represents not only a commitment to education but also a pledge to continuous professional development, guaranteeing that practitioners are well-equipped to deliver high-quality support to individuals and communities.
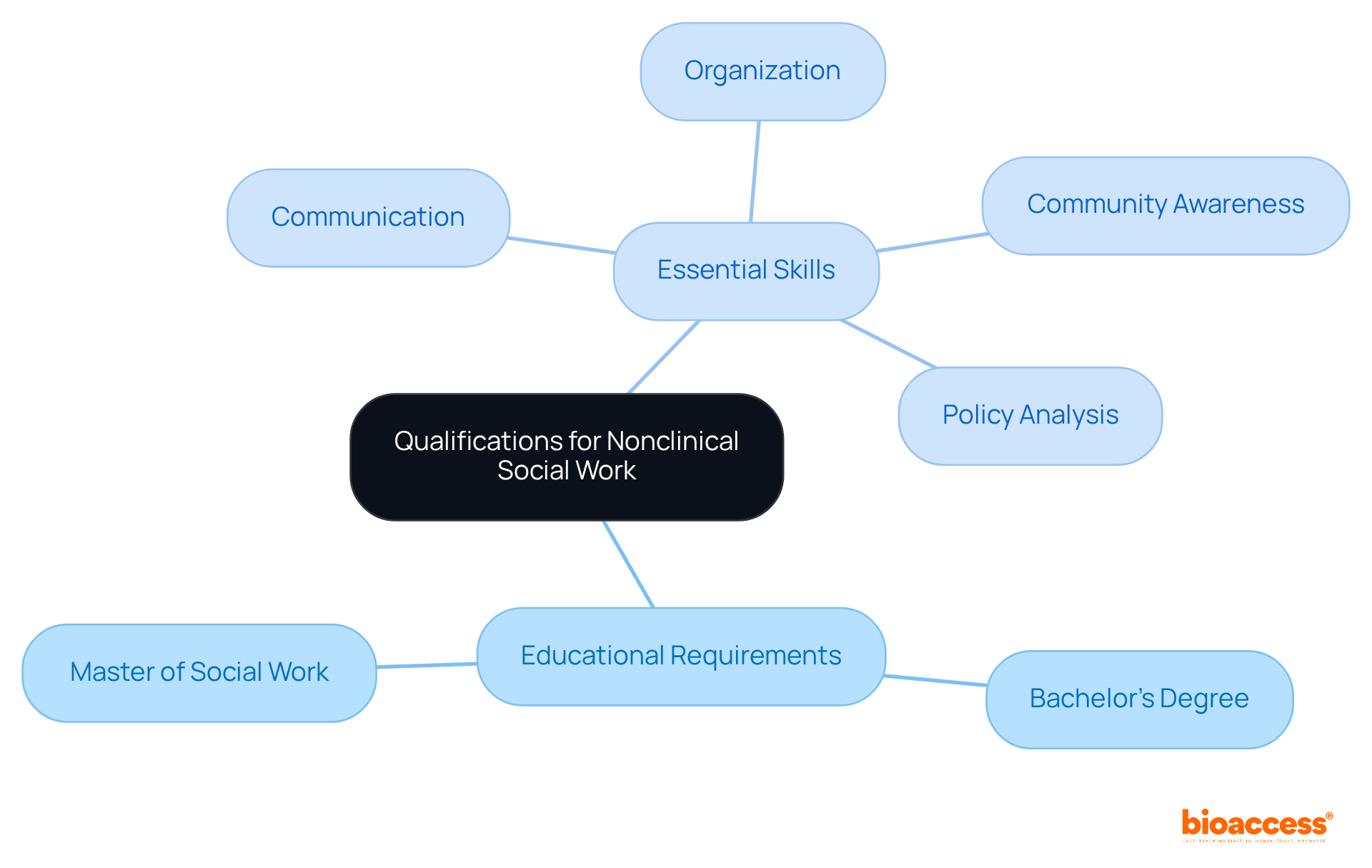
Nonclinical community work positions often require a Bachelor’s degree in social work or a related field; however, many roles may prefer or necessitate a Master of Social Work (MSW). Essential skills include:
Additionally, having a strong awareness of community resources and advocacy strategies is advantageous for effectively addressing societal issues.
Clinical counselors operate within a stringent regulatory framework that includes HIPAA mandates for individual privacy alongside various state licensing requirements. The landscape is further complicated by evolving healthcare policies, reimbursement challenges, and the necessity for continuous training to ensure compliance.
