


The article centers on best practices for mastering informed consent forms in clinical trials, highlighting essential components, readability strategies, and tailored approaches for special populations. It underscores that clear communication, appropriate language, and culturally sensitive practices are vital for ensuring participants fully comprehend their involvement. This understanding fosters trust and ethical compliance in research, establishing a foundation for successful clinical trials.
Informed consent forms stand as the cornerstone of ethical clinical research; however, many participants find it challenging to fully comprehend their contents. By grasping the essential components that render these documents effective, researchers can cultivate a more transparent relationship with participants, thereby enhancing trust and engagement. Yet, how can researchers ensure that these forms are not only compliant but also accessible to diverse populations with varying levels of health literacy?
Informed consent forms are critical in clinical research, requiring several essential components to ensure clarity, compliance, and participant understanding:
Integrating these elements not only satisfies regulatory standards but also fosters trust and openness between researchers and participants. The 2018 updates to the Common Rule underscore the significance of clearly presenting essential information to enhance understanding, ensuring that individuals are sufficiently informed and empowered to make independent choices regarding their involvement in research.

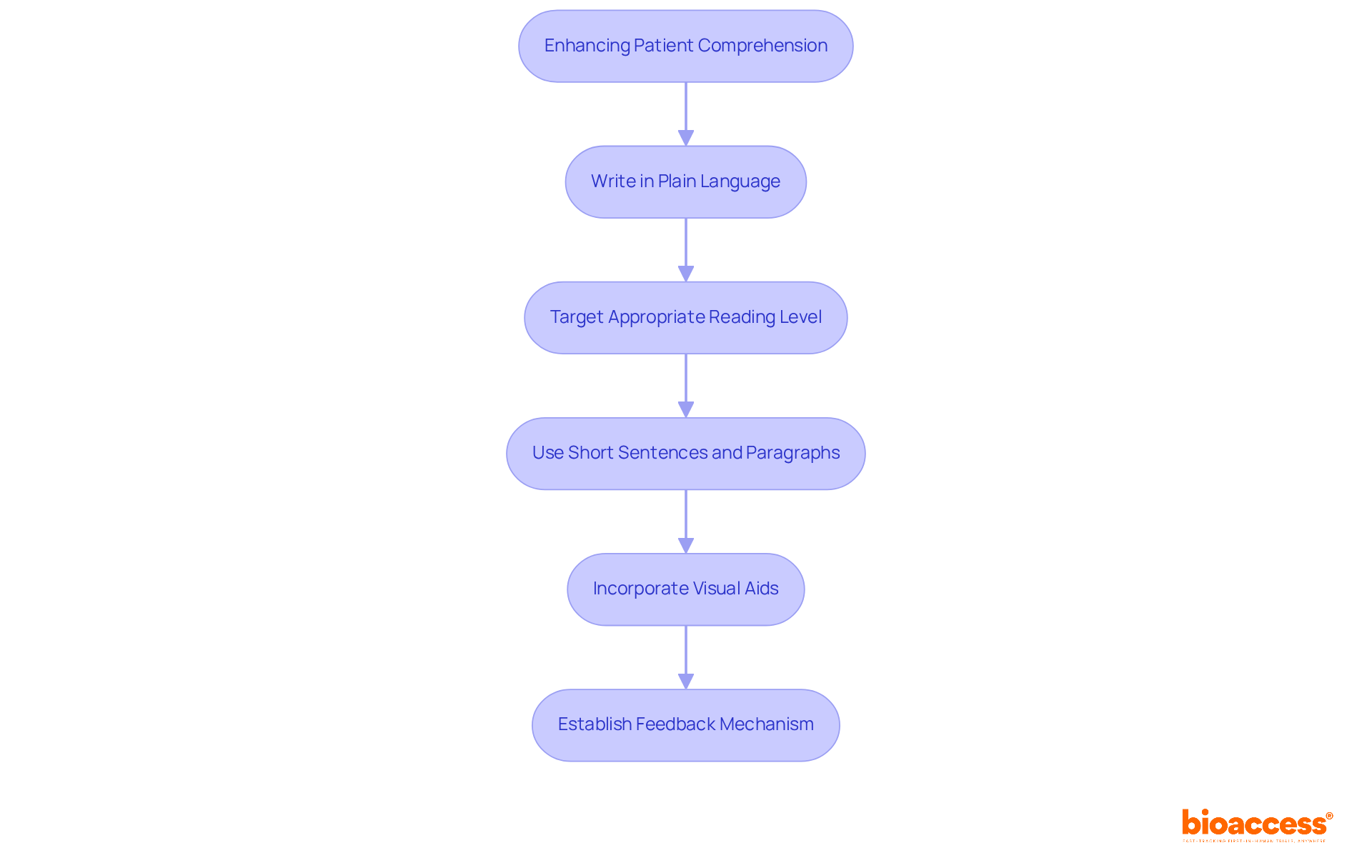
To enhance patient comprehension, informed consent forms must be:
By prioritizing understanding, researchers empower individuals to make informed decisions regarding their participation in the clinical trial ICF. This approach not only aligns with federal recommendations for readability but also fosters participant engagement and trust, ultimately leading to more successful trial outcomes. Neglecting these readability recommendations can adversely affect patient understanding and decision-making, making these strategies essential.
