


The biopharmaceutical and medtech industries are experiencing an unprecedented convergence of operational complexity and regulatory scrutiny, creating an urgent need for systematic approaches to clinical trial management. While the industry has extensively explored technological innovations, regulatory frameworks, and patient-centric methodologies, one critical knowledge gap remains largely unaddressed: the systematic application of Quality by Design (QbD) principles to clinical trial operations as a comprehensive framework for achieving operational excellence.
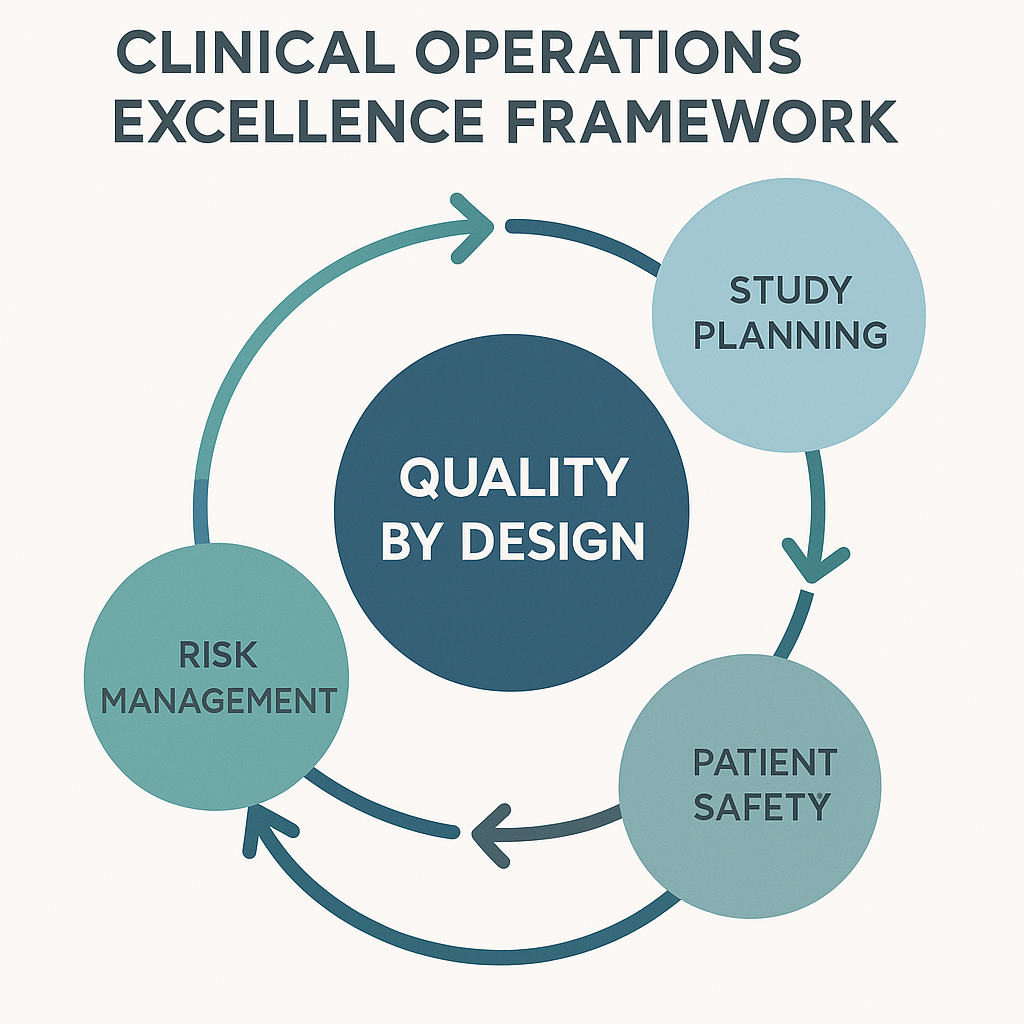
Quality by Design represents a paradigm shift from reactive quality control to proactive quality planning, embedding excellence into every aspect of clinical trial operations from protocol conception through database lock. Unlike traditional approaches that focus on individual operational components in isolation, QbD for clinical operations creates an integrated framework that systematically identifies, controls, and optimizes Critical-to-Quality (CTQ) factors throughout the entire clinical trial lifecycle.
This framework addresses a fundamental operational challenge that remains underexplored in commercial publications: how to translate manufacturing-proven QbD principles into a comprehensive operational excellence methodology specifically tailored for clinical research environments. While pharmaceutical manufacturing has successfully implemented QbD for decades, clinical operations have largely remained fragmented across functional silos, lacking the systematic integration necessary for true operational excellence.
Quality by Design framework for clinical trial operational excellence
The clinical research industry faces an operational crisis that extends far beyond the commonly discussed challenges of patient recruitment and regulatory compliance. Despite decades of technological advancement and process refinement, clinical trials continue to experience systematic failures rooted in fragmented operational approaches. Research indicates that 75% of clinical trials face startup delays averaging one month, resulting in daily sponsor. More significantly, nearly 80% of clinical trials fail to meet enrollment targets on time, and 46% of research sites report that operational challenges are restricting their capacity to participate in new studies.
The root cause of these failures lies not in individual operational deficiencies, but in the absence of a systematic framework that integrates quality considerations across all operational functions. Traditional clinical operations management treats site selection, patient recruitment, data management, regulatory compliance, and monitoring as separate functional domains, each optimized independently. This siloed approach creates systemic vulnerabilities where individual functional excellence fails to translate into overall trial success.
