


Nuclear imaging stands as a vital medical technique, employing small amounts of radioactive materials to observe organ and tissue function. This approach provides profound insights into physiological processes, extending beyond mere structural details. The article underscores its significance in diagnosing various conditions, while also detailing advancements in technology that bolster diagnostic accuracy. Furthermore, it highlights the technique's pivotal role in personalized medicine, reinforcing its importance in enhancing patient outcomes and optimizing healthcare management.
Nuclear imaging stands at the forefront of modern healthcare, offering a unique lens through which medical professionals can observe the intricate workings of the human body. This technique, which utilizes small amounts of radioactive materials, transcends traditional imaging methods to provide critical insights into organ and tissue function. Consequently, it paves the way for timely and accurate diagnoses of various conditions. However, as reliance on nuclear imaging grows, a pressing question emerges: how can healthcare providers effectively balance the undeniable benefits of this technology with the potential risks associated with radiation exposure?
Nuclear visualization is a crucial medical technique that exemplifies what is nuclear imaging, as it employs small amounts of radioactive materials, known as radiotracers, to observe the functioning of organs and tissues within the body. Unlike conventional imaging techniques that primarily emphasize structural aspects, radioactive imaging offers insights into physiological functions by identifying the radiation released from the radiotracers after their introduction to the patient. This technique is essential for diagnosing a range of conditions, including cancers, heart diseases, and other disorders, as it reveals organ functionality at a cellular level.
As of 2025, the global landscape sees over 50 million radiological procedures performed annually, underscoring its growing significance in contemporary healthcare. The most commonly used radioisotope in these processes is technetium-99m (Tc-99m), which constitutes approximately 80% of all imaging procedures conducted each year. In the USA alone, over 20 million radiology procedures are performed annually, highlighting the pressing need for efficient diagnostic solutions.
Recent advancements in nuclear visualization technology have markedly enhanced diagnostic capabilities. For instance, PSMA-PET scans have proven to surpass traditional MRI in staging prostate cancer, detecting metastatic disease in 46% of cases previously deemed negative. Additionally, the integration of radioligand therapies has shown promising outcomes in improving overall survival rates for individuals with metastatic castration-resistant prostate cancer.