For instance, HIPAA compliance is paramount in healthcare settings, where safeguarding individual information is crucial. Violations can result in severe consequences, including fines and damage to professional credibility. Compliance officers stress the significance of comprehending these regulations to adeptly navigate the complexities of healthcare.
As we approach 2025, the impact of HIPAA on therapeutic practices continues to expand, necessitating a proactive approach to training and policy adjustments. This ongoing commitment to compliance not only protects individual privacy but also enhances the quality of care delivered.

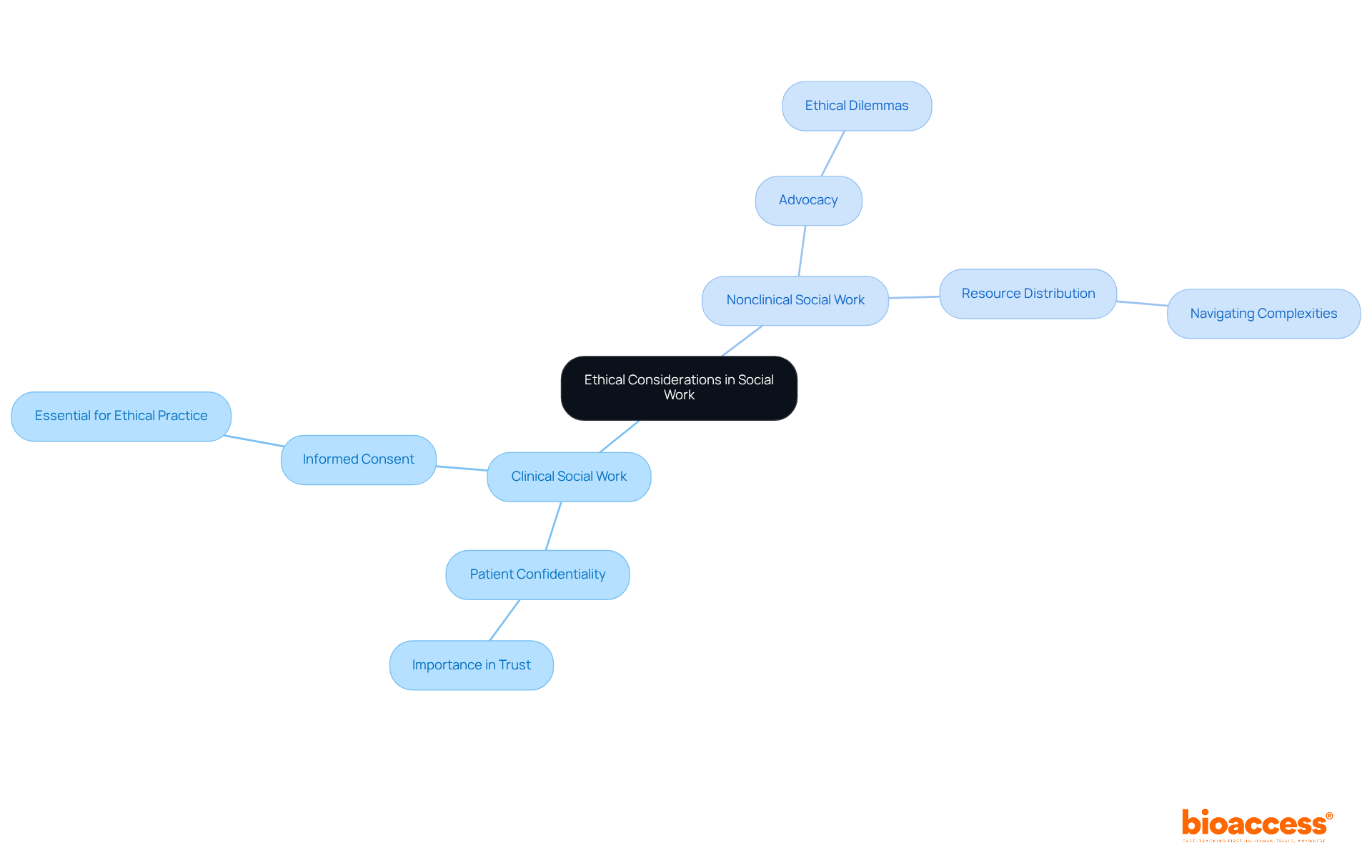
Both therapeutic and non-therapeutic practitioners face ethical challenges that require thoughtful reflection. Clinical professionals must prioritize patient confidentiality and informed consent, essential components in maintaining trust within the profession. Meanwhile, nonclinical practitioners often navigate ethical dilemmas related to advocacy and resource distribution, highlighting the complexity of their roles.