Current industry approaches to operational improvement typically focus on technology adoption, process standardization, or resource optimization within specific functional areas. While these interventions may achieve localized improvements, they fail to address the fundamental integration challenges that drive trial failures. The result is a clinical research ecosystem where operational excellence remains elusive despite significant investments in improvement initiatives.
Quality by Design in clinical operations represents a fundamental reconceptualization of how clinical trials are planned, executed, and managed. Rather than treating quality as an outcome to be measured and corrected, QbD embeds quality considerations into the operational design from the earliest planning stages. This approach recognizes that true operational excellence emerges from systematic integration of quality considerations across all trial functions, creating synergistic effects that exceed the sum of individual functional improvements.
The Clinical Trials Transformation Initiative (CTTI) defines quality in clinical trials as "the absence of errors that matter to decision making—that is, errors which have a meaningful impact on the safety of trial participants or credibility of the results". Building on this foundation, QbD for clinical operations extends this definition to encompass the systematic prevention of operational errors that compromise trial efficiency, participant experience, or data integrity.
The application of QbD principles to clinical operations rests on four foundational pillars that distinguish it from traditional operational management approaches.
Proactive Quality Integration represents the most fundamental departure from traditional clinical operations management. Rather than implementing quality controls as oversight mechanisms, QbD integrates quality considerations into operational design decisions. This means that site selection criteria incorporate quality risk assessments, patient recruitment strategies include retention quality metrics, and monitoring plans are designed around prevention rather than detection of quality issues.
Critical-to-Quality Factor Identification provides the analytical framework for determining which operational elements have the greatest impact on trial success. Unlike traditional approaches that attempt to optimize all operational parameters simultaneously, QbD focuses resources on the specific factors that matter most for each individual trial. For medical device trials, these CTQ factors might include investigator device handling proficiency, patient compliance monitoring, and adverse event reporting accuracy.
Stakeholder-Centric Design ensures that operational decisions consider the needs and capabilities of all stakeholders throughout the trial ecosystem. This includes not only obvious stakeholders like investigators and patients, but also regulatory authorities, data management teams, biostatisticians, and commercial partners. By incorporating stakeholder perspectives into operational design, QbD prevents downstream conflicts and ensures operational feasibility.
Continuous Improvement Integration transforms operational management from a static implementation process into a dynamic learning system. QbD incorporates feedback mechanisms that allow operational parameters to be refined based on real-time performance data, creating trials that become more efficient over their lifecycle rather than experiencing degrading performance.
Traditional clinical operations management typically follows a sequential model where operational decisions are made in isolation, with quality oversight applied as a separate layer. This approach often results in conflicts between operational efficiency and quality requirements, creating tension between functional teams and leading to suboptimal outcomes.
QbD fundamentally alters this dynamic by treating quality and efficiency as complementary rather than competing objectives. By identifying quality requirements early in the operational design process, QbD prevents the need for costly redesigns or remediation activities. This integration creates operational designs that are inherently more robust and efficient than those developed through traditional approaches.
The financial implications of this difference are substantial. Traditional approaches that require remediation of quality issues after implementation typically cost 5-10 times more than QbD approaches that prevent these issues through proactive design. More importantly, QbD approaches create operational systems that become more effective over time, while traditional approaches often experience degrading performance as operational complexity increases.
The identification and systematic management of Critical-to-Quality factors represents the analytical core of operational QbD. Unlike manufacturing applications where CTQ factors are typically physical parameters that can be measured directly, clinical operations CTQ factors are often complex interactions between people, processes, and systems that require sophisticated assessment methodologies.
Site-related CTQ factors represent perhaps the most complex category within clinical operations, as they encompass not only individual site capabilities but also the interactions between sites, sponsors, and the broader trial ecosystem. Research indicates that site selection errors contribute to 29% of enrollment failures, while inadequate site capacity planning affects over 50% of trials.
Investigator Competency and Engagement emerges as a primary CTQ factor that extends beyond traditional qualifications assessment. QbD approaches recognize that investigator competency encompasses not only clinical expertise but also research experience, team management capabilities, and commitment to trial objectives. Systematic assessment of these multidimensional competency factors during site selection can prevent 60-70% of performance-related site issues.
Site Infrastructure and Process Maturity represents another critical dimension that traditional site selection processes often underestimate. This includes not only physical capabilities like patient flow and data management systems, but also process maturity factors such as protocol deviation management, patient retention strategies, and communication effectiveness. Sites with high process maturity demonstrate 40% better enrollment performance and 50% fewer protocol deviations compared to sites selected based solely on traditional criteria.
Site Workload and Capacity Management has emerged as an increasingly critical CTQ factor as trial complexity increases. Research shows that sites managing more than 20 concurrent trials experience significant performance degradation, with 30% longer enrollment times and higher dropout rates. QbD approaches incorporate real-time workload assessment and capacity planning to prevent site overloading.
Patient-related CTQ factors encompass the complex interactions between trial design, patient experience, and operational execution that determine recruitment and retention success. Unlike traditional approaches that focus primarily on eligibility criteria and recruitment channels, QbD examines the entire patient journey to identify systematic optimization opportunities.
