


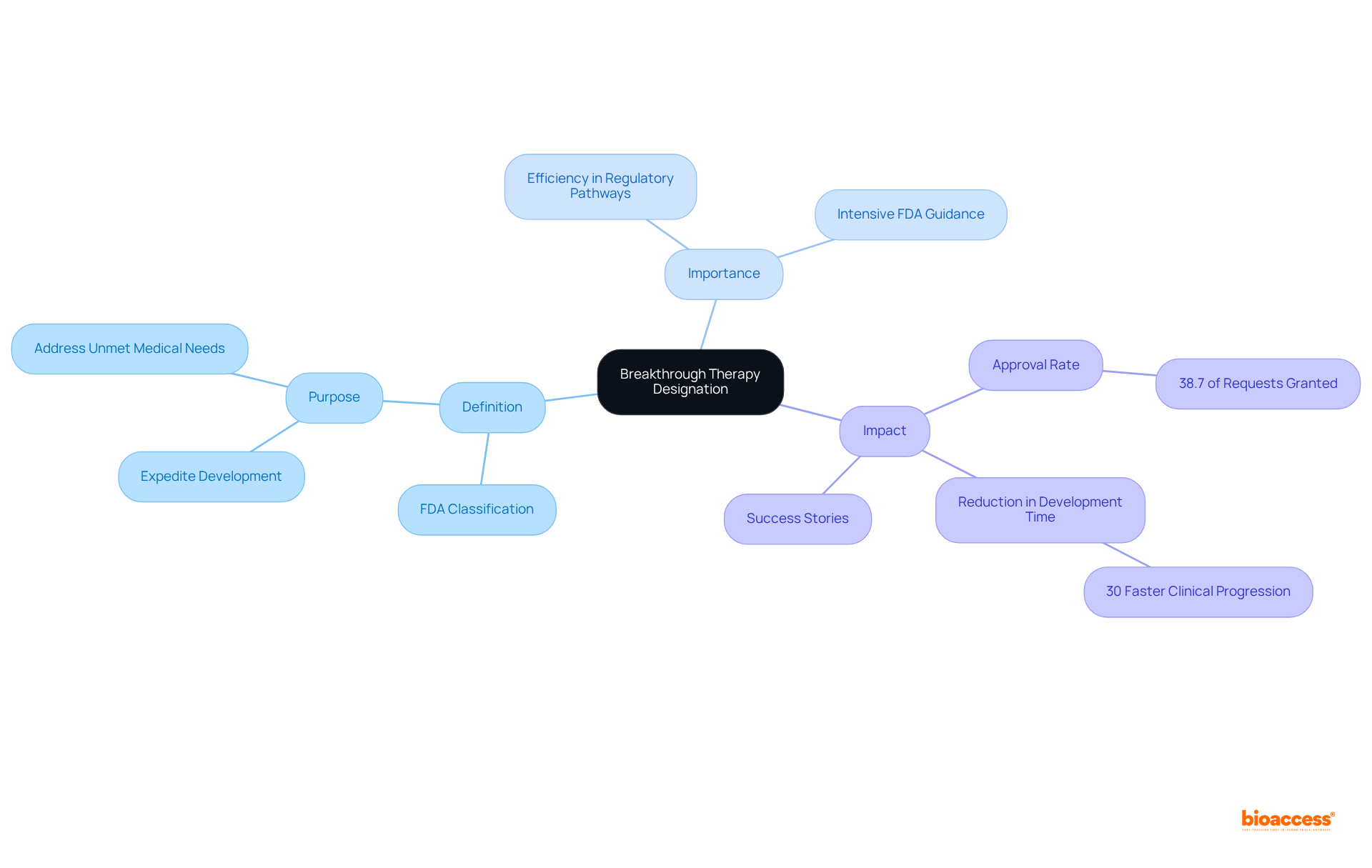
The article emphasizes the critical importance of Breakthrough Therapy Designation (BTD) by the FDA, a mechanism that significantly accelerates the development and approval of drugs targeting serious or life-threatening conditions. This designation not only facilitates a remarkable 30% reduction in clinical progression time but also provides enhanced guidance from the FDA. Such advantages underscore BTD's pivotal role in improving patient access to innovative therapies, effectively addressing unmet medical needs within the healthcare landscape.
Breakthrough drug designation represents a pivotal advancement in the pharmaceutical landscape, aimed at expediting the development of therapies for severe or life-threatening conditions. This designation not only accelerates patient access to potentially life-saving treatments but also offers invaluable support from the FDA, ensuring a more efficient regulatory process.
