


The article delineates the concept of control trials, with a particular emphasis on randomized controlled trials (RCTs) and their historical context, underscoring their critical role in assessing the effectiveness of interventions. It elaborates on the meticulous design of RCTs, which effectively minimizes bias through randomization, thereby reinforcing their importance in producing reliable medical evidence. Furthermore, the article addresses the challenges inherent in conducting RCTs, such as participant recruitment, particularly among older adults, and the progressive evolution of ethical standards in research.
The realm of medical research is fundamentally anchored in rigorous testing and validation, with randomized controlled trials (RCTs) recognized as the gold standard for evaluating treatment efficacy. These meticulously designed experiments provide invaluable insights into the effectiveness of interventions while confronting significant challenges, particularly in participant recruitment among older adults.
As the landscape of clinical trials evolves, understanding the historical context and ethical considerations surrounding control trials becomes increasingly critical.
How can researchers ensure that these trials remain relevant and inclusive, all while upholding the integrity of their findings?
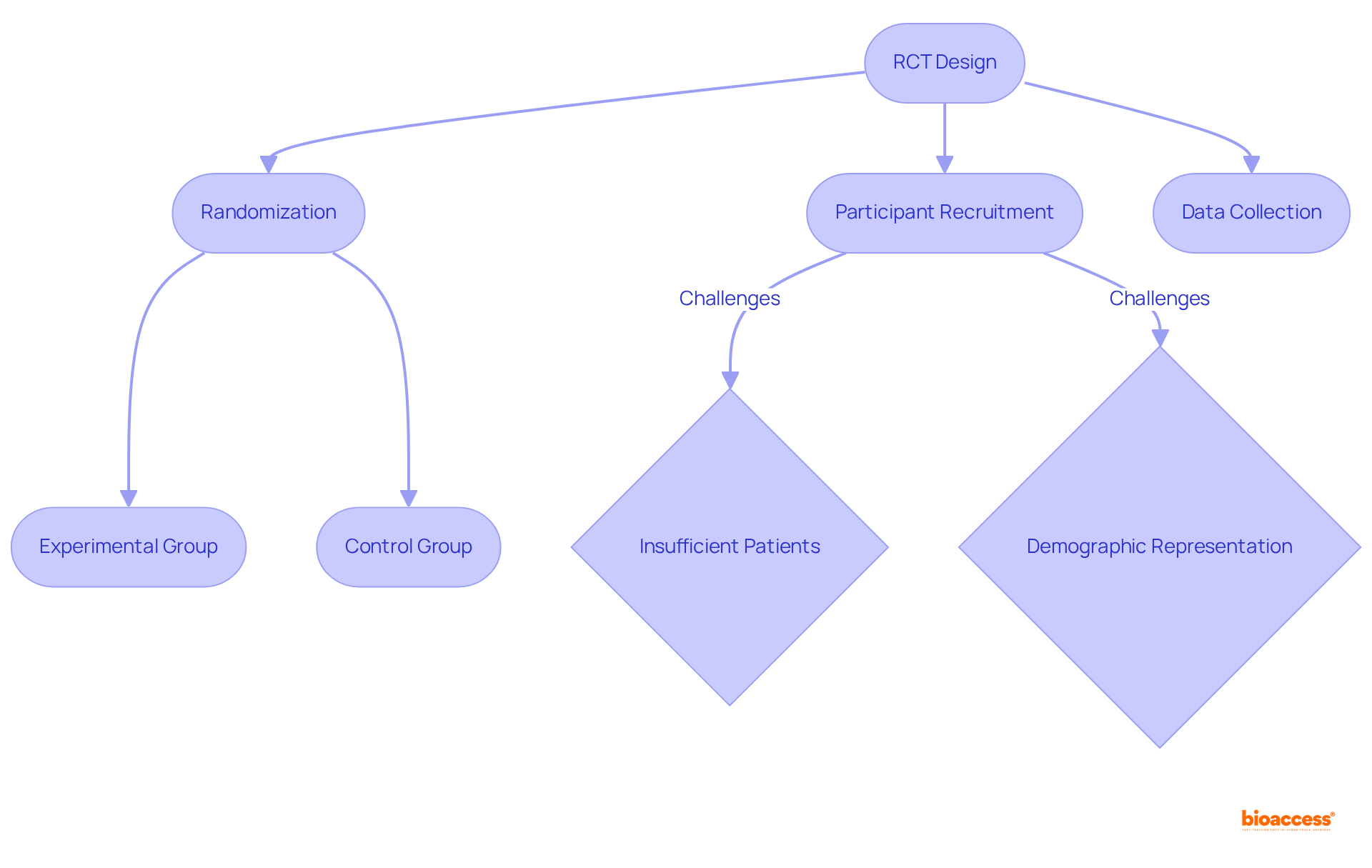
Randomized controlled studies (RCTs) are essential scientific experiments that illustrate the control trial definition, meticulously designed to evaluate the effectiveness of interventions by contrasting them with control groups. In these tests, participants are randomly assigned to either the experimental group, which receives the treatment, or the control group, which may receive a placebo or standard treatment. This randomization is vital as it mitigates bias, allowing researchers to attribute observed effects directly to the intervention rather than external influences.