Medical professionals emphasize the importance of nuclear diagnostics, explaining what is nuclear imaging in personalized medicine and noting its role in developing customized treatment strategies. The capacity to visualize biochemical functions in vivo facilitates more accurate diagnoses and better-informed treatment plans, ultimately enhancing patient outcomes. Case studies, such as those demonstrating the effectiveness of PSMA-PET/CT in identifying metastatic prostate cancer overlooked by other scanning methods, underscore the technique's pivotal role in advancing healthcare.

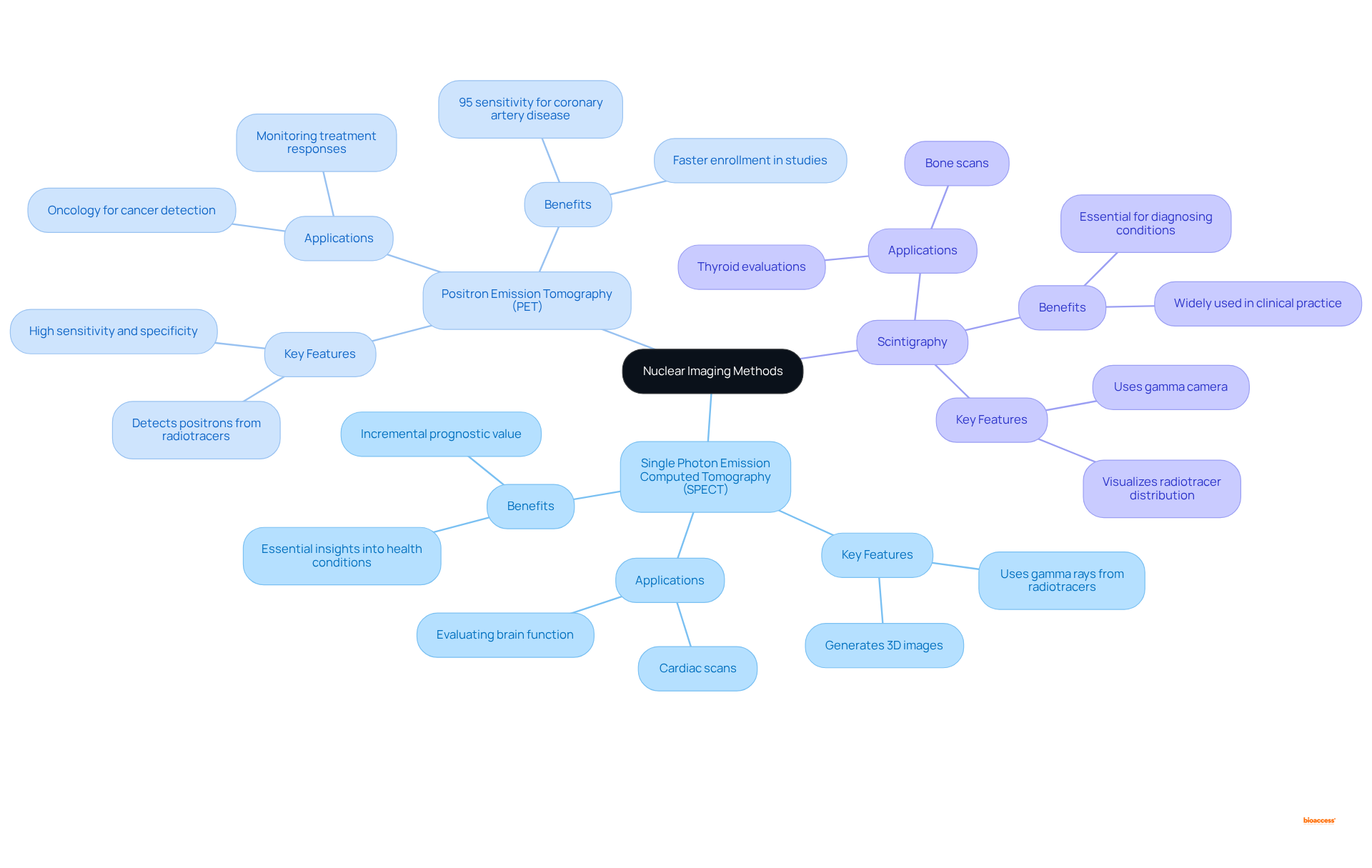
Nuclear imaging encompasses several key techniques that play vital roles in modern medicine:
Single Photon Emission Computed Tomography (SPECT): Utilizing gamma rays emitted from radiotracers, SPECT generates detailed three-dimensional images of internal structures. It is especially valuable in cardiac scans and evaluating brain function, offering essential insights into different health conditions.
Positron Emission Tomography (PET): PET scans detect positrons emitted by radiotracers, providing a window into metabolic processes within tissues. This technique is especially beneficial in oncology, where it aids in the detection of cancerous cells and monitoring treatment responses. Recent advancements have demonstrated that PET myocardial perfusion assessment (MPI) boasts a sensitivity and specificity of 95% for detecting coronary artery disease, underscoring its diagnostic prowess. Moreover, enrollment in radiological studies is 50% quicker than conventional markets, emphasizing the effectiveness of clinical research in this area.
Scintigraphy: This method employs a gamma camera to visualize the distribution of radiotracers throughout the body. Scintigraphy is commonly used for bone scans and thyroid evaluations, providing essential information for diagnosing various conditions.
Each of these methods offers distinct uses and benefits, which raises the question of what is nuclear imaging as an essential instrument in medical practice. For instance, almost 20 million nuclear medicine procedures utilizing radiopharmaceuticals and diagnostic tools are performed each year in the United States, highlighting the commonality and significance of these methods. PET scans have become the primary imaging modality for cancer staging globally, with a significant increase in accuracy compared to traditional methods. Radiologists emphasize the advantages of PET scans, pointing out their capacity to deliver clearer images and more accurate diagnoses, which ultimately improve healthcare management and treatment results. Furthermore, the overall radiation exposure from the majority of radiopharmaceuticals utilized in diagnostic studies is comparable to that from standard chest x-rays or CT scans, ensuring safety while providing essential diagnostic information.