However, with only approximately 38.7% of requests granted, the journey to obtaining this designation can be fraught with challenges. What strategies can developers employ to enhance their chances of success and fully leverage the benefits of breakthrough therapy designation?
Breakthrough drug designation represents a significant classification conferred by the U.S. Food and Drug Administration (FDA) to expedite the development and evaluation of medications targeting severe or life-threatening conditions. The breakthrough drug designation is critical, as it facilitates a more efficient regulatory pathway, thereby enabling quicker access to potentially life-saving treatments.
Specifically designed for drugs that exhibit preliminary clinical evidence suggesting substantial improvement over existing therapies on clinically significant endpoints, breakthrough drug designation (BTD) is vital in addressing unmet medical needs and enhancing patient outcomes. By reducing the time required for clinical progression and regulatory review—an estimated 30% reduction—breakthrough drug designation (BTD) is instrumental in transforming healthcare delivery.
As Kathleen L. Miller aptly notes, the program known as breakthrough drug designation was established 'to enhance patient access to safe and effective therapies by facilitating the efficient clinical progress of qualifying, clinically meaningful therapies.' Not only does the program accelerate the availability of innovative therapies through breakthrough drug designation, but it also offers sponsors intensive FDA guidance, ensuring a more effective resolution of issues throughout the development process.
Historically, about 38.7% of requests for breakthrough drug designation (BTD) have been granted, highlighting the necessity of well-prepared applications backed by robust clinical data. Successful cases of medications benefiting from breakthrough drug designation have revolutionized treatment paradigms, underscoring the designation's potential to drive significant advancements in healthcare.
To qualify for breakthrough drug designation, a treatment must meet two critical criteria:
This evidence should demonstrate a clinically significant endpoint, such as enhanced survival rates or improved quality of life. Furthermore, the manufacturer is required to submit a comprehensive growth plan detailing the strategy for effective market entry. Understanding these criteria is essential for developers aiming to leverage the advantages of breakthrough drug designation, as approximately 38.7% of requests have been granted, highlighting the necessity of robust clinical data and strategic planning in the application process.
It is equally important to acknowledge the challenges associated with BTD, which include increased scrutiny from regulatory agencies and the public, as well as heightened expectations regarding the therapy's efficacy and safety. The benefits of breakthrough drug designation (BTD), including accelerated review and extensive support in pharmaceutical development, further underscore the significance of this designation. Additionally, maintaining transparent communication with the FDA throughout the process is crucial for aligning expectations and keeping them informed of important changes.
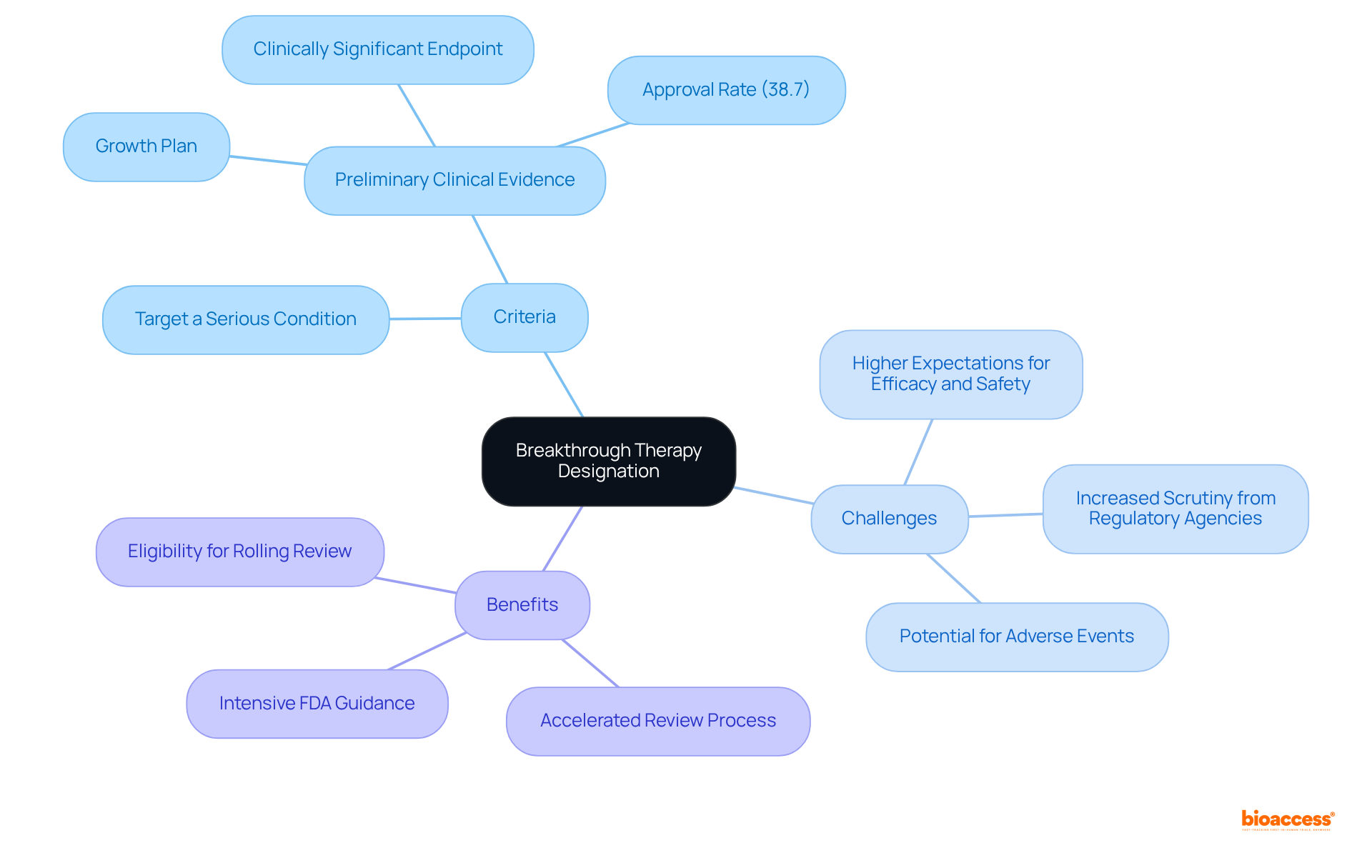
The FDA plays a pivotal role in granting breakthrough drug designation. Launched under the FDA Safety and Innovation Act in 2012, this program aims to accelerate the creation and evaluation of medications intended to address severe or life-threatening conditions when initial evidence demonstrates significant enhancement over current treatments.
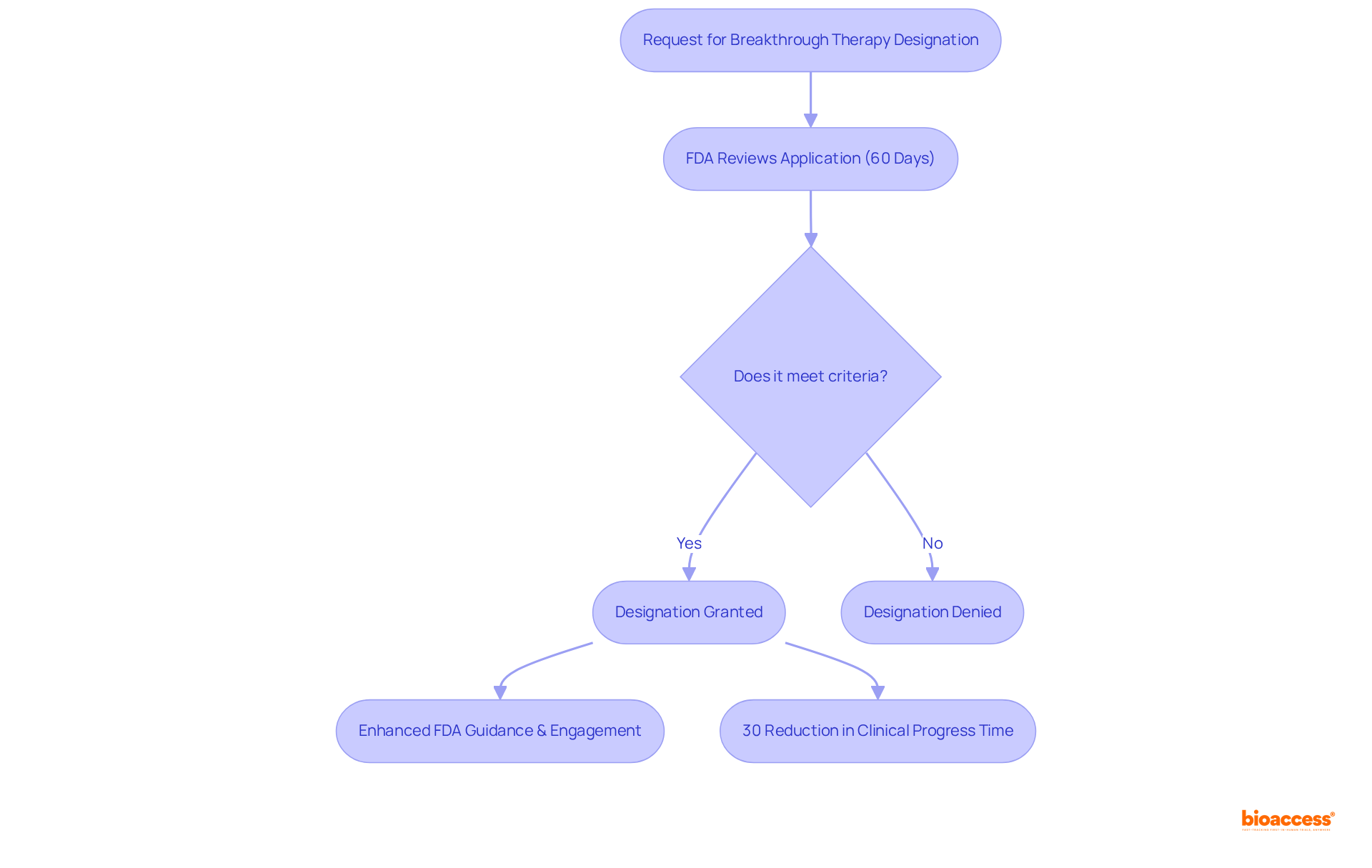
Upon receiving a request for BTD, the FDA commits to reviewing the application within 60 days, examining the initial clinical evidence supplied by the manufacturer to ascertain if the medication fulfills the qualifying criteria. As of 2024, approximately 38.7% of requests for breakthrough drug designation have been granted, underscoring the importance of well-prepared submissions.
If approved, the designation permits enhanced FDA guidance and engagement throughout the medication creation process, including opportunities for more regular meetings and conversations with FDA representatives. This collaborative approach assists in optimizing the project timeline and ensures that the medication meets regulatory expectations.
Maintaining open communication with the FDA is crucial for fostering a productive relationship. Such proactive involvement can significantly decrease the overall progress period, as evidenced by the estimated 30% reduction in clinical progress time for drugs with breakthrough drug designation compared to non-designated drugs.