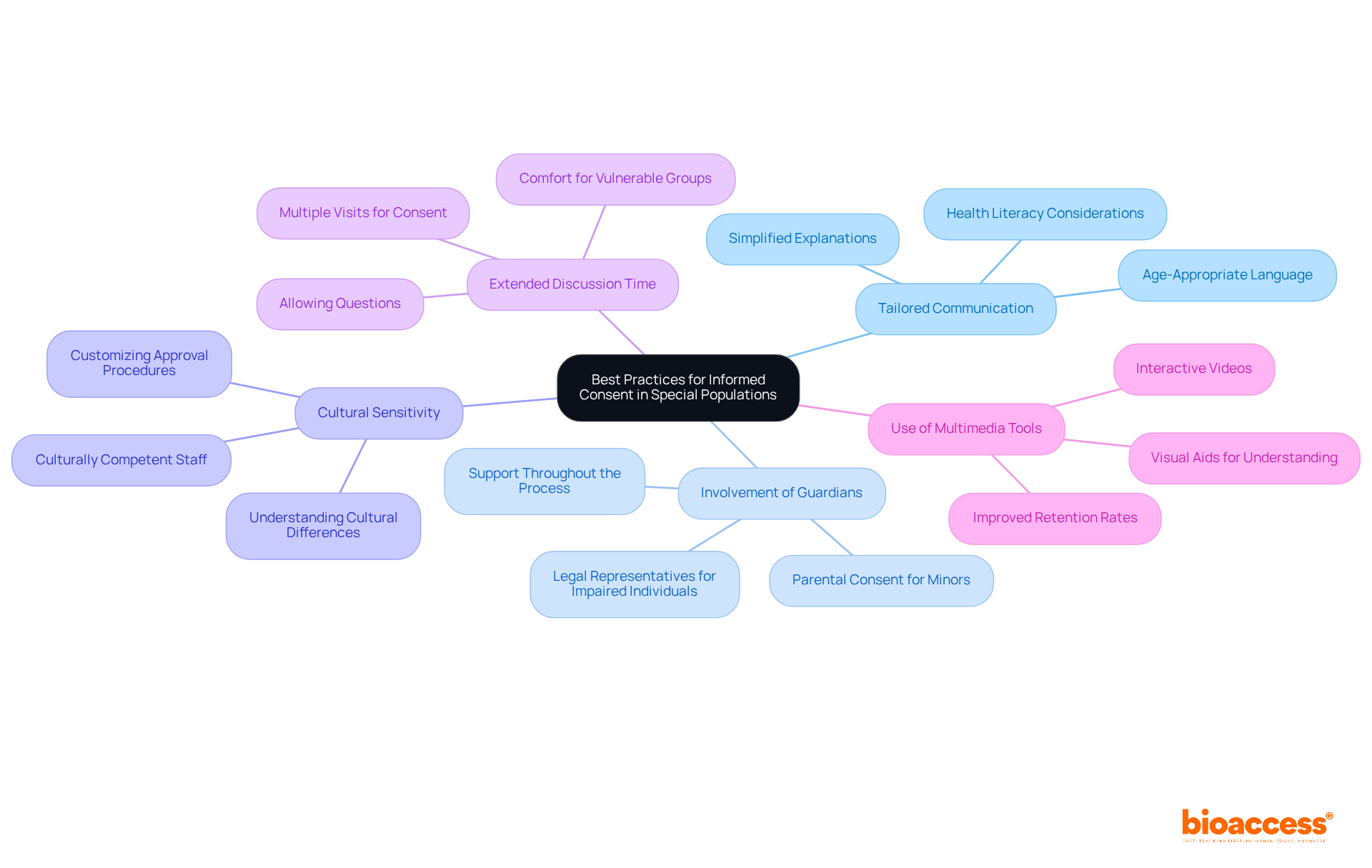
When working with special populations, it is essential to consider the following best practices:
Tailored Communication: Adjust the language and presentation of information based on the specific needs of the population. For instance, using age-appropriate language for children or simplified explanations for individuals with cognitive impairments can significantly enhance comprehension. Research indicates that only 12% of U.S. adults possess proficient health literacy, underscoring the necessity for clear communication strategies to ensure informed agreement.