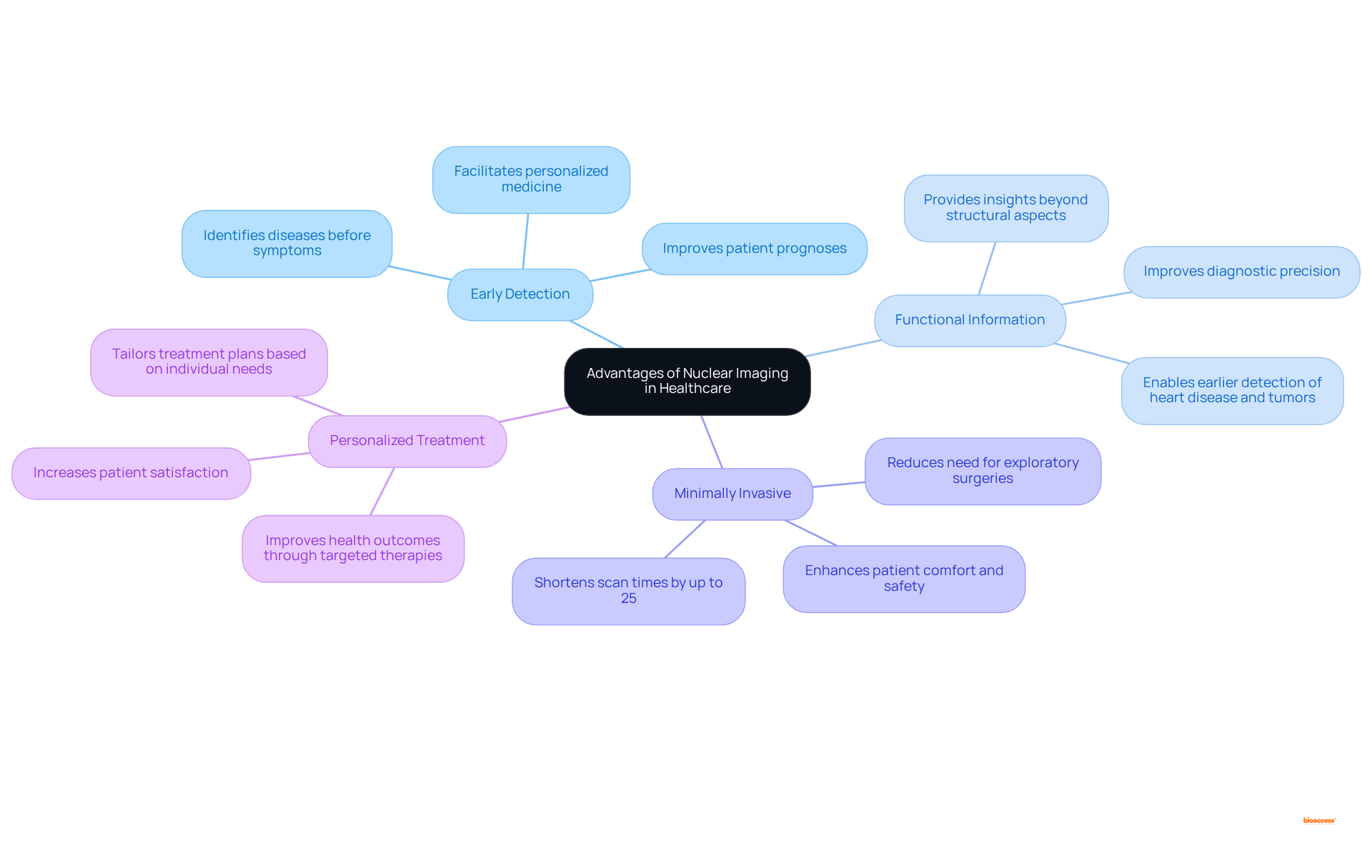
Nuclear imaging presents a range of significant benefits in healthcare, including:
Personalized treatment involves understanding what is nuclear imaging, as the thorough insights obtained from advanced scanning enable healthcare providers to tailor treatment plans based on individual requirements. This customized method not only improves treatment effectiveness but also increases satisfaction by aligning care with specific health profiles. As mentioned by Dr. Horacio Amaral, sharing knowledge in medical diagnostics can enhance access to care, especially in remote regions.