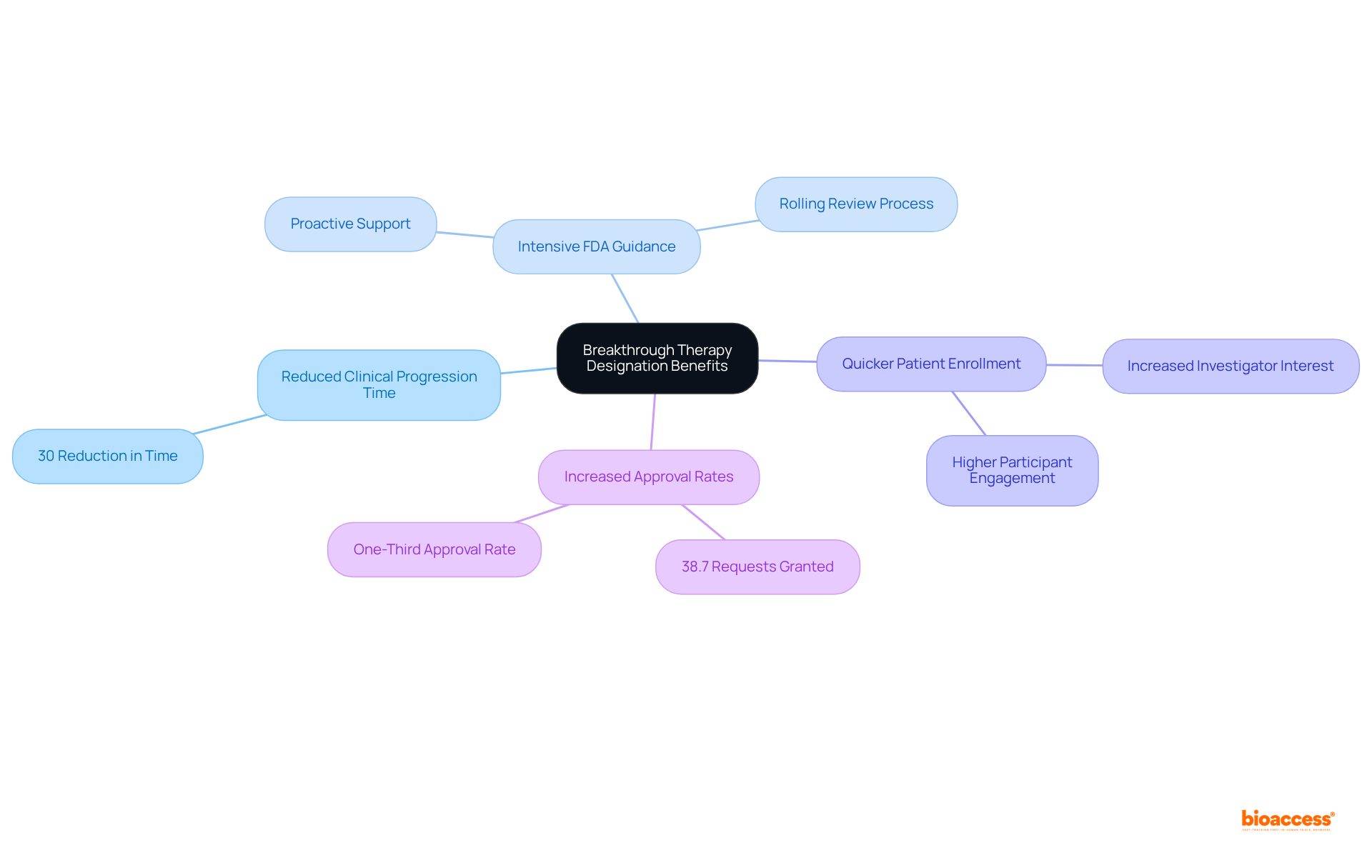
The advantages of breakthrough drug designation for clinical trials are substantial. Drugs that obtain breakthrough drug designation can experience a reduction in clinical progression time by approximately 30%, thereby expediting their route to market. This breakthrough drug designation not only facilitates access to intensive FDA guidance but also ensures that the development process aligns with regulatory expectations, thereby enhancing overall efficiency.
Additionally, the breakthrough drug designation often results in quicker patient enrollment in clinical trials, as it generates increased interest from both investigators and potential participants. To qualify for breakthrough drug designation, therapies must demonstrate a significant improvement on clinically meaningful endpoints compared to existing treatments.
Consequently, therapies that receive breakthrough drug designation benefit from expedited timelines and improved prospects for successful market entry, rendering this designation a vital asset for drug developers. Notably, around 38.7% of requests for breakthrough drug designation have been granted, with the FDA historically approving about one-third of such requests, highlighting its growing significance in the pharmaceutical landscape.
Breakthrough Therapy Designation serves as a vital mechanism established by the FDA to expedite the development of innovative treatments for serious or life-threatening conditions. This designation not only accelerates the regulatory process but also enhances patient access to therapies that demonstrate substantial improvements over existing options. By streamlining clinical progression and offering intensive FDA support, breakthrough drug designation plays a crucial role in transforming the landscape of healthcare.
The article highlights several key aspects of breakthrough drug designation, including:
The emphasis on preliminary clinical evidence and the necessity for a comprehensive growth plan underscores the importance of meticulous preparation in the application process. Additionally, the reduction in clinical progression time by approximately 30% exemplifies the tangible advantages that breakthrough designation offers to drug developers.
