


Adaptive design trials are transforming clinical research by allowing real-time modifications based on interim results, which significantly boosts study efficiency and effectiveness. This article explores the complexities of mastering these innovative methodologies while ensuring compliance with the Therapeutic Goods Administration (TGA) regulatory framework. As the Medtech landscape evolves, researchers must consider:
Adaptive methodologies represent a groundbreaking approach in clinical research, allowing for modifications to study and statistical procedures based on interim results. These innovative models enhance the effectiveness of clinical studies by enabling adjustments in sample size, treatment distribution, or endpoints as new information emerges. With bioaccess, you can enroll treatment-naive cardiology or neurology cohorts 50% faster than traditional Western sites, achieving significant savings of $25K per patient with FDA-ready data-no rework, no delays.
Key types of adaptive designs include:
Understanding these concepts is crucial for organizing and executing tests that involve adaptive design trials and regulatory acceptance by TGA in Australia. As the Medtech landscape evolves, collaboration and innovative strategies like adaptive methodologies will be key to overcoming challenges in clinical research.

The Therapeutic Goods Administration (TGA) has established specific guidelines for conducting clinical studies, especially regarding adaptive design trials and regulatory acceptance by TGA. Understanding these requirements is crucial for success in clinical research.
Principais requisitos:
Utilizing a comprehensive clinical study management service like bioaccess can significantly streamline this process. Their expertise in feasibility studies, site selection, compliance reviews, testing setup, import permits, project management, and reporting directly addresses challenges such as regulatory hurdles and recruitment issues. By understanding these requirements and leveraging specialized services, medical device startups can facilitate a smoother approval process through adaptive design trials and regulatory acceptance by TGA.
In the ever-evolving Medtech landscape, collaboration with experienced partners is essential. Bioaccess not only navigates the complexities of clinical trials but also enhances the likelihood of successful outcomes. By engaging with such specialized services, you can focus on innovation while ensuring compliance and efficiency in your clinical studies.

When planning your adaptive design strategy, it’s crucial to follow these key steps:
Define Objectives: Clearly outline the primary and supplementary aims of your study, ensuring they align with the principles of flexible methodology. This clarity is essential; flexible approaches can significantly enhance study success rates by allowing for adjustments based on interim findings.
Select Suitable Format: Choose the flexible layout that best fits your objectives, such as group sequential or response-adaptive randomization. Notably, group sequential structures were utilized in 60% of phase 3 studies, while response-adaptive randomization modifies treatment distribution based on interim results.
Develop a Statistical Analysis Plan: This plan should detail how interim analyses will be conducted and how decisions will be made based on the data. Flexibility is key here, as adaptive studies often require modifications to sample sizes and allocation ratios.
Risk Evaluation: Identify potential risks associated with the flexible design and develop strategies to mitigate them. Understanding the implications of adaptations is vital; while adaptive trials can reduce resource use and completion time, they may also introduce biases if not managed carefully.
Stakeholder Engagement: Involve key stakeholders, including governing bodies and ethics committees, early in the planning process. This ensures alignment and addresses concerns, fostering coherence on goals and tackling any issues. Such collaboration ultimately enables smoother implementation and increases the chances of compliance approval.
By leveraging bioaccess®'s extensive clinical study management services - ranging from feasibility assessments and site selection to compliance evaluations and project oversight - you can achieve 50% faster patient enrollment and realize $25K savings per patient with FDA-ready data. A well-structured plan not only facilitates smoother execution but also enhances the likelihood of success in adaptive design trials and regulatory acceptance by TGA.