Protocol Complexity and Patient Burden represents a fundamental CTQ factor that influences both recruitment feasibility and retention rates. Research demonstrates that each additional visit requirement reduces potential patient participation by 15-20%, while complex eligibility criteria can reduce eligible patient populations by 60-80%. QbD approaches systematically evaluate protocol complexity against recruitment objectives to identify optimization opportunities.
Patient Experience and Engagement Design has become increasingly important as patients demand more convenient and respectful trial participation options. Trials that incorporate patient experience design principles demonstrate 25-35% better retention rates and higher satisfaction scores. QbD approaches integrate patient experience considerations into operational design rather than treating them as secondary objectives.
Geographic and Demographic Accessibility represents a critical CTQ factor that traditional approaches often overlook. Systematic analysis of patient travel burden, demographic matching, and cultural considerations can improve recruitment rates by 30-50% while enhancing trial diversity. QbD approaches incorporate sophisticated geographic modeling and demographic analysis to optimize site selection and recruitment strategies.
Data-related CTQ factors encompass the complex systems and processes that ensure trial data meets regulatory standards while supporting efficient decision-making. Unlike traditional approaches that focus on data cleaning and verification after collection, QbD emphasizes prevention of data quality issues through systematic operational design.
Source Data Quality and Completeness represents the foundation of regulatory-compliant data systems. Research indicates that 60-70% of data quality issues originate from inadequate source data processes rather than subsequent data management activities. QbD approaches focus on optimizing source data capture processes, investigator training, and real-time quality monitoring to prevent rather than detect data quality issues.
Regulatory Documentation and Compliance Management has become increasingly complex as trials span multiple jurisdictions with varying requirements. QbD approaches systematically map regulatory requirements across all participating jurisdictions and design compliance management systems that prevent regulatory issues rather than reacting to them. This proactive approach can reduce regulatory review times by 30-40% while minimizing compliance risks.
Technology Integration and Validation represents an emerging CTQ factor as digital health technologies become more prevalent in clinical trials. Traditional approaches often treat technology validation as a separate activity, leading to integration challenges and validation delays. QbD approaches integrate technology validation into operational design, ensuring that digital tools enhance rather than complicate operational efficiency.
The systematic implementation of QbD principles in clinical operations requires a structured methodology that can be adapted to different trial types, therapeutic areas, and organizational contexts. This implementation framework consists of five interconnected phases that build upon each other to create comprehensive operational excellence.
The foundation of successful QbD implementation lies in achieving genuine alignment among all stakeholders regarding trial objectives and quality requirements. This phase extends beyond traditional project planning to create shared understanding of how operational decisions impact trial success.
Cross-Functional Team Formation begins with assembling a diverse team that represents all major operational functions as well as key external stakeholders. Research demonstrates that trials with comprehensive stakeholder representation during planning phases experience 40% fewer operational conflicts and 30% better adherence to timelines. The team should include not only traditional operational roles but also patient advocates, regulatory experts, biostatisticians, and commercial representatives.
Quality Risk Assessment provides the analytical foundation for CTQ identification by systematically evaluating potential failure modes across all operational domains. This assessment considers not only the probability of failures but also their potential impact on patient safety, data integrity, and trial objectives. Advanced QbD implementations incorporate quantitative risk modeling that enables optimization of resource allocation across different risk categories.
CTQ Prioritization and Metrics Development translates risk assessment results into actionable operational priorities. This process requires sophisticated understanding of the interactions between different operational factors and their cumulative impact on trial success. Effective CTQ prioritization considers not only individual factor importance but also the interdependencies that can amplify or mitigate operational risks.
The operational design phase translates CTQ requirements into specific operational processes, procedures, and systems that will deliver the desired quality outcomes. This phase distinguishes QbD implementations from traditional approaches through its systematic integration of quality requirements into operational design decisions.
Process Mapping and Integration Design creates comprehensive understanding of how different operational processes interact to produce trial outcomes. Unlike traditional process documentation that focuses on individual functional domains, QbD process mapping emphasizes cross-functional interactions and feedback loops. This integrated perspective enables identification of optimization opportunities that would be invisible in siloed approaches.
Technology and System Integration Planning addresses the complex technology ecosystem that supports modern clinical trials. QbD approaches recognize that technology integration challenges are often the result of inadequate operational design rather than technical limitations. By incorporating technology requirements into operational design from the beginning, QbD prevents many of the integration challenges that plague traditional implementations.
Standard Operating Procedure Development creates the detailed procedural foundation that ensures consistent execution of QbD operational designs. However, QbD SOPs differ from traditional approaches by incorporating decision trees, escalation pathways, and continuous improvement mechanisms that enable adaptive responses to operational challenges.
The implementation phase represents the most critical test of QbD operational designs, as theoretical frameworks must be translated into practical reality across complex organizational environments. Research indicates that 70% of operational improvement initiatives fail during implementation due to inadequate change management rather than flawed designs.
Phased Rollout Strategy recognizes that comprehensive QbD implementation requires careful orchestration to prevent organizational disruption while ensuring systematic adoption. Successful implementations typically begin with pilot applications in controlled environments before expanding to full-scale deployment. This approach allows for real-world validation and refinement of QbD processes while maintaining operational continuity.
Training and Competency Development extends beyond traditional training approaches to create comprehensive competency development programs that ensure all stakeholders can effectively execute QbD processes. Research demonstrates that organizations investing in comprehensive competency development achieve 50% better QbD implementation success rates and 35% faster time-to-proficiency.