The significance of RCTs is underscored by their capacity to provide high-quality evidence regarding the effectiveness and safety of new therapies, establishing them as a cornerstone of medical research. However, challenges persist; approximately 37% of research studies fail to recruit sufficient patients to proceed, with 11% not enrolling any participants at all. This issue is particularly pronounced among older adults, who are disproportionately affected by chronic illnesses. Over half of all cancers are diagnosed in individuals aged 65 and above, yet only 25% of participants in cancer-focused studies come from this age group.
Expert perspectives emphasize that the control trial definition of randomized controlled trials is critical for generating reliable information that informs both medical practice and policy. Sue Peschin, President and CEO of the Alliance for Aging Research, highlights the importance of including older adults in trials to ensure that findings are pertinent to the demographic most affected by chronic illnesses. The integration of innovative methodologies, such as electronic health records (EHRs) and electronic data capture systems, is enhancing the efficiency of RCTs, enabling researchers to streamline data management and bolster patient recruitment. As the landscape of medical investigation evolves, the commitment to RCTs remains essential for ensuring that health innovations benefit those who need them the most.
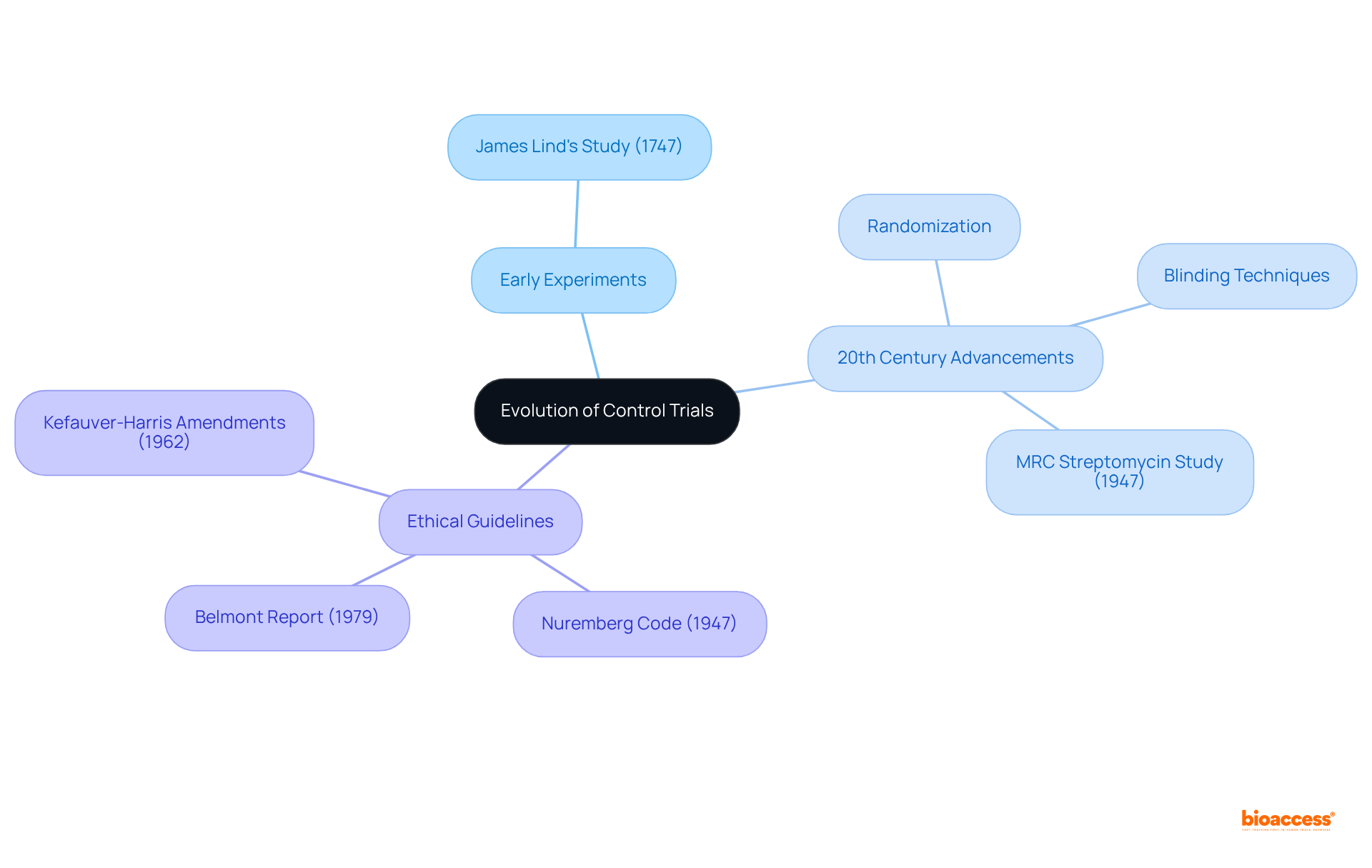
The concept of controlled experiments has its roots in early medical studies, notably marked by Scottish physician James Lind's investigation in 1747, which examined the effects of citrus fruits on scurvy among sailors. This landmark study exemplified the power of controlled methodologies to produce reliable results.