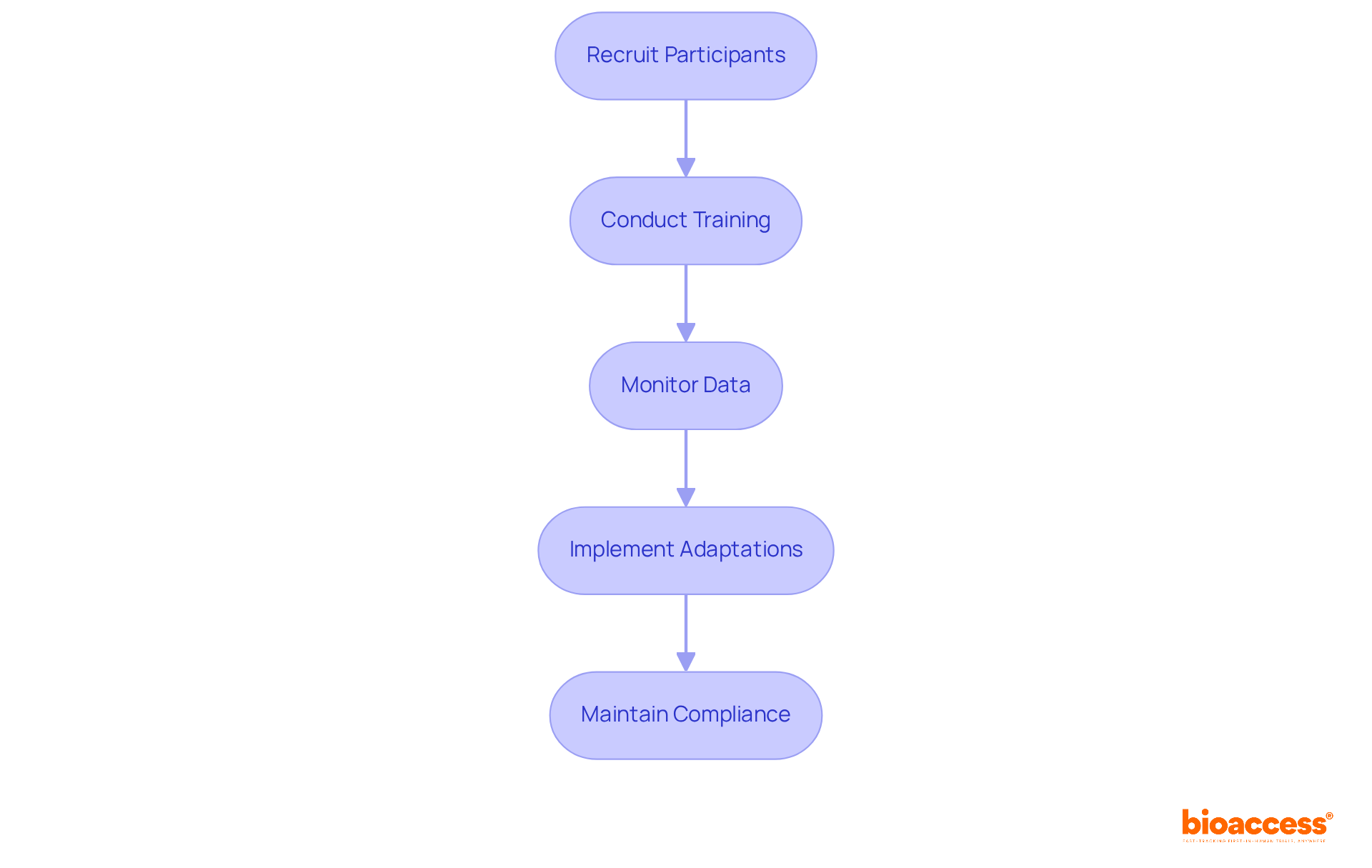
To successfully execute your adaptive design trial, adhere to the following best practices:
Recruit Participants: Implement robust recruitment strategies to ensure a diverse and adequate participant pool. Efficient recruitment is essential, as research shows that flexible studies can boost patient involvement by illustrating how participant information is used to enhance results.
Conduct Training: Ensure that all team members are thoroughly trained on the adaptive design protocol and understand their roles in data collection and analysis. Training effectiveness statistics indicate that well-prepared teams can significantly reduce errors and enhance efficiency.
Monitor Data: Continuously oversee experimental data to identify when modifications are necessary. This includes conducting regular interim analyses as outlined in your statistical plan. More than half of flexible studies have reported unplanned modifications, emphasizing the requirement for careful data supervision.
Implement Adaptations: Make necessary adjustments to the experiment based on interim results, ensuring that all changes are documented and communicated to stakeholders. The iterative nature of adaptive designs allows for real-time modifications, which can lead to more efficient drug development processes.
Maintain Compliance: Regularly review adherence to TGA regulations and ethical standards throughout the study. Following compliance guidelines is essential, as it fosters trust and credibility with oversight authorities.
By following these steps, you will not only enhance the success of your experiment but also create a solid foundation for adaptive design trials and regulatory acceptance by TGA.