Enhanced health results can be achieved by understanding what is nuclear imaging, as the incorporation of advanced scans into clinical practice has been demonstrated to improve health outcomes. For example, early identification via advanced scanning can result in prompt treatments, slowing disease advancement and enhancing overall quality of life. As healthcare continues to advance, the function of radiological techniques in enabling personalized medicine grows more essential, guaranteeing that patients obtain the most suitable and effective treatment customized to their specific conditions.
What is nuclear imaging is widely regarded as a safe diagnostic tool; however, it is essential to consider certain risks and precautions.
In summary, while the benefits of nuclear imaging are typically greater than the associated risks, careful management and adherence to safety protocols are essential to protect patient health. As Dr. Einstein noted, an improved understanding of the risks of radiation is clearly needed, and raising such awareness among providers has been the focus of recent efforts.

Nuclear imaging stands as a cornerstone in contemporary healthcare, employing radiotracers to deliver unparalleled insights into organ and tissue functionality. This groundbreaking technique surpasses conventional imaging methods by illuminating physiological processes, thereby enhancing diagnostic precision and elevating patient care. As the healthcare landscape transforms, the significance of nuclear imaging escalates, highlighting its critical role in personalized medicine and customized treatment approaches.
The article explores various facets of nuclear imaging, spotlighting techniques such as SPECT, PET, and scintigraphy, each offering unique advantages in diagnosing ailments like cancer and heart disease. The discussion underscores the merits of early disease detection, functional insights, and minimally invasive procedures, all contributing to improved patient outcomes. Additionally, it addresses safety considerations related to nuclear imaging, affirming that while risks are present, the overall benefits substantially outweigh them.
Ultimately, grasping the capabilities and applications of nuclear imaging is essential for both healthcare professionals and patients. As advancements persist in enhancing this field, it is imperative to advocate for the responsible application of nuclear imaging techniques, ensuring that individuals receive the most effective and personalized care available. Engaging with this knowledge can empower both patients and providers, cultivating a healthcare environment that prioritizes safety, efficacy, and superior health outcomes.
What is nuclear imaging?
Nuclear imaging is a medical technique that uses small amounts of radioactive materials, called radiotracers, to observe the functioning of organs and tissues in the body, providing insights into physiological functions rather than just structural aspects.
How does nuclear imaging differ from conventional imaging techniques?
Unlike conventional imaging techniques that focus on the structural aspects of the body, nuclear imaging reveals physiological functions by detecting the radiation emitted from radiotracers after they are introduced into the patient.
What are the primary applications of nuclear imaging?
Nuclear imaging is essential for diagnosing various conditions, including cancers, heart diseases, and other disorders, as it reveals organ functionality at the cellular level.
How prevalent is nuclear imaging in healthcare?
As of 2025, over 50 million radiological procedures are performed annually worldwide, with more than 20 million of these procedures occurring in the USA alone, indicating its growing significance in healthcare.
What is the most commonly used radioisotope in nuclear imaging?
The most commonly used radioisotope in nuclear imaging is technetium-99m (Tc-99m), which accounts for approximately 80% of all imaging procedures conducted each year.
What recent advancements have been made in nuclear imaging technology?
Recent advancements include PSMA-PET scans, which have shown to be more effective than traditional MRI in staging prostate cancer, detecting metastatic disease in 46% of cases that were previously deemed negative.
How does nuclear imaging contribute to personalized medicine?
Nuclear imaging plays a crucial role in personalized medicine by enabling the visualization of biochemical functions in vivo, leading to more accurate diagnoses and better-informed treatment plans tailored to individual patients.
Can you provide an example of the effectiveness of nuclear imaging?
Case studies have demonstrated the effectiveness of PSMA-PET/CT scans in identifying metastatic prostate cancer that was overlooked by other scanning methods, highlighting the pivotal role of nuclear imaging in advancing healthcare.