As the field progressed, particularly throughout the 20th century, the introduction of randomization and blinding techniques transformed study design, significantly bolstering the validity of research findings. In response to historical abuses in medical research, ethical guidelines emerged, including:
These were complemented by regulatory frameworks such as the Kefauver-Harris amendments of 1962. These developments ensured that controlled experiments are conducted with integrity, prioritizing participant welfare and enhancing the reliability of research outcomes.
The impact of Lind's experiment, along with subsequent advancements in testing methods, underscores the critical role of the control trial definition in shaping modern medical practices. Furthermore, the MRC Streptomycin study, initiated in 1947, exemplified the importance of randomization, blinding, and controlled comparisons as foundational elements of contemporary medical investigation, resulting in enrollment procedures that are now 50% more efficient than traditional methods.
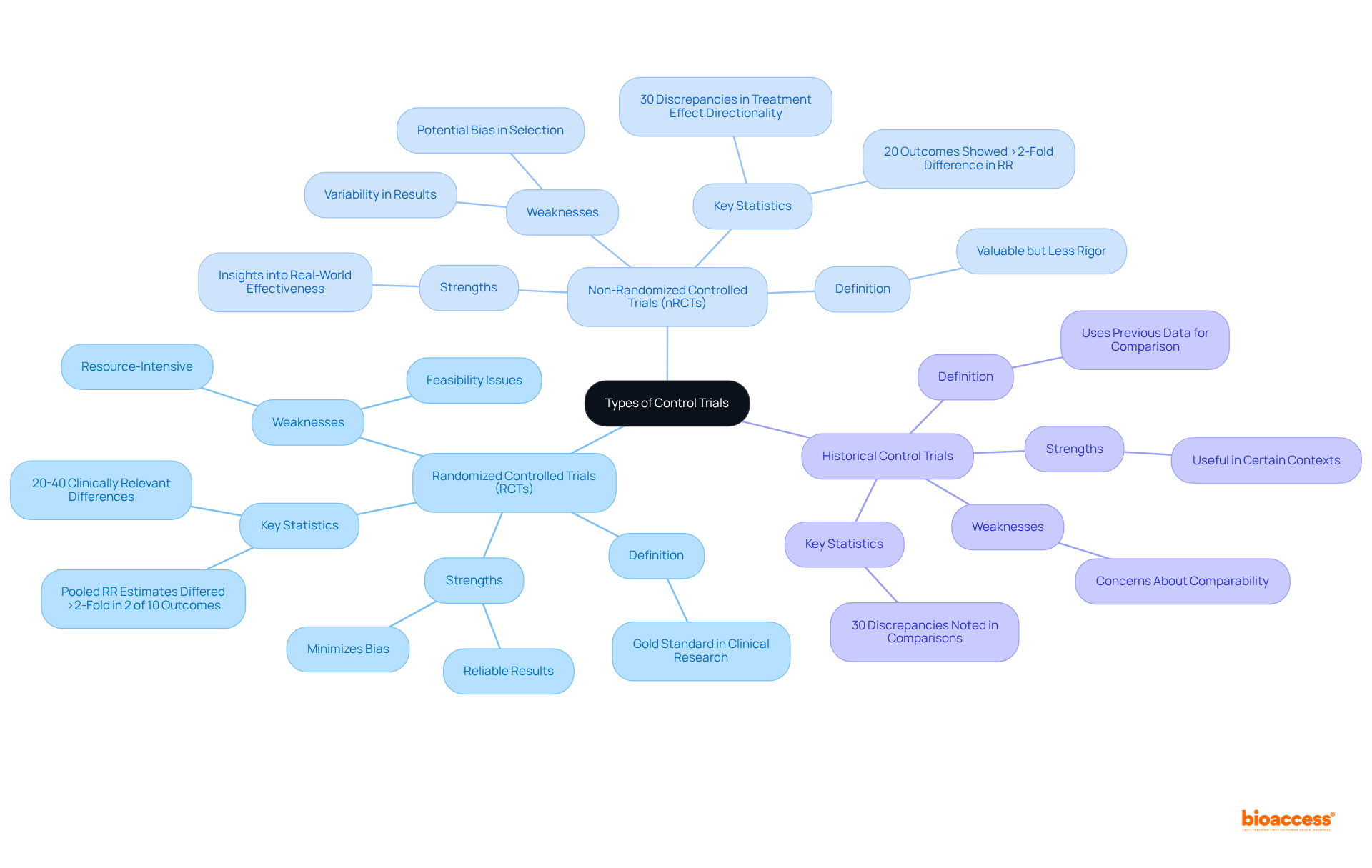
The control trial definition encompasses various types, including randomized controlled studies, non-randomized controlled trials (nRCTs), and historical control trials. Randomized controlled trials are widely regarded as the gold standard in clinical research due to their robust design, which minimizes bias through randomization. This method ensures that participants are assigned to treatment or control groups by chance, thereby reducing selection bias and enhancing the reliability of results. In contrast, nRCTs, while still valuable, do not employ random assignment, which can lead to potential biases in participant selection and outcomes. A recent study found that 20% of outcomes showed