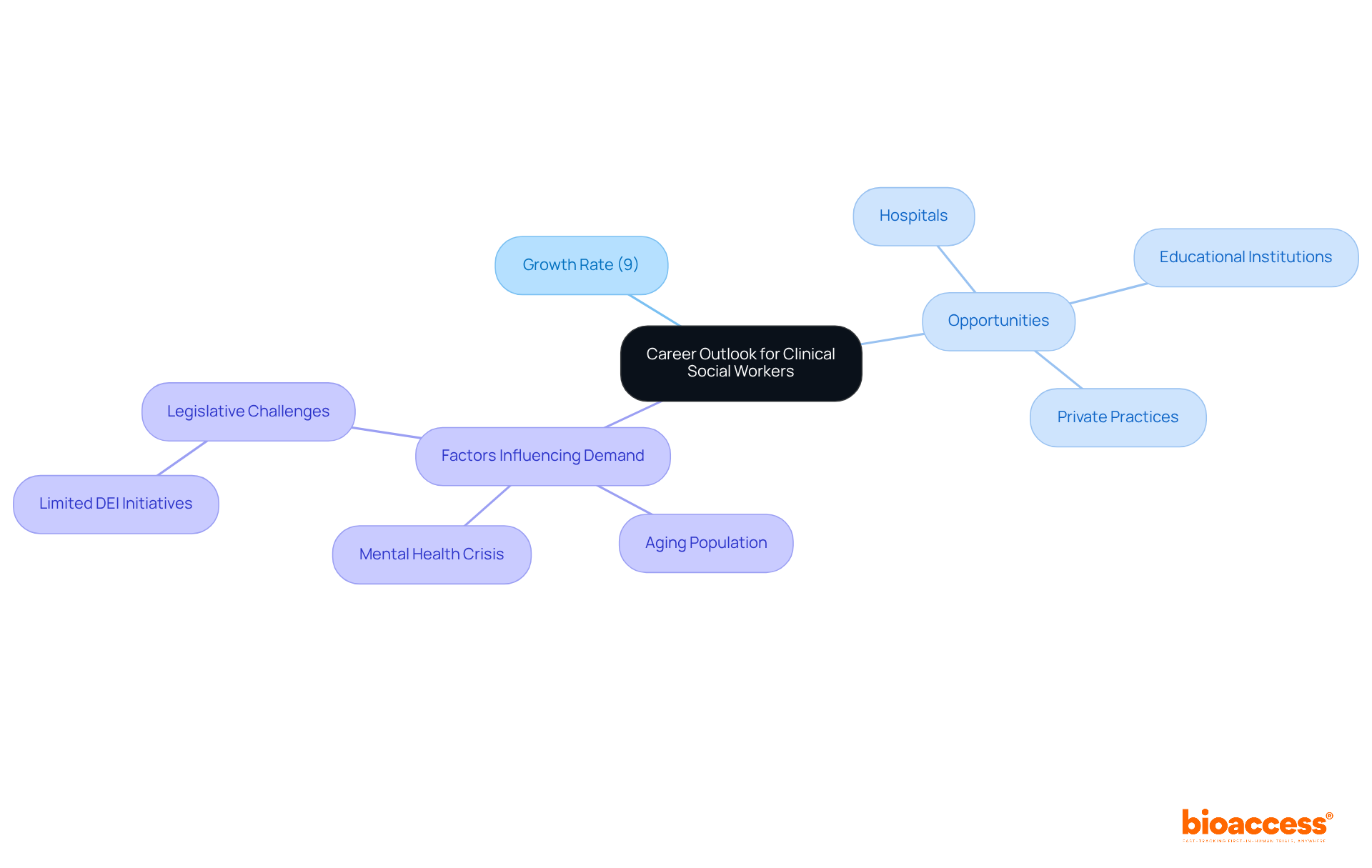
The career prospects for clinical practitioners are exceptionally promising, with the Bureau of Labor Statistics forecasting a robust growth rate of 9% from 2021 to 2031. This surge in demand is primarily due to an increased awareness of mental health issues and the urgent need for qualified professionals to provide essential care.