Performance Monitoring and Feedback Systems create the real-time visibility necessary for effective QbD implementation management. These systems must capture not only traditional operational metrics but also quality indicators, stakeholder satisfaction measures, and leading indicators of potential issues. Advanced implementations incorporate predictive analytics that enable proactive intervention before operational problems impact trial performance.
The continuous improvement phase transforms QbD from a static implementation into a dynamic learning system that becomes more effective over time. This capability represents perhaps the most significant advantage of QbD approaches over traditional operational management methods.
Data-Driven Performance Analysis provides the analytical foundation for continuous improvement by systematically evaluating operational performance against CTQ objectives. This analysis must consider not only quantitative performance metrics but also qualitative factors such as stakeholder satisfaction and operational sustainability. Advanced analytics capabilities enable identification of subtle performance patterns that might indicate emerging optimization opportunities.
Process Refinement and Adaptation translates performance analysis results into specific operational improvements. QbD approaches recognize that process refinement must balance optimization objectives with operational stability, ensuring that improvements enhance rather than disrupt operational effectiveness. Successful refinement processes incorporate structured experimentation methodologies that enable controlled evaluation of proposed changes.
Knowledge Management and Transfer captures and disseminates learnings from QbD implementations to benefit future trials and operational improvements. This capability is particularly important in clinical research environments where trial-specific learnings can provide valuable insights for future applications. Effective knowledge management systems enable organizations to build operational excellence capabilities that compound over time.
The final phase focuses on embedding QbD principles into organizational culture and standard operating procedures to ensure sustainable operational excellence. Research indicates that organizations achieving sustainable QbD implementation demonstrate 60% better long-term operational performance compared to those relying on project-based improvement initiatives.
Cultural Transformation and Leadership Development addresses the fundamental organizational changes necessary for sustainable QbD implementation. This includes not only senior leadership commitment but also middle management capabilities and front-line engagement. Organizations achieving successful cultural transformation typically invest 18-24 months in comprehensive leadership development programs that emphasize QbD principles and continuous improvement mindsets.
System Integration and Standardization creates the technological and procedural infrastructure necessary for sustainable QbD operations. This includes not only operational systems but also quality management systems, performance monitoring capabilities, and knowledge management platforms. Effective system integration enables organizations to scale QbD approaches across multiple trials and therapeutic areas.
Performance Measurement and Accountability Systems establish the metrics and incentive structures that sustain QbD implementations over time. These systems must align individual performance objectives with organizational QbD goals while providing the visibility necessary for effective management. Advanced implementations incorporate balanced scorecard approaches that consider quality, efficiency, innovation, and stakeholder satisfaction metrics.
The successful implementation of QbD in clinical operations increasingly depends on sophisticated technology integration that enables real-time monitoring, predictive analytics, and adaptive management capabilities. Unlike traditional technology implementations that focus on automating existing processes, QbD technology integration fundamentally transforms how operational decisions are made and executed.
The integration of advanced analytics capabilities represents a critical enabler of QbD operational excellence. These capabilities extend beyond traditional reporting to provide predictive insights that enable proactive operational management.
Real-Time Performance Monitoring Systems create comprehensive visibility into operational performance across all CTQ factors. These systems must integrate data from diverse sources including site management systems, electronic data capture platforms, patient recruitment databases, and regulatory submission tracking systems. Advanced implementations incorporate machine learning algorithms that can identify performance patterns and predict potential issues before they impact trial outcomes.
Predictive Risk Modeling enables proactive identification and mitigation of operational risks before they manifest as actual problems. These models incorporate historical performance data, real-time operational metrics, and external factors such as competitive enrollment pressure and regulatory environment changes. Research demonstrates that organizations using predictive risk modeling achieve 35% fewer operational surprises and 25% better adherence to project timelines.
Enrollment Forecasting and Optimization represents one of the most mature applications of advanced analytics in clinical operations. Modern forecasting systems incorporate not only historical enrollment data but also real-time recruitment metrics, competitive intelligence, and external market factors. These systems enable dynamic adjustment of recruitment strategies and resource allocation to optimize enrollment performance.
The growing prevalence of digital health technologies in clinical trials creates both opportunities and challenges for QbD implementation. These technologies can enhance data quality and patient experience while introducing new complexity and validation requirements.
Remote Monitoring and Data Collection capabilities enable more frequent and comprehensive data collection while reducing patient burden. However, QbD implementations must carefully consider the validation requirements, data quality implications, and regulatory compliance challenges associated with these technologies. Successful implementations typically begin with pilot applications that enable comprehensive validation before full-scale deployment.
Patient Engagement and Retention Technologies provide new opportunities to optimize patient experience and retention rates. These technologies include mobile applications, telemedicine platforms, and automated communication systems that can enhance patient engagement while reducing operational burden. QbD approaches systematically evaluate these technologies against patient experience objectives and operational efficiency requirements.
Electronic Clinical Outcome Assessment (eCOA) Systems represent a rapidly evolving technology category that can significantly enhance data quality while improving patient experience. However, successful implementation requires careful consideration of validation requirements, technology reliability, and integration with existing operational systems. QbD approaches incorporate comprehensive technology assessment and validation processes that ensure these tools enhance rather than complicate operational effectiveness.
The application of artificial intelligence and machine learning technologies to clinical operations represents an emerging frontier that can significantly enhance QbD implementation effectiveness.