To effectively analyze and interpret data from adaptive design trials, it’s crucial to follow these essential steps:
Conduct Statistical Analysis: Utilize robust statistical techniques tailored to the flexible framework, ensuring that the effects of any changes during the study are accurately reflected in the outcomes. For instance, the median sample size for flexible Phase II studies is 86 participants, compared to 110 for traditional Phase II studies, underscoring the effectiveness of flexible approaches.
Evaluate Outcomes: Rigorously assess whether the study met its primary and secondary objectives, determining the clinical significance of the findings. This evaluation is vital, as flexible experiments often yield more precise treatment estimates than conventional formats. The RECOVERY study, for example, demonstrated the efficacy of dexamethasone in reducing mortality among ventilated patients, showcasing the real-world impact of flexible methodologies.
Document Findings: Compile a comprehensive report detailing the analysis process, results, and any adaptations made throughout the trial. This documentation is essential for maintaining transparency and supporting compliance submissions, particularly in light of the FDA's guidance on flexible frameworks introduced in 2019, which highlights the significance of adaptive design trials and regulatory acceptance by TGA along with clear decision rules.
Engage Stakeholders: Actively share findings with stakeholders, including regulatory bodies, to promote open communication and facilitate discussions about subsequent steps. Collaborating with biostatisticians early in the process can enhance the robustness of the statistical analysis and decision-making, adhering to best practices in adaptive study methodology.
Plan for Future Trials: Leverage insights gained from the analysis to inform the design of future research initiatives. Understanding the statistical characteristics and potential adjustments can significantly improve the success rates of subsequent experiments.
A comprehensive examination and interpretation are essential for validating results and ensuring adherence to standards, ultimately increasing the likelihood of successful submissions.

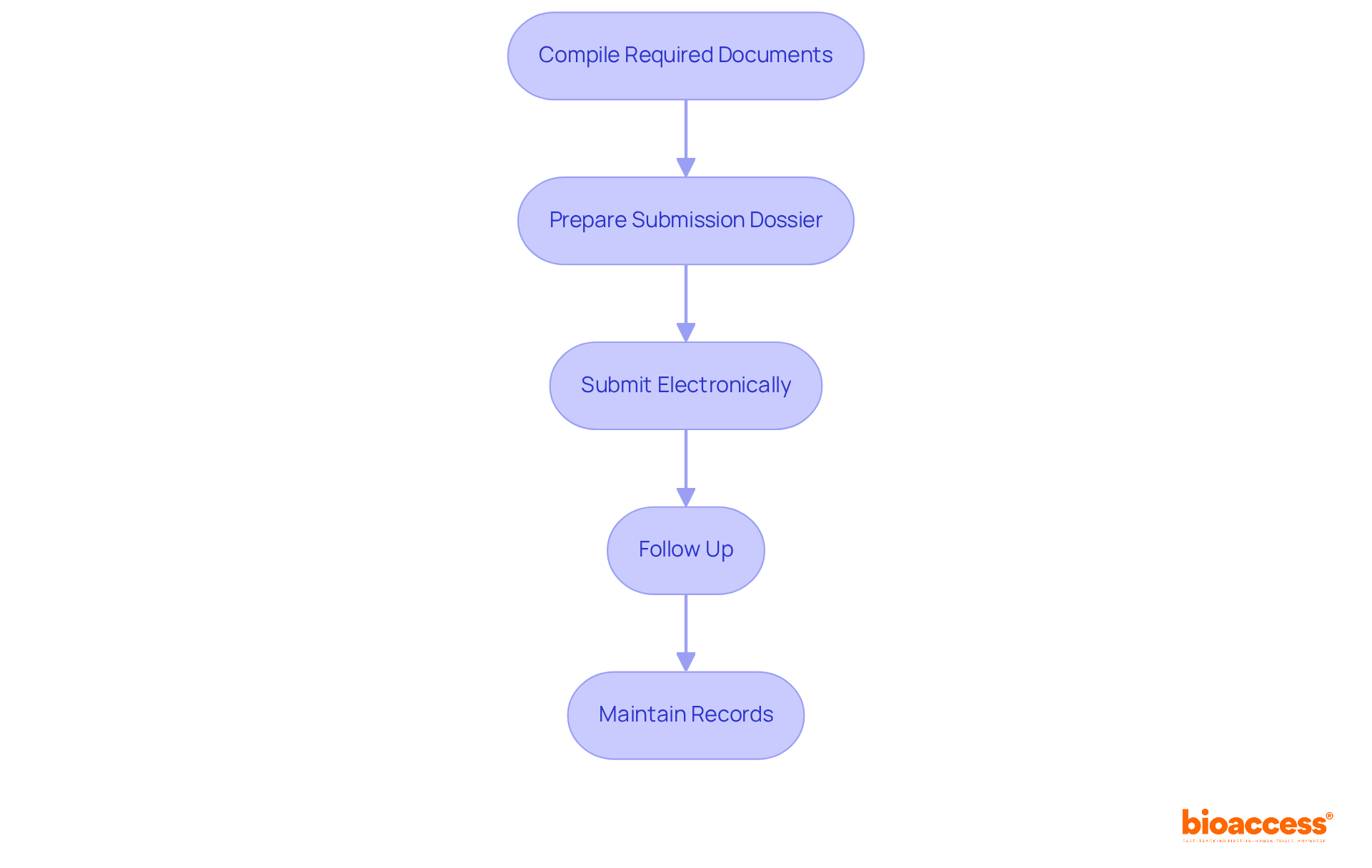
To submit documentation for regulatory approval, follow these essential steps:
A well-prepared submission significantly enhances the likelihood of a smooth approval process, which is essential for adaptive design trials and regulatory acceptance by TGA, facilitating the commercialization of your product.
Mastering adaptive design trials is crucial for securing regulatory acceptance from the TGA. This innovative approach not only boosts the flexibility and efficiency of clinical studies but also aligns with the rapidly evolving landscape of medical technology. By grasping adaptive methodologies, stakeholders can adeptly navigate the complexities of clinical trials while optimizing outcomes and resource allocation.
Key insights from this article underscore the necessity of:
Each of these steps is vital in ensuring compliance and fostering successful trial outcomes. The integration of adaptive design principles can yield significant time and cost savings, ultimately accelerating the journey to market for new therapies.
As the Medtech sector continues to progress, embracing adaptive design trials presents a strategic advantage. Engaging with specialized services like bioaccess can streamline processes and enhance collaboration among stakeholders. By prioritizing adaptive methodologies, researchers and organizations not only meet regulatory expectations but also contribute to innovative solutions that address urgent healthcare needs.
What are adaptive design trials in clinical research?
Adaptive design trials are innovative methodologies that allow modifications to study and statistical procedures based on interim results, enhancing the effectiveness of clinical studies by enabling adjustments in sample size, treatment distribution, or endpoints as new information emerges.
What are the key types of adaptive designs?
The key types of adaptive designs include: - Group Sequential Designs: Allow early stopping for efficacy or futility based on interim analyses. - Sample Size Re-estimation: Adjusts the number of participants based on interim results to ensure adequate power. - Response-Adaptive Randomization: Allocates more participants to better-performing treatments as the study progresses.
How does bioaccess improve the efficiency of enrolling participants in clinical trials?
Bioaccess enables the enrollment of treatment-naive cardiology or neurology cohorts 50% faster than traditional Western sites, achieving significant savings of $25K per patient while providing FDA-ready data without rework or delays.
What are the key regulatory requirements established by the TGA for clinical studies?
The key requirements include: - Ethical Approval: Trials must receive approval from a Human Research Ethics Committee (HREC). - Clinical Study Notification (CSN): Sponsors must inform the TGA of their intention to conduct a study, providing detailed information about the design and objectives. - Documentation: Essential documents must comply with the TGA's Common Technical Document (CTD) format, including the study protocol, informed consent forms, and safety monitoring plans.
How can utilizing a clinical study management service like bioaccess help with TGA regulatory requirements?
Bioaccess provides expertise in feasibility studies, site selection, compliance reviews, testing setup, import permits, project management, and reporting, which helps address challenges such as regulatory hurdles and recruitment issues, facilitating a smoother approval process through adaptive design trials.
Why is collaboration with experienced partners important in the Medtech landscape?
Collaboration with experienced partners is essential to navigate the complexities of clinical trials, enhance the likelihood of successful outcomes, and ensure compliance and efficiency in clinical studies, allowing medical device startups to focus on innovation.