a greater than two-fold difference in relative risk (RR) between RCTs and nRCTs, underscoring the importance of randomization in achieving accurate treatment effect estimates. Clinically significant differences in effect estimates may be shown in 20%-40% of cases, emphasizing the variability in outcomes between the two study types.
Historical control studies utilize data from previous research as a comparison group. While this approach can be advantageous in certain contexts, it raises concerns regarding the comparability of groups, as differences in patient characteristics and treatment protocols may influence outcomes. A systematic review highlighted that discrepancies in treatment effect directionality were noted in 30% of comparisons between randomized controlled trials and non-randomized controlled trials, emphasizing the need for careful consideration when interpreting results from historical controls.
Each type of control trial definition presents unique strengths and weaknesses. Randomized controlled trials are commended for their capacity to deliver high-quality evidence, especially in assessing new therapies. However, they can be resource-intensive and may not always be feasible for large-scale public health interventions. Conversely, nRCTs can provide insights into real-world effectiveness but may lack the rigor of randomized controlled trials, leading to variability in results. Expert opinions suggest that while nRCTs can yield comparable results in some cases, the reliability of their findings is often questioned, particularly in surgical contexts where treatment effects can vary significantly. W.A. Ghali has acknowledged the significance of performing additional randomized controlled trials in surgical therapies to ensure dependable treatment recommendations.