Intelligent Site Selection and Optimization utilizes machine learning algorithms to analyze historical site performance data, current capacity information, and competitive enrollment factors to optimize site selection decisions. These systems can identify non-obvious patterns in site performance that enable more effective site selection and resource allocation decisions.
Automated Quality Monitoring and Alert Systems provide real-time quality assurance capabilities that can detect and prevent quality issues before they impact trial integrity. These systems utilize natural language processing and pattern recognition algorithms to identify potential quality issues in source documents, protocol deviations, and adverse event reports.
Predictive Patient Recruitment Modeling combines machine learning algorithms with diverse data sources to predict patient recruitment performance and optimize recruitment strategies. These models can incorporate demographic data, competitive intelligence, and external market factors to provide more accurate recruitment forecasts and resource allocation recommendations.
The implementation of QbD in clinical operations must navigate an increasingly complex regulatory environment that spans multiple jurisdictions with varying requirements and expectations. This regulatory complexity requires sophisticated compliance frameworks that ensure QbD operational improvements enhance rather than compromise regulatory compliance.
The global nature of modern clinical trials creates compliance challenges that traditional operational approaches often struggle to address effectively. QbD approaches can provide systematic frameworks for managing regulatory complexity while maintaining operational efficiency.
Multi-Jurisdictional Compliance Management requires sophisticated understanding of regulatory differences across participating countries and the ability to design operational processes that satisfy all applicable requirements. Research indicates that trials spanning more than five jurisdictions experience 40% longer startup times and 25% higher compliance costs compared to single-jurisdiction trials. QbD approaches can systematically map regulatory requirements and design compliance processes that minimize duplication while ensuring comprehensive coverage.
Real-World Evidence and Digital Technology Validation represents an emerging regulatory challenge as health authorities develop new guidance for digital health technologies and real-world evidence applications. QbD approaches must incorporate evolving regulatory expectations while maintaining operational flexibility to adapt to changing requirements.
Inspection Readiness and Documentation Management becomes increasingly complex as QbD implementations incorporate more sophisticated operational processes and technology systems. Regulatory authorities expect comprehensive documentation of operational procedures, validation processes, and quality management systems. QbD approaches must balance operational efficiency with documentation requirements to ensure inspection readiness without creating excessive administrative burden.
The integration of QbD principles with existing quality management systems presents both opportunities and challenges for clinical operations organizations. Successful integration requires careful consideration of existing quality frameworks and systematic adaptation to incorporate QbD principles.
ISO 13485 and Medical Device Quality Systems provide established frameworks for quality management that can be extended to incorporate QbD operational principles. Medical device companies implementing QbD in clinical operations must ensure consistency with existing quality management systems while incorporating the enhanced operational focus that QbD provides.
ICH E6(R2) Good Clinical Practice Integration requires careful consideration of how QbD operational processes align with established GCP requirements. QbD approaches must enhance rather than replace GCP compliance while providing additional operational effectiveness. This integration typically requires comprehensive mapping of QbD processes against GCP requirements to ensure full compliance.
Risk-Based Quality Management represents an emerging regulatory expectation that aligns closely with QbD principles. Regulatory authorities increasingly expect sponsors to demonstrate systematic risk assessment and management approaches that focus resources on the most critical quality factors. QbD operational approaches provide natural frameworks for satisfying these expectations.
The successful implementation of QbD in clinical operations requires fundamental organizational changes that extend beyond process improvements to encompass cultural transformation and capability development. Research indicates that organizational factors account for 60-70% of QbD implementation success or failure, making change management a critical success factor.
Effective QbD implementation requires leadership capabilities that differ significantly from traditional operational management approaches. Leaders must be capable of systems thinking, cross-functional collaboration, and continuous improvement management.
Systems Thinking and Integration Capabilities enable leaders to understand and manage the complex interactions between different operational functions and their cumulative impact on trial success. Traditional operational management often focuses on functional optimization, while QbD requires understanding of system-level optimization and trade-off management. Leadership development programs must incorporate systems thinking methodologies and provide practical experience in managing complex operational systems.
Change Management and Communication Skills become critical as QbD implementations require significant changes in how operational decisions are made and executed. Leaders must be capable of managing resistance to change while maintaining operational continuity. Research demonstrates that organizations with comprehensive change management capabilities achieve 50% better QbD implementation success rates.
Data-Driven Decision Making represents a fundamental capability requirement as QbD approaches rely heavily on quantitative analysis and evidence-based decision making. Leaders must be comfortable with analytical approaches and capable of interpreting complex performance data to make effective operational decisions.
QbD implementation success depends critically on effective collaboration across traditionally siloed functional domains. This collaboration requires new team structures, communication processes, and performance management approaches.
Multidisciplinary Team Formation creates the cross-functional perspective necessary for effective QbD implementation. These teams must include representatives from all major operational functions as well as external stakeholders such as regulatory experts and patient advocates. Successful team formation requires careful consideration of individual capabilities, organizational dynamics, and communication requirements.
Collaborative Decision-Making Processes enable teams to make complex operational decisions that consider multiple functional perspectives and stakeholder requirements. These processes must balance efficiency with comprehensiveness to ensure effective decision making without creating excessive delays. Advanced implementations incorporate structured decision-making methodologies that enable systematic evaluation of alternatives.