Ultimately, the significance of Breakthrough Therapy Designation extends beyond regulatory efficiency; it represents a commitment to addressing unmet medical needs and improving patient outcomes. As the pharmaceutical industry continues to evolve, leveraging the benefits of breakthrough drug designation can lead to groundbreaking advancements in treatment options. Stakeholders are encouraged to recognize the potential of this designation and to actively engage with the FDA to foster innovation that ultimately enhances healthcare delivery and patient well-being.
What is Breakthrough Therapy Designation?
Breakthrough Therapy Designation is a classification granted by the U.S. Food and Drug Administration (FDA) to expedite the development and evaluation of medications for severe or life-threatening conditions.
Why is Breakthrough Therapy Designation important?
It is important because it facilitates a more efficient regulatory pathway, enabling quicker access to potentially life-saving treatments and improving patient outcomes.
What criteria must a drug meet to receive Breakthrough Therapy Designation?
A drug must exhibit preliminary clinical evidence suggesting substantial improvement over existing therapies on clinically significant endpoints to qualify for Breakthrough Therapy Designation.
How much time does Breakthrough Therapy Designation reduce in clinical progression and regulatory review?
Breakthrough Therapy Designation can reduce the time required for clinical progression and regulatory review by an estimated 30%.
What additional support do sponsors receive when their drug is granted Breakthrough Therapy Designation?
Sponsors receive intensive FDA guidance, which helps ensure a more effective resolution of issues throughout the development process.
What percentage of requests for Breakthrough Therapy Designation have historically been granted?
Historically, about 38.7% of requests for Breakthrough Therapy Designation have been granted.
What impact has Breakthrough Therapy Designation had on treatment paradigms?
Successful medications benefiting from Breakthrough Therapy Designation have revolutionized treatment paradigms, demonstrating its potential to drive significant advancements in healthcare.