In summary, the choice between RCTs and nRCTs should be guided by the specific inquiry questions and contexts, with an understanding of the inherent strengths and limitations of each design. This nuanced method is essential for advancing clinical studies and ensuring that findings contribute meaningfully to medical knowledge.
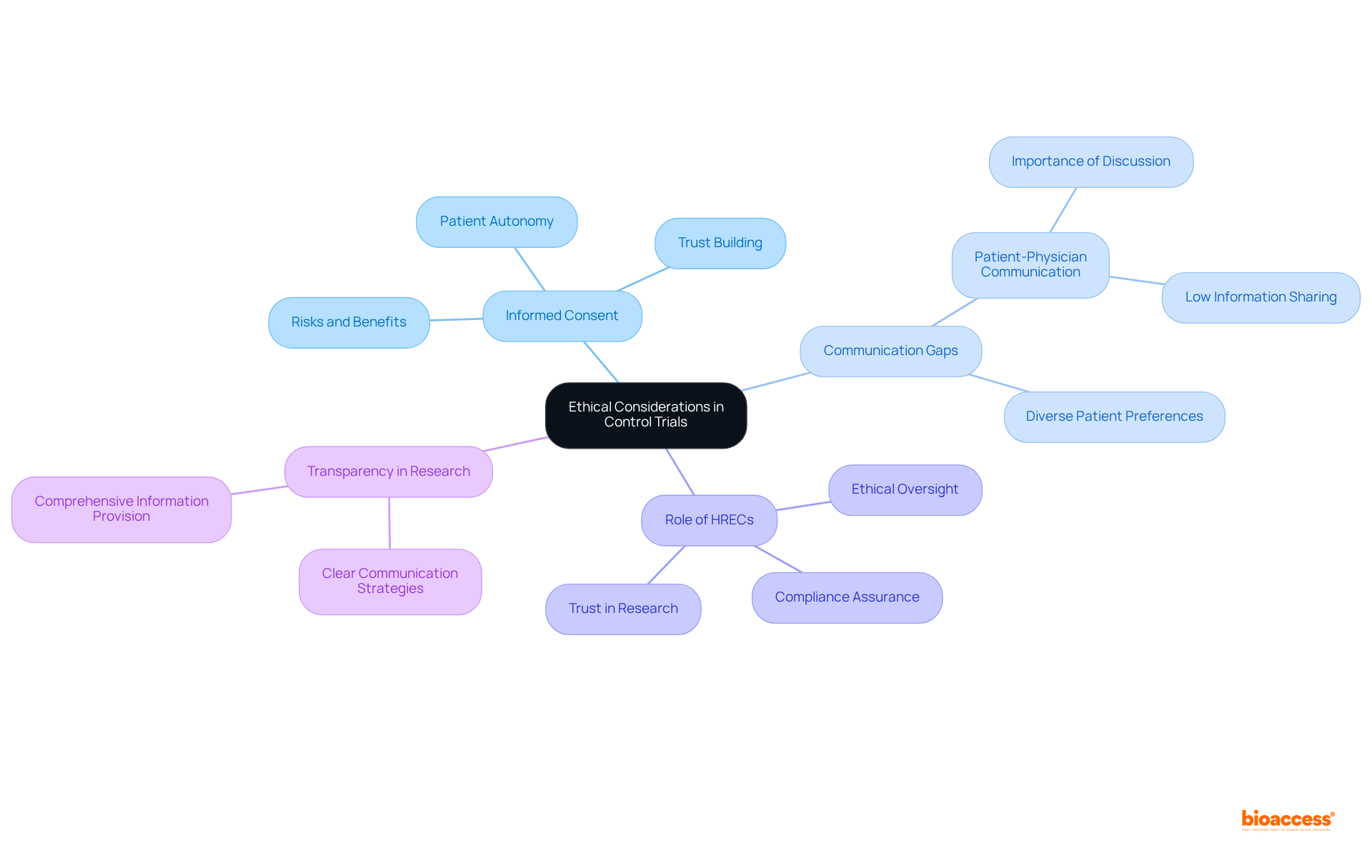
Ethical considerations in control studies are paramount for safeguarding participant welfare and ensuring research integrity. A cornerstone of these considerations is informed consent, which requires that participants are fully informed about the risks and benefits associated with their involvement. This process not only upholds the principle of autonomy but also fosters trust between researchers and participants. Research indicates that 92.7% of oncology patients consider it essential to discuss study details with their healthcare providers prior to participation, underscoring the significance of clear communication. However, only 32% of patients reported that their physicians had ever provided them with details about research studies, highlighting a substantial gap in communication that necessitates attention to enhance informed consent procedures.