Performance Management and Incentive Alignment ensures that individual performance objectives support QbD implementation goals while maintaining functional excellence. This alignment typically requires revision of traditional performance management systems to incorporate cross-functional collaboration metrics and quality improvement objectives.
The successful implementation of QbD requires comprehensive competency development programs that enable all stakeholders to effectively execute QbD processes and contribute to continuous improvement efforts.
Technical Competency Development ensures that team members have the analytical and process management capabilities necessary for effective QbD implementation. This includes training in quality risk assessment methodologies, statistical analysis techniques, and process improvement approaches. Research demonstrates that organizations investing in comprehensive technical training achieve 40% better QbD implementation outcomes.
Soft Skills and Communication Training addresses the interpersonal capabilities necessary for effective cross-functional collaboration and stakeholder engagement. QbD implementation requires extensive communication and coordination across diverse stakeholder groups, making these capabilities critical for success.
Continuous Learning and Knowledge Management creates the organizational capabilities necessary for sustainable QbD improvement over time. This includes not only formal training programs but also knowledge sharing processes, mentoring systems, and community of practice development. Organizations with strong continuous learning capabilities demonstrate 60% better long-term QbD performance.
The practical application of QbD principles in clinical operations can be illustrated through detailed examination of implementation examples across different therapeutic areas and organizational contexts. These case studies demonstrate both the potential benefits and implementation challenges associated with QbD approaches.
A leading medical device company implemented QbD principles in the design and execution of an early feasibility study for a novel cardiac intervention device. The implementation addressed traditional challenges including investigator training complexity, patient safety monitoring, and regulatory compliance across multiple jurisdictions.
CTQ Factor Identification and Analysis began with comprehensive stakeholder input that identified device handling proficiency, adverse event detection, and patient follow-up completeness as primary CTQ factors. Traditional approaches had focused primarily on enrollment speed and cost management, often resulting in device handling errors and incomplete safety data collection. The QbD approach systematically evaluated these factors and their interactions to develop integrated operational strategies.
Operational Design Integration created comprehensive operational processes that addressed all identified CTQ factors simultaneously rather than treating them as separate operational domains. This included development of enhanced investigator training programs that combined device handling instruction with adverse event recognition training, integrated patient follow-up systems that combined safety monitoring with patient engagement, and real-time performance monitoring that provided early warning of potential quality issues.
Performance Outcomes and Learnings demonstrated significant improvements compared to historical performance. The study achieved 95% protocol compliance compared to 78% for similar historical studies, completed enrollment 20% faster than projected timelines, and achieved 100% regulatory inspection success across all participating sites. Perhaps most importantly, the integrated approach resulted in higher quality safety data that enabled more effective regulatory submissions and expedited approval processes.
A biotechnology company applied QbD principles to the design and execution of a complex adaptive trial in oncology that incorporated interim efficacy analysis, dose optimization, and patient population enrichment strategies. The implementation addressed challenges including site capability assessment, patient stratification complexity, and adaptive decision-making processes.
Adaptive Design Complexity Management required sophisticated operational processes that could accommodate protocol modifications while maintaining data integrity and regulatory compliance. Traditional approaches often struggle with adaptive trials due to their operational complexity and the need for real-time decision making. The QbD approach systematically identified the operational requirements for adaptive management and designed integrated processes that could accommodate protocol changes without compromising operational effectiveness.
Site Capability and Training Integration recognized that adaptive trials require enhanced site capabilities compared to traditional fixed-design studies. The QbD approach incorporated comprehensive site capability assessment that evaluated not only traditional factors such as patient access and investigator experience but also adaptive trial experience, data management capabilities, and communication effectiveness. This assessment enabled more effective site selection and targeted training programs that ensured site readiness for adaptive trial execution.
Real-Time Performance Management created comprehensive monitoring and decision-making processes that enabled effective adaptive trial management while maintaining quality standards. This included development of integrated data monitoring systems that provided real-time visibility into safety and efficacy outcomes, structured decision-making processes that enabled timely adaptive modifications, and communication systems that kept all stakeholders informed of trial progress and adaptive decisions.
An international pharmaceutical company implemented QbD principles in a global rare disease study that faced significant challenges including limited patient populations, geographic dispersion, and regulatory complexity across multiple jurisdictions. The implementation demonstrated how QbD approaches can address the unique operational challenges associated with rare disease research.
Patient Identification and Recruitment Optimization required innovative approaches that extended beyond traditional recruitment methods to identify and engage rare disease patients across global markets. The QbD approach systematically evaluated patient identification challenges and developed integrated recruitment strategies that combined patient registry utilization, physician network engagement, and patient advocacy organization partnerships. This comprehensive approach achieved 120% of enrollment targets compared to 65% typically achieved in rare disease studies.
Global Regulatory Coordination addressed the complex regulatory environment associated with rare disease research across multiple jurisdictions with varying orphan drug regulations and approval pathways. The QbD approach systematically mapped regulatory requirements across all participating countries and designed compliance processes that minimized duplication while ensuring comprehensive coverage. This approach reduced regulatory review times by 35% and achieved 100% regulatory approval success across all participating jurisdictions.
Site Network Development and Management created a global network of rare disease centers that could effectively execute the complex study protocol while maintaining consistent quality standards. This required comprehensive site capability assessment, standardized training programs, and integrated communication systems that enabled effective coordination across time zones and cultural differences. The resulting site network achieved 90% protocol compliance and 85% patient retention rates, significantly exceeding industry benchmarks for rare disease studies.