As Alyssa Payne, Application Advisor at MSW Helper, emphasizes, "The world requires more individuals in the helping profession, not fewer, particularly in times like these."
Clinical practitioners can explore opportunities across various settings, including:
Furthermore, the case study titled "Sustained and Growing Demand for Practitioners in the Community" highlights that demographic trends, such as an aging population and a worsening mental health crisis, are intensifying the demand for professionals in this field.
As the mental health crisis continues to escalate, the necessity for skilled practitioners is more critical than ever, ensuring a consistent influx of job openings and career advancement opportunities.
To delve deeper into these prospects, aspiring community service professionals should consider researching local MSW programs and job boards to stay informed about the evolving landscape of their field.
The job market for nonclinical human services is thriving, particularly in areas such as policy analysis, community organization, and program management. Government agencies and non-profit organizations are actively seeking qualified candidates, reflecting a robust demand for expertise in these sectors. As community issues grow increasingly complex, the necessity for skilled nonclinical workers to tackle these challenges is expected to rise significantly. This trend underscores the evolving landscape of social work, where nonclinical roles are becoming essential in shaping effective policies and community initiatives.
The distinctions between clinical and nonclinical roles in healthcare are vital for understanding the diverse landscape of the profession. Clinical roles focus on direct patient care, necessitating specialized training and licensure, while nonclinical roles emphasize administrative, policy-making, and support functions that do not involve direct patient interaction. Recognizing these differences is essential for professionals navigating their career paths and aligning their skills with the needs of the industry.
Key insights throughout the article highlight the growing demand for both clinical and nonclinical positions. Clinical social workers play a crucial role in evaluating and addressing mental health needs, while nonclinical professionals contribute to systemic change through policy development and community outreach. The projected growth in these fields underscores the importance of adapting to evolving healthcare landscapes and the necessity for ongoing education and compliance with regulatory standards.
In conclusion, the healthcare sector is increasingly recognizing the significance of both clinical and nonclinical roles. As the demand for skilled professionals continues to rise, individuals are encouraged to explore opportunities within both spheres. Whether pursuing a career in direct patient care or focusing on administrative and policy-driven roles, understanding the unique contributions of each path is essential for fostering a more effective and responsive healthcare system. Embracing this knowledge not only enhances personal career trajectories but also supports the broader goal of improving health outcomes for communities.
What is bioaccess® and what role does it play in clinical research for Medtech innovations?
bioaccess® accelerates clinical research for Medtech innovations by leveraging the regulatory agility of Latin America, diverse populations of the Balkans, and efficient ethical approval processes in Australia. This approach enables ethical approvals within 4-6 weeks and achieves enrollment rates that are 50% faster than traditional markets.
How does bioaccess® benefit Medtech companies?
By focusing on early-phase studies, bioaccess® helps Medtech companies expedite their innovations to market, allowing individuals to access groundbreaking technologies sooner. This efficiency can also lead to significant cost savings, potentially reducing expenses by $25K per individual when using FDA-ready data.
What is the significance of collaboration in clinical research according to bioaccess®?
Collaboration and strategic partnerships are essential for navigating the complexities of clinical research and delivering innovative solutions that meet the needs of patients and healthcare providers.
What are the core distinctions between clinical and nonclinical roles in healthcare?
Clinical roles involve direct patient care and treatment, requiring specific licensure and training, while nonclinical roles focus on administrative, policy-making, or support functions without direct patient interaction.
What is the job outlook for nonclinical roles in healthcare?
The job outlook for medical and health services managers is projected to grow by 28% between 2022 and 2032, indicating a rising demand for nonclinical roles within the healthcare industry.
How can professionals transition from clinical to nonclinical roles?
Transitioning from clinical to nonclinical roles is generally straightforward due to existing knowledge of administrative systems, which can facilitate career mobility and enhance overall healthcare delivery efficiency.
What are the key responsibilities of clinical social workers?
Clinical social workers evaluate mental health needs, create tailored treatment strategies, and provide therapeutic interventions. They also engage in crisis intervention, case management, and client advocacy, collaborating with other healthcare professionals for comprehensive care.
Why is cultural competence important in clinical social work?
Cultural competence is vital during assessments to deliver effective care, as it ensures that treatment plans are personalized and relevant to the unique challenges faced by individuals.
What is the median salary for clinical social workers in 2023?
The median salary for clinical social workers is $62,940 in 2023.