Moreover, the necessity of employing a control trial definition is vital for establishing the scientific validity of an experiment. Researchers must navigate the ethical implications of using placebos, particularly when effective treatments are available, ensuring that participants are not deprived of necessary care. The formation of Human Research Ethics Committees (HRECs) plays a crucial role in supervising trials, as they assess proposals and guarantee compliance with ethical standards. Regular interaction with HRECs during the study process enhances ethical integrity, safeguards participant rights, and cultivates trust in the medical field, although researchers have shared varied experiences with these committees.
Current ethical guidelines emphasize the need for transparency and robust communication strategies to ensure that informed consent is genuinely informed. This includes providing comprehensive information about the study's objectives, risks, benefits, and alternatives, allowing participants to make well-informed decisions. As the landscape of clinical research evolves, ongoing discussions about ethical practices and participant engagement remain crucial for advancing the field responsibly, particularly in addressing the challenges faced when involving vulnerable populations.
The essence of control trials is their capacity to provide a reliable framework for evaluating the effectiveness of medical interventions through rigorous methodologies. By employing randomized controlled trials (RCTs), researchers minimize bias and enhance the credibility of their findings, ultimately leading to improved healthcare outcomes. This structured approach fosters advancements in medical research and ensures that the benefits of new treatments are effectively communicated and applicable to diverse populations, particularly older adults who are often underrepresented in clinical studies.
Throughout the article, key concepts such as the historical evolution of control trials, the significance of randomization, and the ethical considerations surrounding participant welfare have been thoroughly examined. The historical context underscores how early experiments laid the groundwork for modern practices, while contemporary challenges highlight the ongoing need for inclusivity and ethical integrity in research. The distinctions between various types of control trials—RCTs, non-randomized controlled trials, and historical controls—illustrate the nuanced landscape of clinical research and the importance of selecting the appropriate methodology based on specific research questions.
Ultimately, the commitment to upholding the principles of control trials is vital for advancing medical knowledge and ensuring the ethical conduct of research. As the field continues to evolve, stakeholders must prioritize transparent communication, robust ethical standards, and innovative recruitment strategies to ensure that all demographics are represented in clinical trials. This dedication enhances the quality of research and strengthens public trust in medical findings, paving the way for future health innovations that can benefit everyone.
What are randomized controlled trials (RCTs)?
Randomized controlled trials (RCTs) are scientific experiments designed to evaluate the effectiveness of interventions by comparing an experimental group, which receives the treatment, to a control group, which may receive a placebo or standard treatment.
Why is randomization important in RCTs?
Randomization is crucial in RCTs as it reduces bias, allowing researchers to attribute observed effects directly to the intervention rather than to external influences.
What is the significance of RCTs in medical research?
RCTs provide high-quality evidence regarding the effectiveness and safety of new therapies, making them a cornerstone of medical research.
What challenges do RCTs face in patient recruitment?
Approximately 37% of research studies fail to recruit enough patients to proceed, and 11% do not enroll any participants at all. This issue is particularly notable among older adults, who are often affected by chronic illnesses.
How are older adults represented in cancer-focused studies?
Although over half of all cancers are diagnosed in individuals aged 65 and above, only 25% of participants in cancer-focused studies come from this age group.
What do experts say about the inclusion of older adults in RCTs?
Experts, including Sue Peschin, emphasize the importance of including older adults in trials to ensure that findings are relevant to the demographic most affected by chronic illnesses.
How are innovative methodologies improving RCTs?
The integration of innovative methodologies, such as electronic health records (EHRs) and electronic data capture systems, is enhancing the efficiency of RCTs by streamlining data management and improving patient recruitment.
Why is the commitment to RCTs essential as medical investigation evolves?
The commitment to RCTs remains essential to ensure that health innovations benefit those who need them the most, especially vulnerable populations such as older adults.