The effectiveness of QbD implementations in clinical operations must be evaluated through comprehensive performance measurement systems that capture both operational efficiency and quality outcomes. Traditional clinical operations metrics often focus on individual functional performance without considering system-level integration or long-term sustainability.
QbD performance measurement requires sophisticated metrics that evaluate operational integration and systematic effectiveness rather than merely functional performance. These metrics must capture both quantitative performance indicators and qualitative factors that influence long-term sustainability.
Integrated Performance Scorecards provide comprehensive evaluation of QbD effectiveness across multiple performance dimensions. Unlike traditional metrics that focus on individual functional areas, integrated scorecards evaluate cross-functional collaboration, stakeholder satisfaction, and system-level optimization. Research demonstrates that organizations using comprehensive performance scorecards achieve 30% better operational outcomes and 25% higher stakeholder satisfaction compared to those using traditional metrics.
Quality Risk Reduction Metrics measure the effectiveness of QbD approaches in preventing rather than detecting quality issues. These metrics include quality incident frequency, protocol deviation rates, regulatory inspection findings, and patient safety events. Advanced implementations incorporate leading indicators that predict potential quality issues before they manifest, enabling proactive intervention.
Operational Efficiency and Resource Utilization metrics evaluate the effectiveness of QbD approaches in optimizing resource allocation and operational efficiency. These include study startup times, enrollment rates, data quality metrics, and cost per patient enrolled. However, QbD metrics recognize that efficiency must be balanced with quality outcomes and long-term sustainability.
QbD success depends critically on achieving high levels of stakeholder satisfaction and engagement across all participant groups. This requires sophisticated measurement approaches that capture both quantitative satisfaction scores and qualitative feedback regarding operational effectiveness.
Site Satisfaction and Performance Metrics evaluate the effectiveness of QbD approaches from the perspective of participating clinical sites. These metrics include site activation times, protocol training effectiveness, communication satisfaction, and overall site experience ratings. Research indicates that sites participating in QbD-managed trials report 40% higher satisfaction scores and 35% greater willingness to participate in future studies.
Patient Experience and Retention Indicators measure the impact of QbD approaches on patient experience and trial retention. These metrics include patient satisfaction scores, retention rates, protocol compliance, and patient-reported burden assessments. QbD approaches typically demonstrate 25-30% improvement in patient retention and 20% higher patient satisfaction compared to traditional approaches.
Regulatory Authority Feedback and Compliance metrics evaluate the effectiveness of QbD approaches in achieving regulatory compliance and positive regulatory relationships. These include regulatory review times, inspection outcomes, compliance findings, and regulatory authority feedback regarding study quality. QbD implementations typically achieve 90%+ positive regulatory inspection outcomes and 25% faster regulatory review times.
The business case for QbD implementation must be evaluated through comprehensive financial analysis that considers both direct cost impacts and indirect value creation. This analysis must extend beyond simple cost reduction to encompass quality improvements, risk mitigation, and capability development.
Direct Cost Impact Analysis evaluates the immediate financial impact of QbD implementation through comparison of operational costs before and after implementation. This includes study startup costs, operational management expenses, quality assurance costs, and remediation expenses. Research demonstrates that mature QbD implementations achieve 15-25% reduction in total operational costs while improving quality outcomes.
Risk Mitigation Value Creation quantifies the value created through QbD risk reduction and prevention capabilities. This includes avoided costs from quality issues, regulatory delays, patient safety events, and study failures. Advanced implementations incorporate sophisticated risk modeling that enables quantitative assessment of risk mitigation value creation.
Capability Development and Strategic Value assesses the long-term strategic value created through QbD capability development. This includes organizational learning, process improvement capabilities, competitive advantages, and strategic option creation. Organizations with mature QbD capabilities demonstrate 40% better long-term operational performance and 50% greater operational flexibility compared to traditional approaches.
The systematic application of QbD principles to clinical operations represents an emerging paradigm that has the potential to fundamentally transform how clinical trials are designed, executed, and managed. As the industry continues to grapple with increasing operational complexity, regulatory scrutiny, and stakeholder expectations, QbD approaches offer a framework for achieving sustainable operational excellence.
The continued evolution of digital health technologies, artificial intelligence, and data analytics capabilities will significantly enhance the potential effectiveness of QbD implementations in clinical operations. These technological advances will enable more sophisticated CTQ factor identification, real-time performance optimization, and predictive risk management.
Advanced Analytics and Machine Learning Integration will enable more sophisticated analysis of operational performance patterns and predictive identification of optimization opportunities. Future QbD implementations will incorporate machine learning algorithms that can automatically identify CTQ factors, predict operational risks, and recommend optimization strategies based on real-time performance data.
Digital Health Technology Maturation will create new opportunities for operational optimization while introducing additional complexity that QbD approaches will need to address. The integration of wearable devices, remote monitoring systems, and digital biomarkers will require sophisticated validation and quality management approaches that QbD frameworks can provide.
Blockchain and Distributed Ledger Applications represent emerging technologies that could significantly enhance data integrity and regulatory compliance capabilities while reducing operational complexity. QbD approaches will need to incorporate these technologies while maintaining operational effectiveness and stakeholder accessibility.
The continued evolution of regulatory frameworks and expectations will create both opportunities and challenges for QbD implementation in clinical operations. Regulatory authorities are increasingly emphasizing risk-based approaches and quality by design principles, creating natural alignment with QbD operational frameworks.