Involvement of Guardians or Advocates: For minors or individuals unable to provide agreement, it is crucial to involve parents, guardians, or legal representatives in the approval procedure. This involvement guarantees that the individual's best interests are prioritized and that they receive sufficient assistance throughout the entire process.
Cultural Sensitivity: Understanding cultural differences is vital in shaping perceptions of research. Customizing approval procedures to honor cultural values and norms can enhance involvement and trust. As noted by T. Wysocki, "The cultural diversity of the research team must be considered, but the continuing lack of diversity means that it is often difficult to create a legitimately diverse research team with the capacity to reach special populations." Employing culturally competent staff can significantly enhance participation rates among diverse populations.
Extended Discussion Time: Allowing additional time for discussions and questions is essential. This method ensures that participants feel at ease and knowledgeable prior to giving consent, which is especially crucial for vulnerable groups who may require extra time to understand the information.
Use of Multimedia Tools: Incorporating videos or interactive tools to clarify the study and agreement can greatly enhance understanding, particularly for those with varying literacy levels. Research has demonstrated that multimedia agreement formats can improve information retention over time, making them a valuable asset in the approval procedure. For example, the interactive multimedia video consent process exhibited superior retention of information compared to conventional methods, highlighting its effectiveness in enhancing comprehension.
Implementing these practices not only enhances ethical compliance but also fosters trust and respect between researchers and participants from special populations, ultimately leading to more successful and inclusive clinical trials.
Informed consent forms are essential in clinical trials, serving as the cornerstone of ethical research practices. By ensuring that participants fully understand the study's purpose, procedures, risks, and benefits, these forms empower individuals to make informed decisions about their involvement. The integration of essential components, clear language, and tailored communication strategies is crucial for fostering trust and transparency between researchers and participants.
This article underscores several critical insights, including:
Furthermore, it highlights the need for multimedia tools to improve understanding, particularly among individuals with varying literacy levels. By adhering to these best practices, researchers can ensure that informed consent processes are compliant with regulations while remaining respectful and inclusive of all participants.
Ultimately, prioritizing informed consent is vital for upholding the integrity of clinical research. By committing to clarity and accessibility, researchers can significantly enhance participant engagement and decision-making, leading to more successful trial outcomes. It is imperative to continuously evaluate and refine informed consent practices to meet the evolving needs of diverse populations, ensuring that every individual feels valued and informed throughout the research process.
What are the essential components of informed consent forms in clinical research?
The essential components include the study title, purpose of the study, procedures, risks and benefits, confidentiality, voluntary participation, and contact information.
Why is the study title important in an informed consent form?
The study title provides context for the research, helping participants understand what the study is about.
What should be included in the purpose of the study section?
This section should explain the rationale behind the research and its objectives.
What details are required under the procedures section of the informed consent form?
The procedures section must detail the processes individuals will undergo, including any experimental treatments or interventions.
How are risks and benefits addressed in informed consent forms?
Informed consent forms should outline potential risks or discomforts along with the anticipated benefits of participation.
What challenges exist regarding participants' understanding of risks in clinical trials?
Research indicates that comprehension of risks remains a challenge, with only about 50% of individuals fully understanding all aspects of the clinical trial informed consent form.
How is confidentiality addressed in informed consent forms?
Informed consent forms assure individuals that their data will be kept private and explain the measures in place to protect their privacy.
What does voluntary participation mean in the context of informed consent?
Voluntary participation means that involvement in the study is entirely voluntary, allowing individuals to withdraw at any moment without consequence.
Why is it important to provide contact information in informed consent forms?
Providing contact information allows participants to reach out to the research team with any questions or concerns they may have.
How do the 2018 updates to the Common Rule relate to informed consent?
The 2018 updates emphasize the importance of clearly presenting essential information in informed consent forms to enhance understanding and empower individuals to make informed choices about their participation in research.