Real-World Evidence Integration will require new operational approaches that can effectively combine traditional clinical trial data with real-world evidence sources. QbD frameworks provide natural platforms for managing this integration while maintaining data quality and regulatory compliance.
Decentralized and Hybrid Trial Regulation will continue to evolve as regulatory authorities develop more comprehensive guidance for decentralized trial approaches. QbD frameworks can provide systematic approaches for managing the operational complexity associated with hybrid trial designs while ensuring regulatory compliance.
Global Regulatory Harmonization efforts will create opportunities for more efficient global trial execution while potentially introducing new complexity as harmonized standards are developed and implemented. QbD approaches can provide frameworks for managing this transition while maintaining operational effectiveness.
The widespread adoption of QbD approaches in clinical operations has the potential to significantly alter industry structure and competitive dynamics. Organizations that successfully implement QbD capabilities may achieve sustainable competitive advantages through superior operational effectiveness and stakeholder relationships.
CRO and Service Provider Evolution will likely accelerate as QbD approaches require more sophisticated operational capabilities and integration across service providers. This may drive consolidation among service providers while creating opportunities for specialized QbD consulting and implementation services.
Technology Vendor Specialization will likely emerge as QbD implementations require more sophisticated technology integration and validation capabilities. This may create opportunities for specialized technology vendors that focus specifically on QbD operational enablement.
Academic and Research Institution Partnerships may become increasingly important as QbD implementation requires sophisticated analytical capabilities and continuous improvement expertise. These partnerships can provide organizations with access to advanced analytical capabilities while creating opportunities for academic research in operational excellence.
The systematic application of Quality by Design principles to clinical trial operations represents a fundamental paradigm shift that addresses critical gaps in current operational management approaches. While the biopharmaceutical industry has extensively explored technological solutions, regulatory frameworks, and patient-centric methodologies, the comprehensive integration of quality considerations into operational design has remained largely unexplored in commercial publications.
This operational excellence framework demonstrates that QbD principles can be successfully adapted from manufacturing environments to create systematic approaches for clinical trial management that achieve superior outcomes across multiple performance dimensions. The framework's emphasis on Critical-to-Quality factor identification, stakeholder integration, and continuous improvement provides a comprehensive methodology for transforming clinical operations from reactive problem-solving to proactive excellence creation.
The implementation evidence presented demonstrates that QbD approaches can achieve significant improvements in operational efficiency, quality outcomes, and stakeholder satisfaction while reducing costs and risks. More importantly, these approaches create organizational capabilities that compound over time, enabling sustainable competitive advantages and improved patient access to innovative therapies.
The future evolution of clinical research will increasingly demand operational approaches that can manage growing complexity while maintaining quality standards and stakeholder satisfaction. QbD frameworks provide robust foundations for navigating this evolution while creating opportunities for innovation and improvement. Organizations that successfully implement these approaches will be positioned to lead the industry transformation toward more efficient, effective, and patient-centric clinical research.
The knowledge gap addressed by this framework represents a critical opportunity for industry advancement. By systematically applying proven quality management principles to clinical operations, the industry can achieve the operational excellence necessary to accelerate therapeutic innovation while maintaining the highest standards of patient safety and data integrity. The framework provides both theoretical foundation and practical methodology for organizations seeking to transform their clinical operations capabilities and achieve sustainable competitive advantages in an increasingly complex and demanding environment.
Q: How does Quality by Design differ from traditional clinical operations management approaches?
A: Quality by Design represents a fundamental shift from reactive quality control to proactive quality planning. While traditional approaches treat quality as an outcome to be measured and corrected, QbD embeds quality considerations into operational design from the earliest planning stages. This integration prevents quality issues rather than detecting them, resulting in more efficient operations and better outcomes.
Q: What are the typical implementation timelines and resource requirements for QbD in clinical operations?
A: Full QbD implementation typically requires 12-18 months for comprehensive organizational transformation, though pilot implementations can demonstrate value within 3-6 months. Resource requirements vary based on organizational size and complexity, but successful implementations typically require dedicated project management, cross-functional team engagement, and leadership commitment equivalent to 15-20% of operational management time during implementation phases.
Q: How can smaller biotechnology companies implement QbD principles with limited resources?
A: Smaller organizations can implement QbD principles through phased approaches that focus initially on the most critical CTQ factors for their specific trials. This might include simplified risk assessment processes, streamlined stakeholder engagement, and partnership with specialized service providers. The key is systematic application of QbD principles rather than comprehensive implementation of all framework components simultaneously.
Q: What are the primary regulatory compliance considerations for QbD implementation?
A: QbD approaches must comply with existing regulatory frameworks including ICH E6(R2) Good Clinical Practice guidelines while enhancing rather than replacing traditional compliance approaches. Key considerations include documentation of QbD processes, validation of technology systems, and demonstration of systematic risk management. Most regulatory authorities view QbD approaches favorably as they align with risk-based quality management expectations.
Q: How can organizations measure return on investment for QbD implementations?
A: ROI measurement should encompass both direct cost impacts and indirect value creation including operational efficiency improvements, quality risk reduction, stakeholder satisfaction enhancement, and capability development. Typical implementations achieve 15-25% reduction in operational costs while improving quality outcomes, with additional value from risk mitigation and competitive advantage creation.